-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed H. Alattas, Ronald Dimentberg, Multiple fractures in a 22-year-old man after a simple fall, Journal of Surgical Case Reports, Volume 2015, Issue 10, October 2015, rjv117, https://doi.org/10.1093/jscr/rjv117
Close - Share Icon Share
Abstract
We present the case of a 22-year-old male with longstanding progressive fatigue, weakness and pain around his hips due to an undiagnosed parathyroid adenoma. The resultant primary hyperparathyroidism ultimately caused pathologic fractures. He was admitted to the hospital for further assessment and excision of the parathyroid adenoma. A few days after admission, he fell down while walking and was referred to our team. X-rays showed a displaced left femoral neck fracture (FNF) and right humeral shaft fracture with poor bone quality. His humeral fracture was treated conservatively, and the FNF was treated with total hip replacement. Three days later, he underwent parathyroidectomy. This case demonstrates the importance of a thorough investigation of progressive weakness even in a young individual and illustrates the importance of early diagnosis of parathyroid adenoma to avoid the devastating end results of this condition.
INTRODUCTION
Hyperparathyroidism (HPT) occurs when there is an abnormal increase in parathyroid hormone (PTH) production by the parathyroid gland [1–3]. The function of PTH is to elevate the blood calcium level. HPT may exist in a primary, secondary or tertiary form [4]. Primary HPT (PHPT) is caused by parathyroid adenomas in 85% of cases, leading to hyperplasia and over-secretion of PTH [2]. In most individuals in western society, it is diagnosed at an asymptomatic stage, without signs or symptoms of (PTH) calcium excess [5]. Initial symptoms are nonspecific, such as weakness, malaise, fatigue and possible mood disturbances.
If not diagnosed and left untreated, it leads to devastating consequences including nephrolithiasis, nephrocalcinosis, renal failure, osteopenia and osteoporosis.
CASE REPORT
A 22-year-old male student presented to our hospital with a 2-year history of progressive lower extremity weakness. One year prior to the admission, he had been seen at another medical clinic because of fatigue and difficulty walking. His radiographs showed no fractures, and he was referred to physiotherapy for muscle strengthening. He underwent 5 months of physiotherapy. Given the lack of progress, his therapist advised him to be reassessed medically. This time, he presented to the Family Medicine clinic at our hospital. Further questioning revealed that, despite physiotherapy, his weakness had progressed and he had to quit school as he was having considerable difficulty walking up a flight of stairs. A thorough investigation was performed and showed a serum calcium level of 3.46 mmol/l (normal: 2.1–2.6 mmol/l) and a PTH level of 138 pmol/l (normal: 1.6–9.3 pmol/l). A parathyroid scan revealed a parathyroid adenoma. He was referred to our General Surgery service where he was admitted for excision of the parathyroid adenoma. Upon admission, radiographs of his pelvis showed no fracture, but severe osteopenia was observed. One day prior to the scheduled parathyroidectomy, he had a simple, low-energy fall while he was walking on his own to the hospital. Radiographs revealed a displaced subcapital fracture of his left hip, a segmental fracture of his right humerus and extreme osteopenia (Fig. 1).
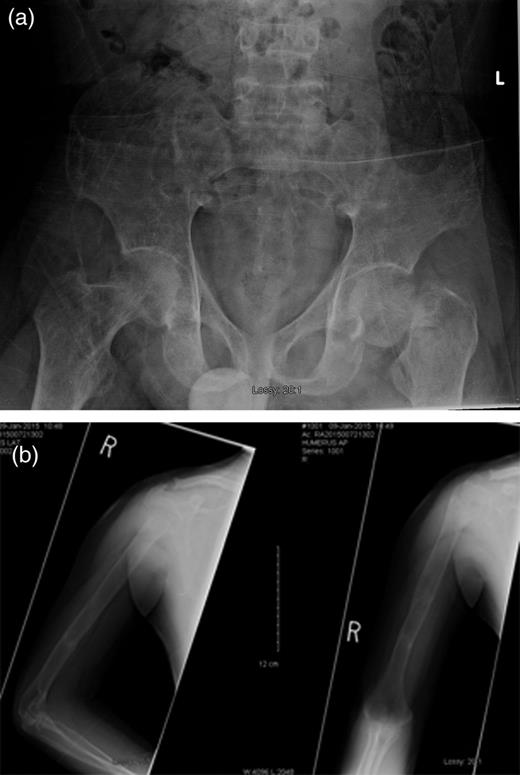
(a) Left femoral neck displaced subcapital fracture and (b) right humeral shaft segmental fracture.
