-
PDF
- Split View
-
Views
-
Cite
Cite
Michael Hughes, Jesper Roos, Multiple vascular and enteric fistulas into an anal pouch, Journal of Surgical Case Reports, Volume 2015, Issue 2, February 2015, rju157, https://doi.org/10.1093/jscr/rju157
Close - Share Icon Share
Abstract
We present a case of an 87-year-old female who presented 3 months following an emergency Hartmann's procedure for perforated diverticulum with per rectum bleed. She was found to have a false aneurysm in the iliac artery communicating with her rectal stump. This was treated successfully with intravascular coiling; however, she re-presented 2 years later complaining of passing stool per rectum and decreased colostomy output. She was found to have communication between two enterorectal fistulae with the distal segment of the remaining bowel.
INTRODUCTION
Enterocutaneous fistula formation following bowel resection is not uncommon; however, fistula formation between the bowel and remaining rectal stump is rarely reported. In addition, the occurrence of a fistula between a false aneurysm and a rectal stump is similarly a rare phenomenon.
CASE REPORT
An 84-year-old female was admitted to the hospital from the clinic complaining of dysuria and increased urinary frequency following an emergency laparotomy and Hartmann's procedure for a perforated diverticulum 3 months previously.
Her initial postoperative recovery was complicated by a pelvic collection and the development of hydronephrosis of the left kidney. Unfortunately, 2 days prior to her clinic appointment, she was found to have a bilateral femoral deep vein thrombosis for which she was commenced on warfarin.
After 2 days of treatment for a urinary tract infection and continuation of her warfarin, the patient complained of large fresh rectal bleed and haematuria. Her INR was found to be high; thus, warfarin was withheld and reversed with vitamin K, and instead an inferior vena cava filter was inserted. The patient continued to bleed, requiring blood transfusion to achieve haemodynamic stability.
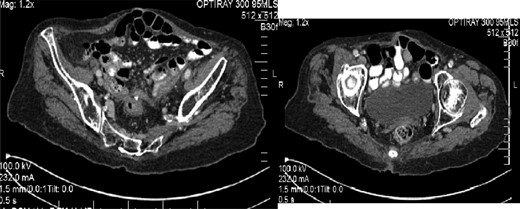
A CT angiogram was arranged which identified a large false aneurysm of the left internal iliac artery (Fig. 1) with probable communication to the rectal stump and the left ureter. The patient was transferred to the local vascular centre for endovascular coiling, which was successful.
Following discharge, the patient re-presented to the clinic 2 years later complaining of increasing discharge from her rectal stump with a simultaneous decrease in colostomy output. A sigmoidoscopy demonstrated two fistulae within the rectal stump, and a CT confirmed a communication between the stump and proximal small bowel (Fig. 2). She has elected for conservative management of her condition.
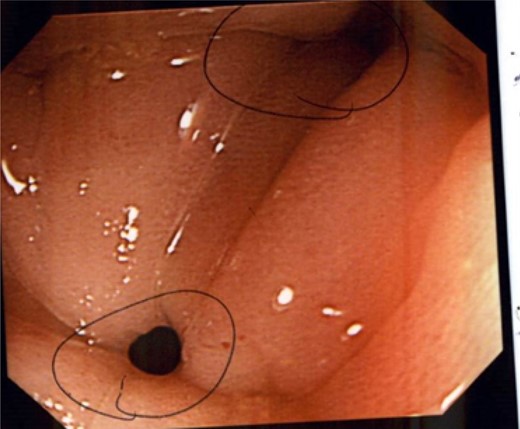
Colonoscopy demonstrating several fistulae into the anal pouch.
DISCUSSION
The formation of a ureteric-arterio-enteric fistula is extremely rare and when reported has a poor prognosis [1]. A similar case to the above was treated with open surgery and ligation of the iliac artery requiring a bypass graft [2], which despite a prolonged recovery period resulted in discharge from the hospital with no vascular sequelae.
Enterocutaneous fistulae are associated with considerable morbidity and mortality with some papers suggesting a mortality of 6–33% from complications such as sepsis [3]; however, enterocolonic fistulae are less well known.
Enterocolonic fistulae have been reported as a complication of Crohn's disease and diverticulitis. Less commonly cases have been reported following radiotherapy, lymphoma and localized trauma; however, few follow surgical intervention [4, 5]. Without intervention, mortality rates as high as 15–25% have been reported [6].
There have been very few reported cases of fistula formation between small bowel and a rectal stump following a Hartmann's procedure. One case reported in Japan following resection of adenocarcinoma of the bowel was treated surgically and found to be a recurrence [7].
The evidence for conservative versus surgical treatment for complex fistulation is sparse. One paper reported a 30% spontaneous closure rate of small bowel fistula's following a 4-week period of total parenteral nutrition and ‘bowel rest’ advocating surgical management if unsuccessful; however, this included few enterocolonic fistulae.
In the present case, it seems that pelvic sepsis and inflammation led to both the formation of a false aneurysm and anenterocolonic fistulae. This patient's residual symptoms are occasionally faecal incontinence and decreased stoma output, both of which she can manage. While the overall prognosis remains poor in such circumstances, successful conservative management is possible.
CONFLICT OF INTEREST STATEMENT
None declared.



