-
PDF
- Split View
-
Views
-
Cite
Cite
Emmanuel M. Gabriel, Michelle Savu, Discovery of a rare ileocecal plasmacytoma, Journal of Surgical Case Reports, Volume 2014, Issue 3, March 2014, rju016, https://doi.org/10.1093/jscr/rju016
Close - Share Icon Share
Abstract
Here we report the discovery of an extramedullary ileocecal plasmacytoma, a rare entity reported only ∼60 times in the literature. This finding occurred during management of a patient who had sustained an occult perforation during diagnostic colonoscopy. We explored the patient finding a large ileocecal perforation, and thus a right hemicolectomy was performed. Interestingly, the pathology of the mass was consistent with an extramedullary plasmacytoma, which is a very rare gastrointestinal diagnosis. We end by summarizing the presentation and work-up of extramedullary plasmacytoma.
INTRODUCTION
Iatrogenic colonic perforation during colonoscopy is a well recognized though infrequent complication of the procedure. The rate of perforation for colonoscopy done for all indications, whether diagnostic or therapeutic, has been reported to be <1% [1]. Risk factors for colonoscopic perforation include therapeutic interventions including polypectomy and biopsy particularly when done for larger lesions, pneumatic dilation and endoscopic coagulation [2, 3].
Here, we present a patient who sustained an injury to the cecum and terminal ileum following a polypectomy during routine screening colonoscopy. The patient presented with delayed symptoms of perforation. We therefore decided to perform an exploratory laparotomy which showed a significant defect across his ileocecal junction. The lesion was found to be an extramedullary plasmacytoma, a rare diagnosis in gastrointestinal pathology.
CASE PRESENTATION
We report a case of a 62-year-old man with a past medical history significant for hypertension and hypothyroidism who underwent diagnostic colonoscopy for melena at an outside facility at ∼9:00 a.m. on the day of the injury. The gastroenterologist identified a large nearly 4 cm pedunculated and ulcerated polyp at the medial border of the cecum in close proximity to the ileocecal junction (Fig. 1). Given the characteristics of the polyp, the concern for malignancy was high. The lesion was removed endoscopically in its entirety through the use of a hot snare.

Ileocecal plasmacytoma. Gross appearance of polyp during the diagnostic colonoscopy for our case. The polyp measured nearly 4 cm and had an obvious ulceration on its surface as shown. It had a thin, long stalk and so was removed by hot snare.
The patient presented to the emergency department 5h post-procedure complaining of abdominal pain and had a firm abdomen. He had a leukocytosis of 17 000. His Computerized Tomography (CT) scan showed a significant amount of pneumoperitoneum and inflammatory changes in the right lower quadrant in the region of the terminal ileum and cecum (Fig. 2). As the patient was improving, we initially attempted a trial of non-operative management. In the interim, pathology from the endoscopic biopsy had returned as extramedullary plasmacytoma. A baseline carcinoembryonic antigen level was 0.8. After ∼48 h the patient manifested signs of unsuccessful non-operative management characterized by increasing abdominal pain, tachycardia and rising leukocytosis. Therefore, we decided to perform an exploratory laparotomy.
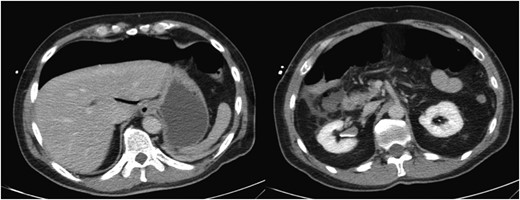
Colonoscopic perforation on CT. CT scan of the abdomen revealing significant intra-abdominal free air (left). On a lower portion of the scan, there are inflammatory changes evident in the right lower quadrant in the region of the ileum and cecum (right). These structures are difficult to discern in the presence of the inflammatory changes.
In the operating room, we found two interloop abscesses in the mesentery of the distal ileum and cecum. The right colon was markedly edematous. After performing a right hemicolectomy including ∼10 cm of edematous distal ileum, we were able to identify the 2.5 cm defect extending across the ileocecal junction where the biopsy was performed (Fig. 3). We performed a side-to-side stapled anastamosis from the terminal ileum to transverse colon, and diverted the gastrointestinal tract with a loop ileostomy.

