-
PDF
- Split View
-
Views
-
Cite
Cite
Harsh Dhar, Jyoti P. Dabholkar, Bhuwaneshwari M. Kandalkar, Ratnaprabha Ghodke, Primary thyroid schwannoma masquerading as a thyroid nodule, Journal of Surgical Case Reports, Volume 2014, Issue 9, September 2014, rju094, https://doi.org/10.1093/jscr/rju094
Close - Share Icon Share
Abstract
The thyroid gland is a very rare site for head and neck schwannomas. Till date there have been only 19 reported cases in English literature. Only 25% of schwannomas occur in the head and neck region, most of them arising in relation to the peripheral nerves and cervical sympathetic chain. We report a similar case, with clinical and sonological features of a benign thyroid nodule. The diagnosis of schwannoma was established on the final histopathology report and a review of the slides and the imaging was done to confirm the site of origin. A thorough review of earlier reported cases was done. We summarize the existing knowledge on this entity, emphasizing the challenge of diagnosing it pre-operatively.
INTRODUCTION
Schwannomas, first reported by Verocay in 1908 [1], are the less common form of peripheral nerve sheath tumours of the thyroid gland. The first reported case was by Delaney and Fry in 1964 [2]. They mimic a benign thyroid nodule and the overlapping features on sonography along with a paucity of cells on fine needle aspiration cytology (FNAC) make pre-operative diagnosis very challenging [1].
Such a case is reported here along with a review of 10 completely described earlier cases.
CASE REPORT
A 47-year-old male presented with a 6-month history of a progressive swelling in the right lobe of thyroid. He was euthyroid and asymptomatic. Sonography (Fig. 1) was suggestive of a right hypoechoic thyroid nodule along with a hyperechoic solid lesion adjacent to the postero-lateral aspect of the right lobe with cystic degeneration.

USG of the neck: hyperechoic cystic lesion abutting the postero-lateral aspect of the right lobe of thyroid.
Computed tomography (CT) scan of the neck (with contrast) indicated a heterogeneously enhancing lesion with multiple cystic spaces along the postero-lateral aspect of the right lobe. The lesion was seen to push the adjacent lobe anteriorly to the left (Fig. 2). The lesion was also displacing the right common carotid and the internal jugular vein laterally; however, a well-defined fat plane was seen between the lesion and the carotid sheath. No such plane was seen between the lesion and the adjacent thyroid lobe (Fig. 3).
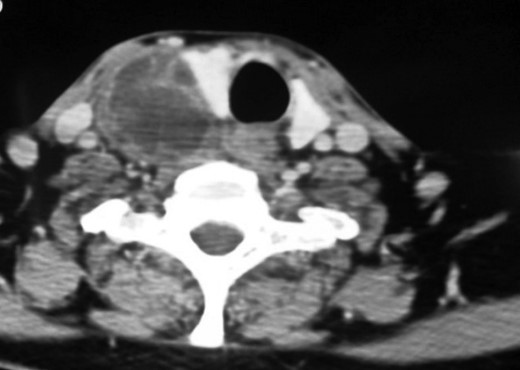
Contrast enhanced CT neck (axial section). Heterogeneously enhancing lesion with multiple cystic areas within abutting the postero-lateral aspect of the right lobe of thyroid, pushing it anteriorly and medially.
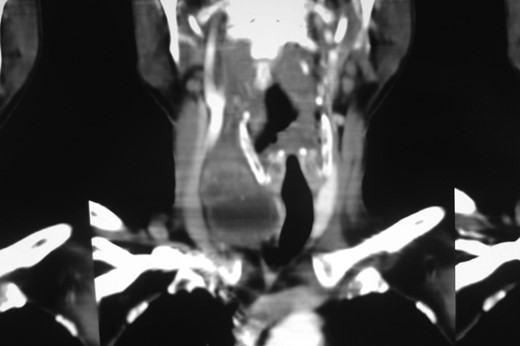
Contrast enhanced CT neck (coronal section). Coronal section showing good plane of delineation between the lesion and carotid sheath, along with mass effect on the thyroid gland and the right common carotid.
