-
PDF
- Split View
-
Views
-
Cite
Cite
Sebahattin Destek, Vahit Onur Gul, Serkan Ahioglu, Zeynep Tatar, Yesim Erbil, A rare cause of chronic dysphagia: eosinophilic esophagitis, Journal of Surgical Case Reports, Volume 2014, Issue 9, September 2014, rju096, https://doi.org/10.1093/jscr/rju096
Close - Share Icon Share
Abstract
Eosinophilic esophagitis (EE) is attributable to environmental factors, allergens and several immunological causes. The most typical symptoms include dysphagia and sensation of food impingement in the retrosternal area. Although its clinical features resemble those of gastroesophageal reflux, proton pump inhibitors are not effective for its treatment. The diagnosis of EE is dependent on the pathological detection of eosinophilic infiltration in esophageal mucosa. In this study, we evaluated a patient who applied to our clinic with complaints of long-term difficulty in swallowing, sensation of food sticking while eating and weight loss; the patient was diagnosed with EE, following biochemical, radiological, endoscopic and pathological assessments and was treated with steroids. The results show that EE should be considered in the differential diagnosis of patients with dysphagia and food impingement in the retrosternal area, and the diagnosis should be confirmed through multiple esophageal biopsies.
INTRODUCTION
Eosinophilic esophagitis (EE), which first reported by Dr. John W. Dobbins in 1977 [1], is attributable to several factors, including environmental causes, food allergy and disruption of immune defence system in the digestive tract. The main symptoms of EE include dysphagia and a sensation of food impingement in the retrosternal area [2]. Its clinical features resemble those of gastroesophageal reflux disease (GORD) however; proton pump inhibitors are not effective in EE patients. The diagnosis of EE is dependent on observations of eosinophilic infiltration in endoscopic biopsy [3]. The current study emphasizes the importance of considering EE in the differential diagnosis of patients with chronic dysphagia.
CASE REPORT
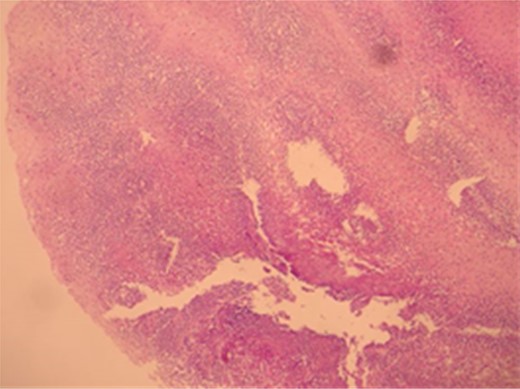
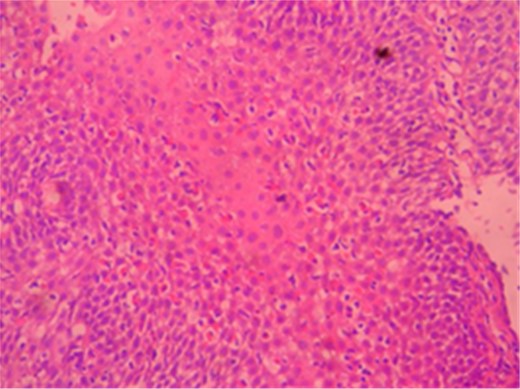
A male patient of 35 years age presented to our General Surgery Clinic with complaints of difficulty in swallowing, sensation of food sticking in the back of the breast while eating, stomach ache, weight loss and weakness for nearly a year. The fact that the symptoms chiefly arose upon ingestion of dairy products was interesting. Normal values were obtained for complete blood count serum CRP, sedimentation and total serum IgE of the patient. Standing abdominal X-ray and abdominal ultrasonography failed to reveal any evidence of pathology. Mucosal fissure and erosional areas were observed in the middle distal esophagus using upper GI endoscopy and are probably associated with reflux esophagitis; biopsies were made of the same (Fig. 1). Bulbitis and pangastritis were observed in the duodenum and stomach and biopsies were made. Pathological examinations of the endoscopic biopsies revealed evidence of chronic esophagitis in esophagus, chronic Helicobacter pylori-positive pangastritis in stomach and chronic duodenitis in the duodenum. The examination showed eosinophilic infiltration only in the esophagus (Fig. 2). Histological examination (40 X) revealed more than 30 eosinophils per field (Fig. 3). The patient was diagnosed with eosinophilic esophagitis and administered dexamethasone I.M as well as treatment for H. pylori eradication which resulted in relief of the symptoms. The patient was also instructed to avoid consumption of milk and dairy products, which caused the development of symptoms. The control endoscopic examination and pathological evaluation made after 3 months, failed to reveal evidence of esophageal eosinophilic infiltration, relapse did not occur during the following 2 years.
