-
PDF
- Split View
-
Views
-
Cite
Cite
Vishnu R. Mani, Godwin Ofikwu, Ali Safavi, Surgical resection of a giant primary liposarcoma of the anterior mediastinum, Journal of Surgical Case Reports, Volume 2015, Issue 9, September 2015, rjv126, https://doi.org/10.1093/jscr/rjv126
Close - Share Icon Share
Abstract
This case describes the incidental finding and surgical removal of an 1.8-kg liposarcoma in the anterior mediastinum. These tumors are very rare and would normally present with symptoms of intrathoracic compression; however, this patient was completely asymptomatic. The case presentation and treatment rationale are described along with a brief review of existing literature.
INTRODUCTION
Liposarcomas are the second most common soft tissue sarcoma in adults after malignant fibrous histiocytoma, predominantly occurring in the lower extremity and the retroperitoneum. Primary mediastinal liposarcoma is a very rare variant of mediastinal neoplasms. It constitutes <1% of all mediastinal malignancies and 9% of all primary mediastinal sarcomas with scarce data in the literature to date [1, 2]. In this study, we present a case of primary liposarcoma of the anterior mediastinum abutting and compressing intrathoracic structures in a young female.
CASE REPORT
A 28-year-old asymptomatic obese female presented to the bariatric clinic for weight reduction surgery. During the routine bariatric preoperative evaluation, examination revealed decreased breath sounds bilaterally and dullness to percussion in the anterior chest. On X-ray, widening of the mediastinum with possible intrathoracic mass was identified and the patient was referred to thoracic surgery. Further laboratory investigation of common tumor markers, such as ABG, AFP, HCG, CA 19.9 and CEA, were all negative along with chemistry and hepatic panels. CT imaging was performed and revealed a large heterogeneous anterior mediastinal mass with fat and soft tissue. With possible differential including thymolipoma, liposarcoma and germ cell tumors, further imaging of the abdomen, brain and bones was performed and did not show any evidence of metastasis. CT-guided biopsy revealed a well-differentiated sclerosing variant liposarcoma with cellular-spindled areas. The cells were positive for CD34, desmin, S100 and MDM2. They were negative for SMA, CD117 and DOG1 (Figs 1–5).

Initial bariatric preoperative chest X-ray that led us to the diagnosis.


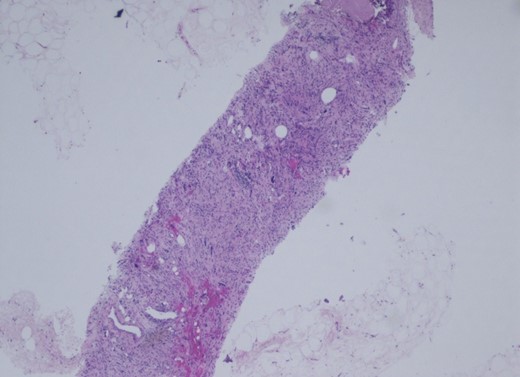
Mediastinal mass, core biopsy. The histology is that of a well-differentiated liposarcoma, sclerosing variant.
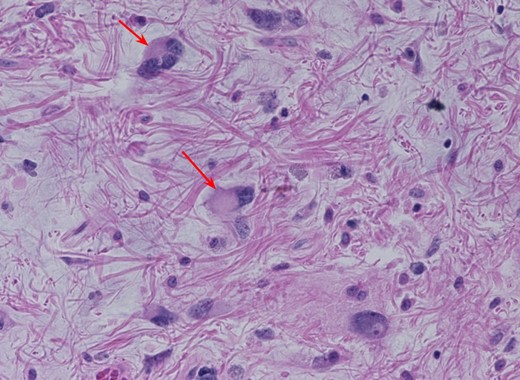
The tumor is composed of atypical spindle cells embedded in fibrous matrix. There are scattered tumor giant cells and rare lipoblasts, as well as numerous floret-like multinucleated giant cells (arrows). Importantly, silver and chromogenic in situ hybridization was performed for MDM2 and shows diffuse amplification.
The patient was taken electively for resection of the mass. The surgical approached was via a median sternotomy and the mass was resected without any complications from the anterior mediastinum and with an intact capsule. The smooth lobulated yellow-red mass weighed 1840 g, and measured 28.0 × 19.0 × 8.0 cm. The patient was discharged without any complications and has continued to follow up in clinic without any complaints.
DISCUSSION
Liposarcoma predominantly presents in the deep soft tissue of the limbs and the retroperitoneum. Although the overall anatomic distribution may be widespread, primary liposarcoma of intrathoracic origin is a very rare entity with few reported cases in the international literature [1]. Liposarcoma of the anterior mediastinum is even rarer as it is more commonly found in the posterior mediastinum [3]. Most of these masses are diagnosed incidentally or worked up secondary to compression symptoms from intrathoracic structures: dyspnea, tachypnea, wheezing, chest pain, SVC compression and voice hoarseness. These tumors are most commonly discovered during chest X-ray with a finding of widened mediastinum. On CT, a low attenuation signal between −50 and −150 HU is indicative of fatty tissue while greater signal intensity indicates soft tissue or tissue necrosis [4]. Of course, these indicators cannot be used as a diagnosis and differentials for such a mass must include thymolipoma, teratoma, germ cell tumor, lymphoma, herniated peritoneal fat and diaphragmatic hernia [5].
Mean age of diagnosis is 43 and it is very rarely documented in children and young adults [6]. These tumors are mesenchymal in origin, and the clinical course and outcome of liposarcoma largely depends on the histopathologic type of liposarcoma as they may be broadly classified into four histologic types: well-differentiated, dedifferentiated, myxoid and pleomorphic. In a 2014 retrospective study of 23 patients conducted in Shanghai, well-differentiated and atypical lipomatous variants carried the best prognosis while dedifferentiated and pleomorphic carried the worst [7]. They also found that radical surgery had a better overall survival rate compared with nonradical surgery. For patient receiving nonradical surgery, radiation and chemotherapy did not improve the prognosis or rate of relapse. Furthermore, there was no significant difference between overall survival and disease-free survival when comparing parameters such as tumor size, gender and age.
Based on the limited published data, surgical resection appears to be the best treatment modality and greatly increases the rate of disease-free and overall survival.
In difficult cases where complete resection is not possible or difficulty ensues in identifying the margin, en bloc debulking is the best option. Certain authors consider that huge masses require preoperative radiotherapy and chemotherapy before debulking surgery or as adjuncts, but they have shown to have low efficacy [8].
Recurrence within 6 months is common in deep-seated liposarcomas, but may take as long as 5–10 years after the initial excision [8]. Recurrence is related to the incomplete excision and the amount of tumor tissue left behind at the time of surgery. For difficult resections where the boundary of the tumor tissue is hard to delineate, the risk of incomplete excision is very high. In these cases, follow-up examinations should be held very frequently.
This case describes a young female who was incidentally identified with an anterior mediastinal mass and was promptly treated with radical surgery. Eighteen months later, there has been no sign of recurrence; however, the patient will be closely followed for the next year and there on. Although this case was made easier due to the fact that the tumor had a well-differentiated capsule, radical surgery appears to be the best option for all anterior mediastinal tumors.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
Histopathology slides were provided by Dr Marina Landa.