FNAC showed a benign lesion (Bethesda category II). A right hemi-thyroidectomy was done and intraoperative findings showed a firm and enlarged right lobe with area of cystic degeneration along its posterior surface, the opposite lobe being normal.
Gross appearance showed 6 × 4 × 4 cm smooth encapsulated right thyroid swelling with a posterior cystic area which was yellowish brown in colour. Walls of the cyst were bright yellow with polypoid areas (Fig. 4). Histology showed classical Antoni A (hypercellular areas) with Verocay bodies and Antoni B (hypocellular) pattern, with interspersed thyroid cells along the periphery (Figs 5–7). The lesion was reported to be arising from within the thyroid gland itself and not extrinsic to it.

Cross section of hemithyroidectomy specimen: a well-circumscribed cystic lesion with yellowish colour of the inner cyst wall; a rim of normal thyroid is seen at the periphery.
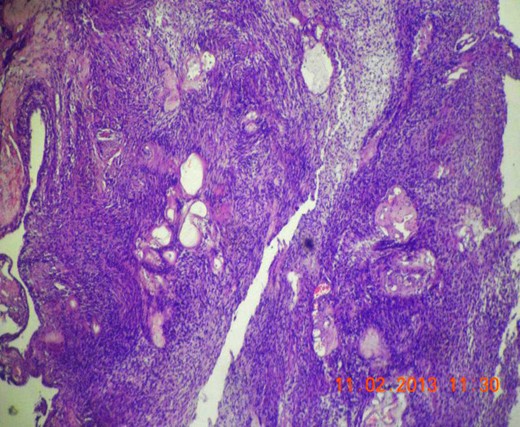
Microscopic section (H&E slide, 40×) of well-encapsulated lesion with hyper- (Antoni A) and hypocellular (Antoni B) areas. Multiple cystic areas are also seen.
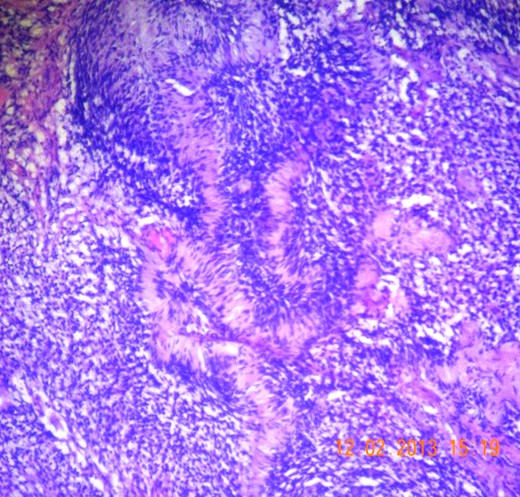
Microscopic section (H&E slide, 40×) of Verocay bodies within Antoni A pattern.
Microscopic section (H&E slide, 100×) of magnified view of a region in Fig. 6 showing Verocay bodies.
DISCUSSION
Peripheral nerve sheath tumours of the thyroid may be benign or malignant, the benign variety includes neurofibromas and schwannomas. Within the neck, the most common site of schwannoma is the vagus, followed by the cervical sympathetic chain [3]. The origin of primary thyroid schwannomas—the rarest subset of neck schwannomas—has been a matter of speculation and they are thought to arise from the intrathyroid sensory nerves or from the autonomic innervation to the thyroid [3].
The rarity of the diagnosis inspired us to review the FNAC slides, which probably failed to show the presence of spindle cells as a result of the aspirate being drawn from the thyroid tissue surrounding the posteriorly placed lesion. A guided FNAC would have had better accuracy.
