-
PDF
- Split View
-
Views
-
Cite
Cite
Mike JR Kent, Claire Harding, Sean Walsh, Soft tissue ‘mallet’ injury to the hallux, Journal of Surgical Case Reports, Volume 2015, Issue 5, May 2015, rjv049, https://doi.org/10.1093/jscr/rjv049
Close - Share Icon Share
Abstract
We describe a case of a delayed presentation of a traumatic soft tissue mallet injury to the distal phalanx of the hallux in a teenager. Reports of this rare injury are sparse and there is no consensus in their treatment. This injury was treated with open repair of the tendon using a Mitek suture anchor, and stabilization with a 1.2-mm K-wire and extension splinting for 8 weeks. Following this treatment, she regained full power and a range of movement compared with the contralateral side, and achieved full function. We advocate surgical reconstruction of these injuries with suture anchors and stabilization of the interphalangeal joint.
INTRODUCTION
The ‘stubbed toe’ is a common innocuous injury, usually sustained barefoot, which can result in a wide range of injuries including nail bed lacerations, fractures of the distal phalanx and, uncommonly, bony or soft tissue mallet injuries. The mainstay of management of simple fractures and nail bed injuries is usually non-operative, with good long-term function and little or no morbidity [1].
Mallet fingers are common injuries with well-established treatments depending on the presence or absence of a fracture or joint subluxation [2]. However, similar injuries to the hallux are rare with only a handful of single case report in the literature [3–7]. The rarity of these injuries likely relates to the relative sizes of the digits and tendons and the protection offered by footwear. There is often a delay in presentation as in this case. Owing to their relative rarity, there is no consensus as to the optimum treatment which ranged from non-operative treatment in a rigid soled shoe, closed reduction and stabilization with Kirschner wires or open repair and reattachment of the tendon with suture anchors. Failure to recognize and treat these injuries can lead to extensor lag of the hallux, which carries some morbidity.
CASE REPORT
A 13-year-old girl injured her left great toe while running downstairs barefoot, incurring a forced plantar flexion injury. There was pain, swelling and bruising to the hallux, but she was able to weight bear. She noted a progressive drooping of the hallux over the following 3 weeks and presented to the trauma clinic via her GP.
On examination, she had a swelling overlying the interphalangeal joint (IPJ) of the hallux, which was held in 20° of plantar flexion, and she was unable to actively dorsiflex at the IPJ. There was full power of dorsiflexion at the metatarsophalangeal joint (MTPJ). The toenail was intact.
Plain radiographs showed no bony injuries, but the IPJ was subluxed in a plantar-flexed position (Fig. 1). An urgent ultrasound scan confirmed a full thickness rupture of the extensor hallucis longus (EHL) tendon at its insertion into the distal phalanx and evidence of a healing tear to the dorsal joint capsule (Fig. 2).

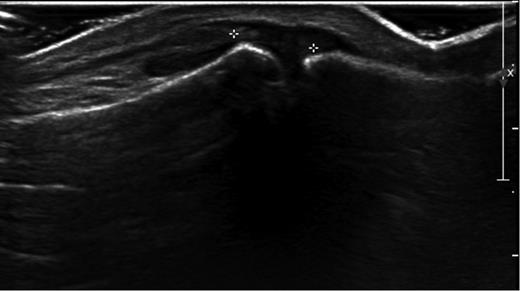
Ultrasound image showing ruptured IPJ capsule and avulsed EHL tendon.
Under general anaesthesia, an L-shaped incision was made to avoid the dorsomedial sensory nerve and avoid injury to the germinal matrix of the nail. The EHL tendon was found to be completely ruptured from the distal phalanx and had retracted back towards the MTPJ. The tendon end was debrided back to healthy tissue and was secured back to the distal phalanx using a Mitek anchor and a non-absorbable suture in a modified Krakow technique. The IPJ was stabilized with a 1.2-mm Kirschner wire (Figs 3–5).
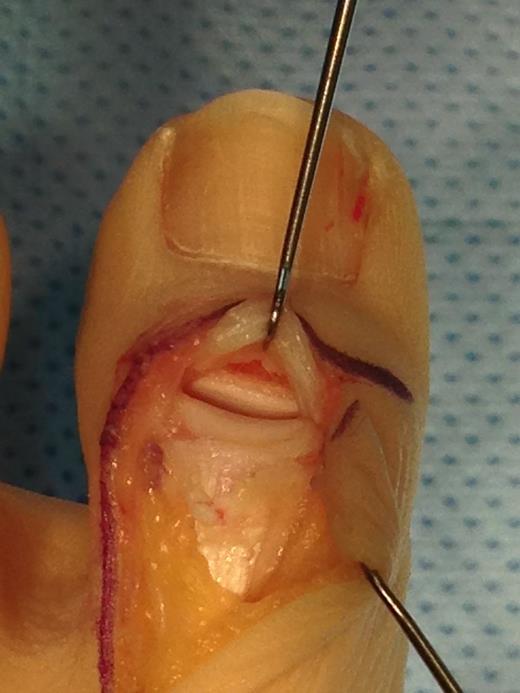
Operative photograph showing ruptured EHL tendon and avulsed IPJ capsule.
