-
PDF
- Split View
-
Views
-
Cite
Cite
J.J. van den Broek, M.M. Poelman, B.M. Wiarda, H.J. Bonjer, A.P.J. Houdijk, Extensive cervicomediastinal hematoma due to spontaneous hemorrhage of a parathyroid adenoma: a case report, Journal of Surgical Case Reports, Volume 2015, Issue 5, May 2015, rjv039, https://doi.org/10.1093/jscr/rjv039
Close - Share Icon Share
Abstract
Spontaneous extracapsular hemorrhage is a rare but potentially life-threatening manifestation of parathyroid gland adenomas. We present a case demonstrating that even in a patient with increased bleeding tendency due to anticoagulants, combined with compression of trachea and esophagus, conservative treatment can be successful.
INTRODUCTION
Parathyroid adenomas autonomously release parathyroid hormone (PTH) resulting in stimulation of bone resorption, reduction in renal calcium clearance and increased intestinal calcium absorption. The most common clinical presentation of parathyroid adenomas is asymptomatic hypercalcemia detected by routine biochemical screening [1]. Some patients present with easy fatigue, constipation, kidney stones, overt bone disease or proximal neuromuscular weakness [1, 2]. Spontaneous extracapsular hemorrhage of a parathyroid adenoma causing a cervicomediastinal hematoma is an uncommon but potentially life-threatening manifestation. This can be associated with ‘mass’ symptoms such as dysphagia and dyspnea, ultimately resulting in an endangered airway [3]. Only very few cases of spontaneous hemorrhage of parathyroid adenomas have been reported in the literature [4]. Although some authors state that acute surgical intervention in case of airway compromise is inevitable, we will present a case in which conservative treatment was successful.
CASE REPORT
A 79-year-old woman presented at the emergency department with pain during swallowing. Her past medical history included atrial fibrillation for which she had been receiving oral anticoagulants (Acenocoumarol). Three weeks earlier during routine laboratory investigation, an elevated serum calcium level was found. Urinary calcium excretion was 312 mg/24 h, ruling out familial hypocalciuric hypercalcemia. Further investigation with ultrasound, scintigraphy and SPECT scan had revealed a right-sided enlarged parathyroid gland (Fig. 1). Calcimimetic therapy [Cinacalcet (Mimpara®) 30 mg twice daily] had been initiated and surgical extirpation was scheduled.
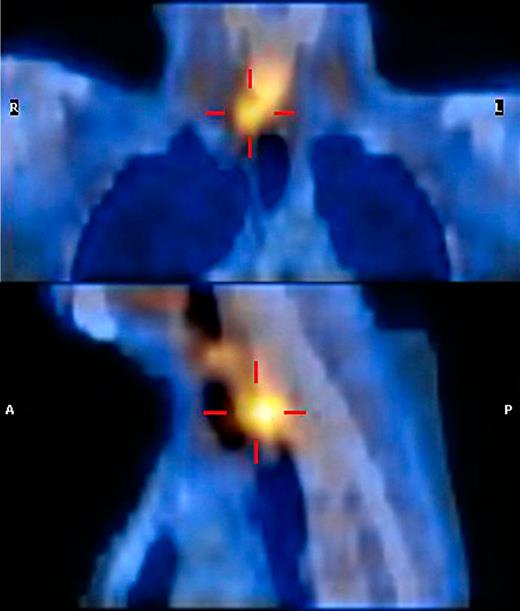
SPECT scan demonstrating a right-sided parathyroid gland adenoma.
At the time of presentation, the patient experienced swallowing difficulties, globus sensation and malaise since 3 days with reduced oral intake. Progressive pain and mild dyspnea were present since 1 day. Physical examination revealed a subtle inspiratory stridor, the anterior lower neck was tender at palpation, but no evident ecchymosis or mass was found and signs of infection were absent. Laboratory data demonstrated an elevated prothrombin time—International Normalized Ratio of 9.49, an elevated PTH level (8.9 pmol/l, normal range 0.7–4.4 pmol/l) and a normalized calcium level (2.28 mmol/l, normal range 2.10–2.55 mmol/l) as a result of the calcimimetic drug therapy. An ultrasound study of the neck revealed a low-density mass dorsal of the right thyroid lobe possibly extending intrathoracically. Subsequent magnetic resonance imaging (MRI) showed an elongated retropharyngeal mass expanding from the second cervical vertebra into the posterior mediastinum with compression of the trachea and esophagus (Fig. 2).