The images of the lesion had created a diagnostic dilemma as to its origin, i.e. extrinsic or intrinsic to the thyroid. A review of the sonological and CT images with the radiologist was done to discuss its possible origin. Both seem to indicate that the lesion was extrinsic to the thyroid. However, a well-preserved plane between the lesion and the carotid sheath rules out a cervical sympathetic origin. The possibility of schwannoma of the thyroid bed still remained.
The pathologists were in favour of a diagnosis of primary thyroid schwannoma saying that the lesion was arising from within the thyroid with a rim of thyroid tissue around the capsule and a major part of the posterior half of the right lobe had been replaced by the lesion.
A thorough literature search has shown only 19 completely reported cases of primary thyroid schwannoma, 10 of which have been reviewed here (Table 1).
| . | Presentation . | USG . | FNAC . | CT scan . | Surgery done . | IHC . | Review of FNAC slides . |
|---|---|---|---|---|---|---|---|
| Delaney and Fry et al. (first reported case 1953) [2] | Asymptomatic neck swelling | – | – | – | Hemi-thyroidectomy | – | – |
| De Paoli et al. [1] | Enlarging neck mass with foreign body sensation in the throat | Hypoechoic nodule with rich vascularity | USG-guided apirate-inconclusive | – | Total thyroidectomy done i/v/o suspected malignancy | S 100 +ve | Aggregate of spindle cells seen on previous slides |
| Subramaniam et al. [10] | Asymptomatic neck swelling | Thyroid nodule with large cystic degeneration | Colloid goitre | – | Hemi-thyroidectomy | – | – |
| An et al. [4] | Asymptomatic neck swelling | Hypoechoic nodule with cystic changes | Paucicellular aspirate with few round cells and spindle cells | Well-enhancing homogenous mass | Hemi-thyroidectomy | S 100 +ve Tgb −ve | – |
| Kandil et al. [5] | Neck swelling with hoarseness and dysphagia | – | Inconclusive | Enhancing thyroid mass compressing the oesophagus | Hemi –thyroidectomy (frozen section done: spindle cell tumour) | S100 and Vimentin +ve | – |
| Sujita et al. [6] | Asymptomatic neck swelling | Well-defined solid thyroid lesion | Inflammatory cells seen inconclusive | Low-density mass on plain CT and moderately enhancing on contrast | Hemi-thyroidectomy | – | – |
| Jayaram [7] | Asymptomatic neck swelling | Hypoechoic nodule | USG-guided aspirate; pallisading pattern of spindle cells s/o schwannoma | – | Hemi-thyroidectomy | S 100 +ve (done on fine needle aspirate) | Both final histology and FNAC slides were indicative of schwannoma |
| Aron et al. (2 cases) [8] | Asymptomatic neck swelling | Hypoechoic nodule with cystic spaces | USG-guided aspirates s/o schwannoma | – | Hemi-thyroidectomy | – | Both final histology and FNAC slides were indicative of schwannoma |
| Mikosch et al. [9] | Asymptomatic neck swelling | Hypoechoic thyroid nodule | USG-guided FNAC: suspicious of neural tumour | – | Hemothyroidectomy | – | – |
| . | Presentation . | USG . | FNAC . | CT scan . | Surgery done . | IHC . | Review of FNAC slides . |
|---|---|---|---|---|---|---|---|
| Delaney and Fry et al. (first reported case 1953) [2] | Asymptomatic neck swelling | – | – | – | Hemi-thyroidectomy | – | – |
| De Paoli et al. [1] | Enlarging neck mass with foreign body sensation in the throat | Hypoechoic nodule with rich vascularity | USG-guided apirate-inconclusive | – | Total thyroidectomy done i/v/o suspected malignancy | S 100 +ve | Aggregate of spindle cells seen on previous slides |
| Subramaniam et al. [10] | Asymptomatic neck swelling | Thyroid nodule with large cystic degeneration | Colloid goitre | – | Hemi-thyroidectomy | – | – |