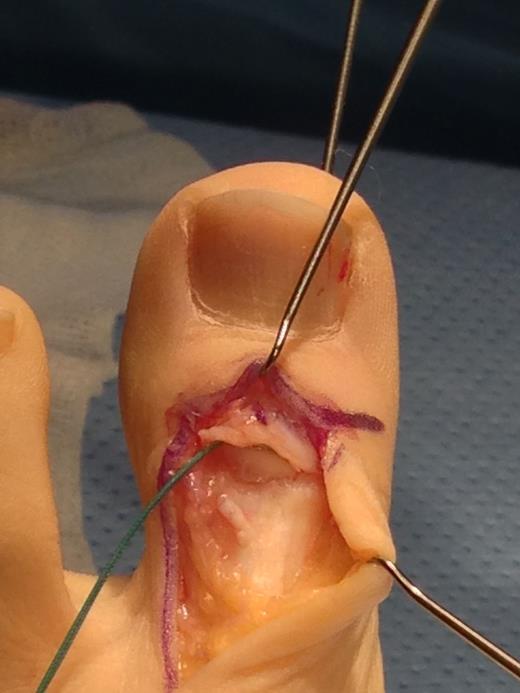
Operative photograph showing transfixion of the IPJ with a K-wire and insertion of a Mitek anchor into the distal phalanx.

She was allowed to heel weight bear. The K-wire was removed 4 weeks postoperatively and she was placed into a thermoplastic extension splint for a further 4 weeks, allowed to weight bear normally in shoes and undertake a passive range of movement exercises with physiotherapy. At this stage, she had good power of dorsiflexion, but limited plantar flexion due to stiffness.
At the point of discharge, 6 months following surgery, she had regained a full range of movement compared with the contralateral side, full power of plantar flexion and dorsiflexion, and had returned to normal function.
DISCUSSION
The earliest reports of ‘Mallet Hallux’ by Rapoff in 1999 and Saxby et al in 2001 advocated non-operative treatment with a rigid soled shoe and an extension splint, respectively [3, 7]. These cases were both middle-aged patients who had sustained bony mallet injuries and following treatment had stiff IPJs, but were asymptomatic with good function.
More recently, four further reports advocate surgical management akin to the management of mallet finger injuries. Three of these reports describe temporary stabilization with K-wires (either to reduce and stabilize fracture fragments directly or to act as blocking wires) [5, 6, 8]. In all of these cases, a K-wire was used to transfix the IPJ. All report bony union within 5–8 weeks and full function at final follow-up. However, only one of these patients (who was 16 years old) regained a full range of movement.
Hong and Tan were the first to report two cases of open reconstruction of ‘Mallet Hallux’ using bio-absorbable suture anchors and non-absorbable sutures, in combination with early mobilization of the joint [4]. They were concerned that popular K-wire transfixion was associated with a high degree of stiffness and the possibility of infection and wire breakage. They showed that with this combination of treatment, both of their patients were able to get back to full function relatively sooner with no stiffness of the joint.
This more involved treatment using suture anchors is perhaps more practical in ‘Hallux Mallet’ as the EHL tendon is larger than the extensor tendons involved in soft tissue mallet injuries of the fingers, meaning that the repair is of better quality.
In our reported case, due to the chronicity of the rupture (nearly 4 weeks at the time of surgery) and degree of retraction of the EHL tendon, it was felt that the patient would benefit from the combined treatment with a suture anchor and K-wire transfixion.
Following this combination of treatment, the patient has made a full functional recovery and achieved a full range of movement. We feel that this reflects the strength of the reconstruction and relative protection that the K-wire affords in addition to a suture anchor, with relatively early (4 weeks) passive movement. Additionally, the only other patient to achieve a full range of movement following treatment was also a teenager (despite having IPJ transfixion), suggesting that, as with most injuries, the virtues of youth enable better recovery.
Unstable bony and soft tissue mallet injuries of the hallux are uncommon. In this more chronic case in a younger patient with significant retraction of the tendon, we advocate open reconstruction with combined suture anchor repair and K-wire transfixion, with a return to normal functional outcomes and a range of movement.
CONFLICT OF INTEREST STATEMENT
None declared.