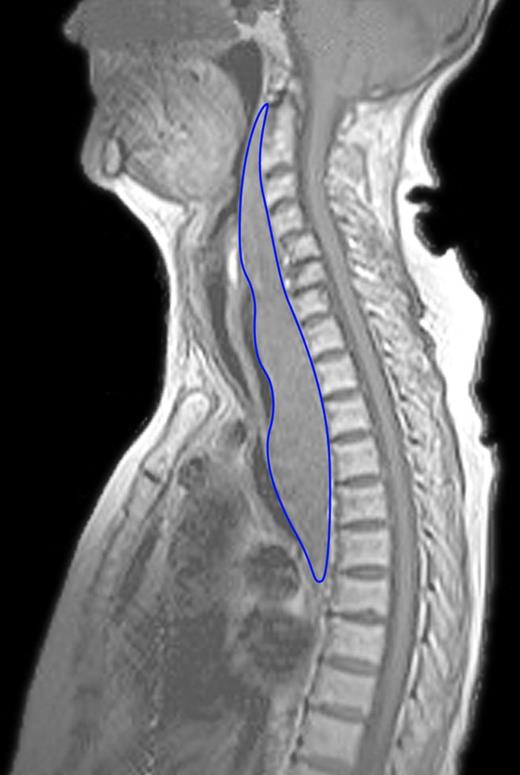
MRI showing the elongated retropharyngeal mass anteriorly of the spine, compressing the trachea and esophagus. The mass starts at the level of the second cervical vertebra and expands into the posterior mediastinum until the level of the seventh thoracic vertebra. Length of the hematoma is 200 mm with an anterior–posterior diameter of 33 mm. Compression of the trachea to a minimal diameter of 3 mm.
Bleeding of the parathyroid gland adenoma aggravated by the overdose of anticoagulants was suspected. The patient was admitted to the intensive care unit and endotracheal intubation was performed to secure the airway. Acenocoumarol was stopped and antagonized by vitamin K. Laryngoscopy and bronchoscopy revealed compression of both the trachea and esophagus with a subglottic stenosis of the trachea. Conservative treatment was chosen over surgical exploration. The patient was extubated successfully after 2 days without experiencing dyspnea.
After this event, calcimimetic drug therapy was continued, and blood calcium and PTH levels remained within the normal range. Hence, autoparathyroidectomy was suspected and surgery was cancelled. After 4 months, however, calcium and PTH levels increased again. On parathyroid scintigraphy and SPECT scan, a small area at the right lower thyroid lobe showed increased activity, again suspicious for a parathyroid adenoma. Since the patient experienced symptoms of hypercalcemia, surgery was scheduled. Identification of the adenoma was difficult due to adhesions; therefore, a resection of the right lower thyroid lobe was performed successfully. Postoperatively, serum calcium and PTH levels returned to normal (PTH 2.1 pmol/l and Ca2+ 2.46 mmol/l), and after 24 months of follow-up these levels were still within the normal range.
DISCUSSION
Spontaneous hemorrhage is a rare but potentially life-threatening manifestation of parathyroid gland adenomas [5, 6]. The etiology of this non-traumatic bleeding is unknown. A lack of balance between cell growth and blood supply leaving the adenoma susceptible for necrosis and bleeding has been suggested. This mechanism is believed to be similar to the apoplexy observed in other endocrine neoplasia [5, 7]. The hemorrhage may remain intracapsular or expand outside the thin capsula dissecting into cervical tissues or even into the mediastinum [8].
Signs and symptoms of extracapsular hemorrhage can involve cervicothoracic pain, dysphonia, dysphagia, dyspnea, cervicothoracic ecchymosis and a palpable cervical mass [4]. Nonspecific signs of hypercalcemia can accompany this. It can present similar to conditions such as subacute thyroiditis, cervical abscesses or thyroid lesions. The mediastinal symptoms may even mimic a dissecting aortic aneurysm or a bleeding thymic tumor [4]. Owing to the latency of most symptoms, misdiagnosis might be possible. Coexistence of elevated calcium or PTH levels could raise the suspicion, but further imaging techniques such as ultrasonography, CT or MRI are required to confirm the diagnosis.
In case of hypovolemic shock, superior vena cava obstruction syndrome or airway compromise, emergency surgery has to be considered [4]. Sometimes, even a thoracotomy has to be undertaken for evacuation of the hematoma [9]. However, in most cases with moderate cervical or cervicomediastinal hematoma, acute surgical exploration is not necessary. Our case demonstrates that even in a patient with compression of trachea and esophagus, conservative treatment can be successful. Endotracheal intubation can be used to bridge the acute phase. Acute surgical exploration is not without risk. It can be associated with damage to surrounding cervical structures or postoperative infection. Some might argue that acute surgical intervention enables the possibility of extirpating the adenoma and thereby treating the underlying problem of hyperparathyroidism at the same time. The hematoma, however, disturbs the normal anatomy making it more difficult to identify the parathyroid adenoma and increases the risk of surgical complications. Another argument advocating against extirpation of the parathyroid adenoma in the acute phase is the phenomenon of autoparathyroidectomy. Spontaneous parathyroid hemorrhage can induce remission of primary hyperparathyroidism. It can cause temporary remittance and sometimes even permanent control of hyperparathyroidism and its metabolic derangements [10]. If hyperparathyroidism persists, delayed parathyroidectomy can be scheduled after resorption of the hematoma. A minimum delay of 3 months has been proposed by Chaffanjon et al. [4] in order to facilitate successful surgical treatment.
In conclusion, hemorrhage from a parathyroid adenoma is a rare phenomenon, but it has to be considered in patients with non-traumatic neck emergencies. The coexistence of hypercalcemia with ‘mass’ symptoms such as neck swelling, dysphagia and/or dyspnea should point to the clinical hypothesis. The use of anticoagulants is considered to be a risk factor. This case also demonstrates that conservative treatment of the hemorrhage can be safe, even with moderate compression of the trachea and esophagus.
CONFLICT OF INTEREST STATEMENT
None declared.