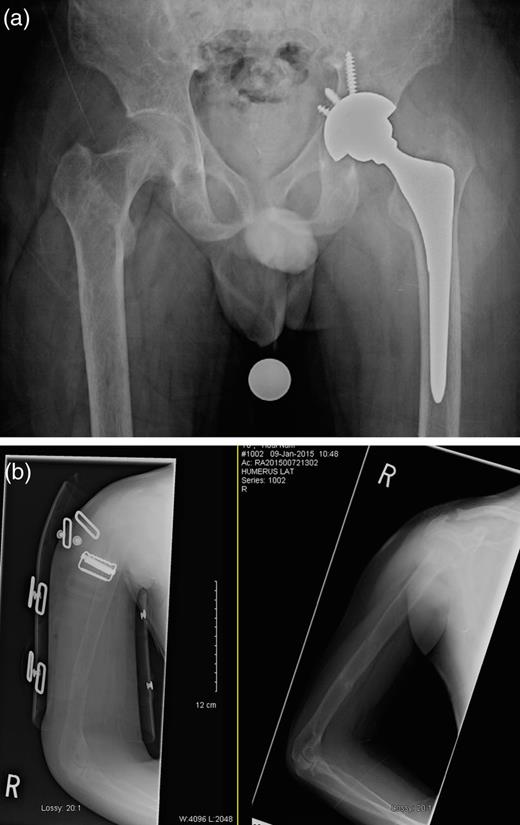
One day after sustaining this injury, the patient underwent an uncemented left total hip arthroplasty (THA) (Fig. 2), and acetabular fixation was supplemented with multiple screws, and he maintained touch-down weight bearing for 6 weeks postoperatively. His right humeral fracture was managed conservatively using a functional brace. A parathyroidectomy was performed 2 days later. The histopathology report confirmed the diagnosis of a parathyroid adenoma. Within 3 days postoperatively, the PTH level had decreased to 4.9 pmol/l, and the calcium level had returned to normal at 2.42 mmol/l. The calcium level continued to fall, and 2 weeks after the parathyroidectomy, it had reached 1.70 mmol/l. After a further 20 days, it started to normalize and then continued to remain stable, as shown in Fig. 3.
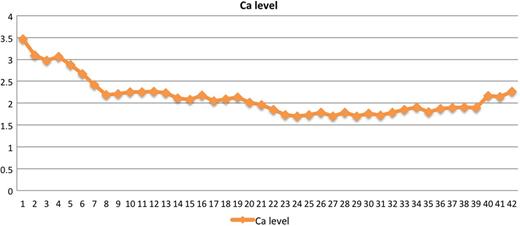
A graph for calcium level from admission to 7 weeks after surgery.
DISCUSSION
We report this case to illustrate the importance of early detection and diagnosis of PHPT, which was possible in this young and presumed healthy individual if proper assessment and management were done. Furthermore, sending him for physiotherapy without a clear diagnosis increased the likelihood of missing the diagnosis and progression of the disease.
Solitary parathyroid adenoma is the most common cause of PHPT, representing 85–90% of cases [6]. The majority of patients are asymptomatic because of early detection and treatment. Symptomatic PHPT with skeletal, renal, abdominal and neuro-psychiatric manifestations has become exceedingly rare in developed countries [6]. Our patient was unusual in that he was not diagnosed early and presented with skeletal manifestations resulting in multiple fractures including femoral neck fracture (FNF), which was treated with total hip replacement (THR). At this young age, THR would affect his lifestyle and put him at risk of revision surgery early in his life. The literature clearly shows that the earlier HPT is detected, the more reversible the disease [7].
We believe that, despite the young age of our patient, THR was still the preferred treatment in this situation owing to his poor bone quality, which could have led to failure of fixation; in addition, severe fracture displacement carries a high risk of femoral head avascular necrosis. Yang et al. found that salvage THA for failed internal fixation following FNF is a more technically demanding procedure with prolonged operative time and larger amounts of postoperative drainage (within 24 h) and that patients are at increased risk of developing hip complications compared with primary THR for acute displaced FNF.
French et al. [8] reported a case of a 21-year-old male with parathyroid adenoma who had presented with a left femoral shaft fracture and right FNFs. Although these were treated with fixations, the right side required conversion to THR within a year of his presentation. He also needed a kidney transplantation for his renal failure [9].
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- diagnostic radiologic examination
- fatigue
- asthenia
- femoral neck fractures
- pathological fractures
- hip region
- humeral fractures
- pain
- parathyroidectomy
- hip replacement arthroplasty
- hyperparathyroidism, primary
- humeral shaft fractures
- parathyroid adenoma
- excision
- early diagnosis
- undiagnosed
- fractures, multiple