| An et al. [4] | Asymptomatic neck swelling | Hypoechoic nodule with cystic changes | Paucicellular aspirate with few round cells and spindle cells | Well-enhancing homogenous mass | Hemi-thyroidectomy | S 100 +ve Tgb −ve | – |
| Kandil et al. [5] | Neck swelling with hoarseness and dysphagia | – | Inconclusive | Enhancing thyroid mass compressing the oesophagus | Hemi –thyroidectomy (frozen section done: spindle cell tumour) | S100 and Vimentin +ve | – |
| Sujita et al. [6] | Asymptomatic neck swelling | Well-defined solid thyroid lesion | Inflammatory cells seen inconclusive | Low-density mass on plain CT and moderately enhancing on contrast | Hemi-thyroidectomy | – | – |
| Jayaram [7] | Asymptomatic neck swelling | Hypoechoic nodule | USG-guided aspirate; pallisading pattern of spindle cells s/o schwannoma | – | Hemi-thyroidectomy | S 100 +ve (done on fine needle aspirate) | Both final histology and FNAC slides were indicative of schwannoma |
| Aron et al. (2 cases) [8] | Asymptomatic neck swelling | Hypoechoic nodule with cystic spaces | USG-guided aspirates s/o schwannoma | – | Hemi-thyroidectomy | – | Both final histology and FNAC slides were indicative of schwannoma |
| Mikosch et al. [9] | Asymptomatic neck swelling | Hypoechoic thyroid nodule | USG-guided FNAC: suspicious of neural tumour | – | Hemothyroidectomy | – | – |
USG, ultrasonography; FNAC, fine needle aspiration cytology; k/c/o, known case of; s/o, suggestive of; i/v/o, in view of .
| . | Presentation . | USG . | FNAC . | CT scan . | Surgery done . | IHC . | Review of FNAC slides . |
|---|---|---|---|---|---|---|---|
| Delaney and Fry et al. (first reported case 1953) [2] | Asymptomatic neck swelling | – | – | – | Hemi-thyroidectomy | – | – |
| De Paoli et al. [1] | Enlarging neck mass with foreign body sensation in the throat | Hypoechoic nodule with rich vascularity | USG-guided apirate-inconclusive | – | Total thyroidectomy done i/v/o suspected malignancy | S 100 +ve | Aggregate of spindle cells seen on previous slides |
| Subramaniam et al. [10] | Asymptomatic neck swelling | Thyroid nodule with large cystic degeneration | Colloid goitre | – | Hemi-thyroidectomy | – | – |
| An et al. [4] | Asymptomatic neck swelling | Hypoechoic nodule with cystic changes | Paucicellular aspirate with few round cells and spindle cells | Well-enhancing homogenous mass | Hemi-thyroidectomy | S 100 +ve Tgb −ve | – |
| Kandil et al. [5] | Neck swelling with hoarseness and dysphagia | – | Inconclusive | Enhancing thyroid mass compressing the oesophagus | Hemi –thyroidectomy (frozen section done: spindle cell tumour) | S100 and Vimentin +ve | – |
| Sujita et al. [6] | Asymptomatic neck swelling | Well-defined solid thyroid lesion | Inflammatory cells seen inconclusive | Low-density mass on plain CT and moderately enhancing on contrast | Hemi-thyroidectomy | – | – |
| Jayaram [7] | Asymptomatic neck swelling | Hypoechoic nodule | USG-guided aspirate; pallisading pattern of spindle cells s/o schwannoma | – | Hemi-thyroidectomy | S 100 +ve (done on fine needle aspirate) | Both final histology and FNAC slides were indicative of schwannoma |
| Aron et al. (2 cases) [8] | Asymptomatic neck swelling | Hypoechoic nodule with cystic spaces | USG-guided aspirates s/o schwannoma | – | Hemi-thyroidectomy | – | Both final histology and FNAC slides were indicative of schwannoma |
| Mikosch et al. [9] | Asymptomatic neck swelling | Hypoechoic thyroid nodule | USG-guided FNAC: suspicious of neural tumour | – | Hemothyroidectomy | – | – |
| . | Presentation . | USG . | FNAC . | CT scan . | Surgery done . | IHC . | Review of FNAC slides . |
