-
PDF
- Split View
-
Views
-
Cite
Cite
Nabil S. El-Masry, Ruben Geevarghese, Large bowel obstruction secondary to adhesive bands, Journal of Surgical Case Reports, Volume 2015, Issue 2, February 2015, rju152, https://doi.org/10.1093/jscr/rju152
Close - Share Icon Share
Abstract
Large bowel obstruction (LBO) is most commonly due to malignancy, volvulus, hernia, diverticular disease and inflammatory bowel disease. LBO due to adhesions is unusual. A literature review was conducted which revealed that only a few such cases have been reported. We report two cases of LBO secondary to adhesions in patients, one with and one without a past abdominal surgical history. We highlight that while rare, the aetiology of LBO secondary to adhesions must be considered in the differential diagnosis in patients presenting with obstructive symptoms.
INTRODUCTION
The most common causes of large bowel obstruction (LBO) are colonic neoplasm, volvulus, hernia, diverticular disease and inflammatory bowel disease. Adhesions secondary to previous inflammation or operation commonly cause small bowel obstruction, but are a rare cause of LBO. We report two cases of LBO secondary to adhesions.
CASE REPORT
Case 1
A 58-year-old man presented with sudden onset of right-sided colicky abdominal pain associated with nausea and vomiting. He had not opened his bowel for 4 days. He had three similar episodes of pain during the previous 3 weeks with two hospital admissions. The last admission was 4 days before, and he was in the hospital for 3 days and discharged home after he ‘opened’ his bowel. He reported no change in his bowel habits or bleeding per rectum. His appetite was poor. He had no urinary or other symptoms.
His past medical history (PMH) included gall stone pancreatitis 10 years ago and laparoscopic cholecystectomy subsequently. On examination, he was afebrile and haemodynamically stable. The abdomen showed fullness with mild tenderness in the right iliac fossa (RIF). Digital rectal examination (DRE) revealed an empty rectum.
Haemoglobin was 14.9 g/dl and the white cell count (WCC) was 9 × 109/l. Other remarkable laboratory tests included a C-reactive protein (CRP) of 15 mg/l. Urinalysis was normal. The plain X-ray abdomen (AXR) (Fig. 1) revealed dilatation of a focal segment of large bowel with mildly dilated small bowel. Computed tomography (CT scan) of his abdomen reported that the gas-filled viscus is likely to represent the caecum (Fig. 2).

Plain AXR (Case 1) revealed dilatation of a focal segment of a large bowel with a mildly dilated small bowel.
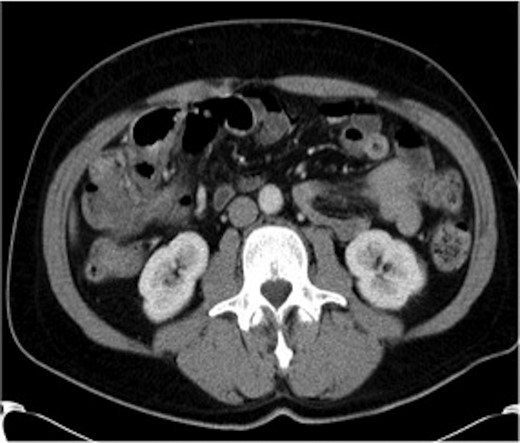
CT of the abdomen (Case 1) demonstrating the gas-filled caecum.
A presumptive diagnosis of caecal volvulus was made and the patient was taken to theatre. Laparotomy revealed an omental band wrapping the colon at the junction between the caecum and the ascending colon with a marked dilatation of the caecum. The caecum was viable and the appendix was normal. The rest of the large bowel and small bowel were normal. The band was dissected free off the colon and excised. Appendicectomy was performed and the gas in the caecum was aspirated via the appendicular stump prior to its ligation.
Case 2
A 46-year-old woman presented with a 5-day history of absolute constipation, abdominal distension, discomfort and an episode of vomiting. There was no change in her bowel habit and she had no other systemic symptoms. She had a PMH of a right-sided ovarian cyst detected on an ultrasound that she had for lower abdominal pain sometimes ago. She had no previous abdominal surgery. On examination, she was afebrile and haemodynamically stable. The abdomen was distended with mild tenderness in the RIF. DRE revealed an empty rectum.