Gross pathology of colonoscopic injury to ileocecal junction. Gross pathology of the iatrogenic colonoscopic injury to the ileocecal junction sustained during the snare polypectomy. The perforation measured ∼2.5 cm across the ileocecal valve.
Pathologic analysis of the polyp returned as an extramedullary plasmacytoma. Figure 4 shows the polyp histology. The top left insert shows hematoxylin and eosin (H&E) staining, whereas the upper and lower right inserts show special staining for the kappa or lambda type of the light chain, respectively. The left lower insert shows a higher power magnification showing multiple plasma cells with the presence of the characteristic cartwheel or clockface nuclei typical of plasma cells. As illustrated, the entirety of the polyp stains for the kappa light chain, indicating that the polyp comprised a monoclonal population of plasma cells and confirming that the lesion is a rare extramedullary plasmacytoma. These photos illustrate that the plasma cells were confined to the polyp itself, and that the polyp was pedunculated on a stalk of gastrointestinal tissue which can be appreciated at the mucosal border of the specimen. The pathology of the right colon and terminal ileum did not reveal any remaining areas of plasmacytoma at the site of perforation on either the colon or the terminal ileum.
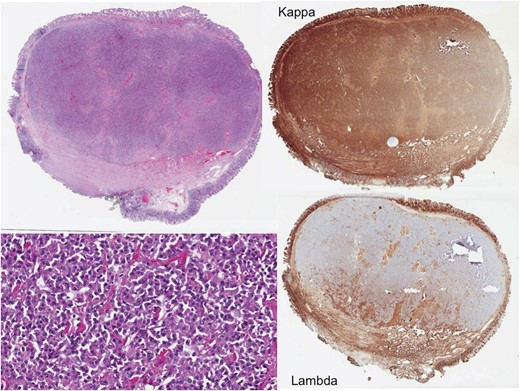
Histology of the ileocecal plasmacytoma. Pathology revealed that the polyp was an extramedullary plasmacytoma. The top left shows H&E staining and the bottom left shows increased magnification, illustrating classic cartwheel nuclei. The top right and bottom right show special staining for either the kappa or lambda light chain, respectively. Here the polyp specifically stains for the kappa light chain, indicating that it comprised a monoclonal population of plasma cells.
DISCUSSION
Here we have presented a unique case of iatrogenic perforated plasmacytoma following colonoscopic polypectomy. Extramedullary plasmacytoma (EMP) is a rare diagnosis with few cases presented in the literature. Lopes da Silva in a 2012 review of EMP reported that there were 61 cases described in the literature searching as far back as 1947 [4]. The true incidence of EMP is unknown; however, as many patients will be asymptomatic. Of these 61 cases, 20 occurred in the duodenum, 24 in the jejunum and 17 in the ileum.
The most common presentations were abdominal pain and other nonspecific symptoms including nausea, vomiting and weight loss [4]. There is one case report of EMP presenting as a small bowel intusseception in a patient with multiple myeloma [5]. This may have been a similar circumstance with our patient whereby the large plasmacytoma was located in the distal ileum near the ileocecal valve. The lesion may have migrated into the cecum during the polypectomy as an intussceptum, which explains our finding of the perforation across both the cecum and terminal ileum. Other cases in the literature have been described where EMPs are located in the distal ileum [6, 7]. Overall, the median age at presentation is 55 years and tends to be more frequent in men [4]. Imaging modalities including CT and positron emission tomography have been used in the work-up of plasmacytoma but tend to be nonspecific [4].
The course of this condition is indolent and typically only requires treatment when symptomatic. Treatment options classically have involved surgical resection. However, there are recent studies showing that these lesions may also be successfully treated endoscopically [8]. As with any polyp removed endoscopically, the size of the lesion is related to the success of the removal as well as the rate of perforation. As endoscopic techniques continue to evolve, endoscopists have been able to treat larger and more invasive extramedullary gastrointestinal plasmacytomas in more aggressive but clinically safe and effective manners. Kodani et al. [9, 10] have shown successful endoscopic techniques in resection of colonic plasmacytomas which extend into the mucosa. In our case, the plasmacytoma was pedunculated and did not appear to invade the mucosa either grossly or on the histology as shown in Fig. 4. Therefore, the injury sustained to the bowel wall was most likely iatrogenic from the application of the hot snare rather than an erosion of the lesion through the layers of the bowel wall.