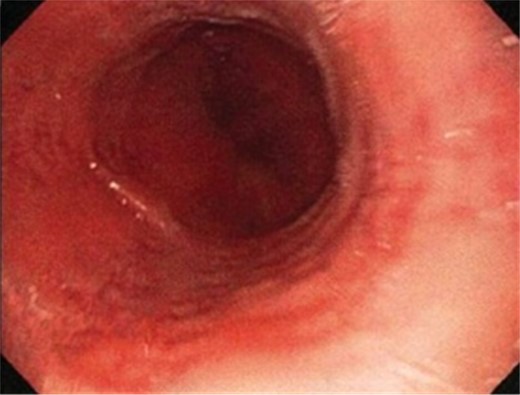
The image of linear erosional areas in middle and distal esophagus.
DISCUSSION
Studies conducted in the USA suggest that EE could affect all age and ethnic groups but is more common among children. In adults, it chiefly occurs during the 30s and 40s, with a male:female prevalence rate of 3:1. The incidence and prevalence of EE are 1/10 000 and 4/10 000, respectively, in children, and 2–6/10 000 and 27/10 000 respectively, in adults. Existing data support a family liability in EE, underscoring the importance of genetic factors [2]. EE, first defined by Dr. John W. Dobbins in 1997, is also termed allergic, primer or idiopathic eosinophilic esophagitis [1].
As with the other parts of the gastrointestinal system, eosinophil accumulation in esophagus is not observed under normal conditions and detection of any number of eosinophils in the mucosa of the esophagus is indicative of a pathological situation. Previous research has implicated two chief mechanisms in the pathogenesis of EE exposure to allergens, which initiates immune response and loss of immune tolerance. EE is frequently found in conjunction with other allergic diseases and most EE patients also suffer from other atopic diseases. The identification of atopic diseases in EE patients and response obtained to elimination diet or elementary dietary applications reinforce the idea that IgE-mediated allergic mechanisms are associated with the in etiopathogenesis of EE. However, IgE levels are not detectable in every patient [3, 4], but are chiefly observed in the pediatric age group, where food allergy has been reported as the most frequent (90%) etiology. The exact pathogenesis of EE is unclear, but increased expression of IL-4, IL-5 and IL-13 has been detected during examination of inflamed esophageal tissue [4]. In addition, mutation and excessive expression of the gene that encodes oetaxin-3, an important protein for eosinophil transition, and inflammation has been observed in nearly half of the children with the EE [5].
Vomiting, stomachache and GORD are the more frequently observed symptoms in children with EE, whereas difficulty in swallowing over a prolonged duration (90%) or repeated sensation of food sticking (60%) are the most frequent indications in children of over 12 years age and in adults [6]. The diagnosis of EE is made upon evaluation of the results of both endoscopic and histopathological tests, while the differential diagnosis of the EE is dependent on GORD, as EE could be confused with achalasia, eosinophilic gastroenteritis and hypereosinophilic syndrome.
An accurate diagnosis of EE could be made upon observations of eosinophilic infiltration in the squamous epithelium of the esophagus. An eosinophil count of >15 per high power field (HPF) upon histological examination is generally considered sufficient for a diagnosis of EE in symptomatic patients, although the exact eosinophil count per HPF for a definite diagnosis of EO has not yet been clearly established. Moreover, eosinophilic infiltration in the mucosa of the esophagus in EE patients does not show homogeneous distribution, and employing more than one tissue sample from the middle and proximal region of the esophagus is recommended for diagnosis. Accordingly the rate of diagnosis of EE is 55% with a single mucosal biopsy, but 100% when five biopsies are utilized [6].
Endoscopy examination is likely to reveal symptoms such as linear erosions, concentric circles, esophageal mucosa (crepon mucosa) and white exudative lesions containing microabscesses; of these, white exudates and linear erosions are the most frequently detected indicators of EE [7]. A prospective study showed that the frequency of EE among patients with dysphagia to solid food but without any endoscopic pathology is about 10%. High esophageal stricture is often observed in eosinophilic esophagus and is more common among middle-aged men with white skin [8].
The treatment of EE involves the identification and avoidance of systemic and topical steroids as well as allergens [9]. IL-5 and leukotriene inhibitors could be a treatment option in resistant patients [10]. Identification of the allergy triggers, if present, is essential for their inactivation or avoidance.
EE is a disease characterized by eosinophilic inflammation, which is a rare occurrence. Because its symptoms are not particular to the disease, it could often be confused with reflux esophagitis. Therefore, accurate and effective treatment is dependent on the diagnosis of eosinophilic esophagitis in patients with dysphagia and sensation of food sticking, followed by a confirmation of the diagnosis through multiple esophageal biopsies.
REFERENCES
Author notes
This article has been presented as a Poster in the 2014 National Surgery Congress. PS-0331.