Haemoglobin was 12.6 g/dl and a WCC of 8.3 × 109/l. Other remarkable laboratory tests included a CRP of 19 mg/l. Urinalysis was normal. The AXR revealed a grossly distended large bowel. A CT scan of the abdomen revealed that the rectum, sigmoid and descending colon were collapsed with an apparent calibre change within the transverse colon with no mass lesion (Fig. 3).

CT of the abdomen (Case 2) showing a calibre change within the transverse colon with no mass lesion.
A gastrografin enema (Fig. 4) failed to demonstrate any flow beyond the mid-transverse colon. A presumptive diagnosis of transverse colon obstruction was made and the patient was taken to theatre.
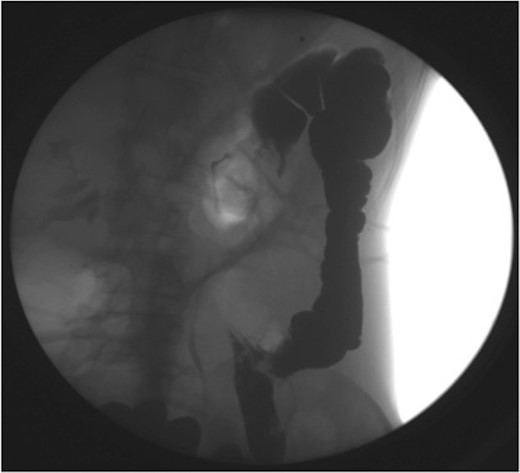
Gastrografin enema (Case 2) demonstrating no flow beyond the mid-transverse colon.
Laparotomy revealed an adhesive band extending from the gastrocolic omentum to the right fallopian tube causing a closed-loop obstruction of right half of transverse colon, ascending colon and terminal 5 cm of ileum. The band was divided. The bowel was viable. Appendicectomy was performed and most of the gas in the colon was aspirated via the appendicular stump prior to its ligation.
DISCUSSION
Colonic obstruction is most commonly attributed to a neoplasm or volvulus. Other aetiologies include incarcerated hernias, inflammatory bowel disease, diverticular disease, ischaemic stricture, intussusception and faecal impaction.
Adhesions, which are fibrous bands between two or more adjacent anatomic structures, are a common cause of small bowel obstruction but a very rare cause of large bowel obstruction [1–6]. The origin of these adhesions can be congenital [1, 2], inflammatory, post-traumatic or iatrogenic following previous surgery [3, 4].
The aetiology of the bands causing colonic obstruction in our cases was obscure, but may be related to a previous intraperitoneal inflammatory process with gall stone pancreatitis and laparoscopic cholecystectomy in Case 1. Interestingly, Case 2 had no previous abdominal surgery or any evidence of intraperitoneal inflammatory process. However, unnoticed right-sided salpingitis might have triggered the formation of this band.
In the absence of either surgery or abnormal fixation of the colon, adhesive obstruction may be secondary to inflammation of epiploic appendage. In these patients, the inflamed epiploic appendage that has become adherent to the abdominal wall or another intra-abdominal structure constricts the colon directly or forms a band entrapping the small bowel. The sigmoid colon is the most common site for a diseased epiploic appendage, accounting for 50% of patients [7].
Other unusual entities causing adhesive colon obstruction include remnants of embryological structures such as vitello-umbilical cord [8] and mesourachus [9]. A vitello-umbilical cord connects the tip of Meckel's diverticulum to the abdominal wall at the umbilicus, obstructing the middle portion of the redundant transverse colon or long sigmoid colon [8]. The mesourachus was bound by adhesions to small bowel mesentery and resulted in severe obstruction of the sigmoid colon, simulating a volvulus [9]. Anatomical and histopathological studies of the bands distinguish between embryonic remnants and aberrant mesenteric bands [8, 9].
On barium enema, adhesions cause a sharp, localized, circumferential narrowing of the large bowel. Occasionally, an area of circular muscular contraction may suggest this appearance. There are some areas of narrowness or focal contraction in the colon that are inconstantly seen radiologically. These contraction rings or colonic valves rarely persist during an entire barium enema, while compression from adhesions does [10].
Clinical features and findings of a combination of radiology investigations are important in timely decision-making surgery in patients with an adhesive band causing colonic obstruction. However, it is still difficult to make a preoperative diagnosis of adhesive colonic obstruction. Surgical intervention is mandatory in these patients for definitive diagnosis and treatment.
CONFLICT OF INTEREST STATEMENT
None declared.