|---|---|---|---|---|---|---|---|
| Delaney and Fry et al. (first reported case 1953) [2] | Asymptomatic neck swelling | – | – | – | Hemi-thyroidectomy | – | – |
| De Paoli et al. [1] | Enlarging neck mass with foreign body sensation in the throat | Hypoechoic nodule with rich vascularity | USG-guided apirate-inconclusive | – | Total thyroidectomy done i/v/o suspected malignancy | S 100 +ve | Aggregate of spindle cells seen on previous slides |
| Subramaniam et al. [10] | Asymptomatic neck swelling | Thyroid nodule with large cystic degeneration | Colloid goitre | – | Hemi-thyroidectomy | – | – |
| An et al. [4] | Asymptomatic neck swelling | Hypoechoic nodule with cystic changes | Paucicellular aspirate with few round cells and spindle cells | Well-enhancing homogenous mass | Hemi-thyroidectomy | S 100 +ve Tgb −ve | – |
| Kandil et al. [5] | Neck swelling with hoarseness and dysphagia | – | Inconclusive | Enhancing thyroid mass compressing the oesophagus | Hemi –thyroidectomy (frozen section done: spindle cell tumour) | S100 and Vimentin +ve | – |
| Sujita et al. [6] | Asymptomatic neck swelling | Well-defined solid thyroid lesion | Inflammatory cells seen inconclusive | Low-density mass on plain CT and moderately enhancing on contrast | Hemi-thyroidectomy | – | – |
| Jayaram [7] | Asymptomatic neck swelling | Hypoechoic nodule | USG-guided aspirate; pallisading pattern of spindle cells s/o schwannoma | – | Hemi-thyroidectomy | S 100 +ve (done on fine needle aspirate) | Both final histology and FNAC slides were indicative of schwannoma |
| Aron et al. (2 cases) [8] | Asymptomatic neck swelling | Hypoechoic nodule with cystic spaces | USG-guided aspirates s/o schwannoma | – | Hemi-thyroidectomy | – | Both final histology and FNAC slides were indicative of schwannoma |
| Mikosch et al. [9] | Asymptomatic neck swelling | Hypoechoic thyroid nodule | USG-guided FNAC: suspicious of neural tumour | – | Hemothyroidectomy | – | – |
USG, ultrasonography; FNAC, fine needle aspiration cytology; k/c/o, known case of; s/o, suggestive of; i/v/o, in view of .
Most common presentation was an asymptomatic neck mass in the fourth or fifth decade without any sex predilection. Majority of the lesions appeared as a hypoechoic nodule on USG with variable cystic degeneration.
Pre-operative CT scan was done in three cases [4–6]. The lesion was homogeneous and of low density on plain CT, with good post-contrast enhancement. Sujita et al. [6] explained that the well-enhancing areas on CT corresponded to the hypercellular Antoni A areas, whereas those showing poor enhancement corresponded to Antoni B pattern.
Schwannoma was correctly diagnosed on pre-operative FNAC in only three cases [7–9], all three being done under sonographic guidance .Most of the remaining cases were reported either as colloid goitre with cystic degeneration or as paucicellular aspirates with scattered spindle cells and labelled inconclusive [1, 4–6, 10].
On immunohistochemistry (IHC) schwannomas are positive for S100 and Vimentin and negative for Desmin and SMA. IHC was used as a confirmatory marker in four cases [1, 4, 5, 7].
Intraoperative frozen section was done in one case [5], which showed a spindle cell tumour. This may prove to be a useful intraoperative diagnostic modality.
Primary thyroid schwannoma is a rare entity. It closely mimics a thyroid nodule in presentation and sonology. Better dialogue with the pathologist, use of USG-guided FNAC, IHC and intraoperative frozen section are sure to improve pre-operative diagnosis. More reports will improve our understanding and raise our index of suspicion.



