-
PDF
- Split View
-
Views
-
Cite
Cite
Kenichiro Hamada, Nofirumi Naka, Shinsuke Omori, Hidetatsu Outani, Kazuya Oshima, Susumu Joyama, Nobuhito Araki, Hideki Yoshikawa, Intercalary endoprosthesis for salvage of failed intraoperative extracorporeal autogeneous irradiated bone grafting (IORBG) reconstruction, Journal of Surgical Case Reports, Volume 2014, Issue 3, March 2014, rju014, https://doi.org/10.1093/jscr/rju014
Close - Share Icon Share
Abstract
Intraoperative extracorporeal autogeneous irradiated bone grafting (IORBG) after femoral tumor resection ultimately sometimes will fail in patients achieving long-term survival. There are several alternative surgical approaches for revision of these reconstructions. In 2002 and 2005, two patients with femoral intercalary resection of malignant tumor (synovial sarcoma and MFH) underwent IORBG reconstruction with intramedullary nail or plate. At 32 and 96 months after IORBG reconstruction, both patients had failed IORBG (pathological fracture) in the femur. We used custom-made endoprostheses in these two patients to reconstruct femoral diaphyseal bone defect after excision of failed IORBG. Follow-up of the patients averaged 40.5 months (range, 39–42 months) after endoprosthetic revision. Musculoskeletal Tumor Society scores averaged 75% (66–83%). When used to salvage massive IORBG failure from fractures, intercalary endoprosthetic revision preserves limb function with minimal complications.
INTRODUCTION
Advances in adjuvant and neoadjuvant therapies and accurate preoperative imaging techniques have improved the prognosis of patients with sarcoma. Tumors in the diaphysis are relatively uncommon, and in some patients it may be possible to achieve adequate margins without sacrificing the adjacent articular surface [1]. There are several alternative surgical approaches to reconstruct a femoral diaphyseal defect. Available methods include the use of autogeneous extracorporeally irradiated bone [1–3], massive allograft [4], distraction osteogenesis [5] and intercalary custom-made endoprostheses [6, 7, 8].
Previously, long-term results of intercalary endoprosthetic reconstruction are not clear [7], and we have used extracorporeal radiation and re-implantation in patients with primary or metastatic diaphyseal bone tumors [2]. Custom-made diaphyseal implants allow immediate weight bearing, but the complications include loosening, wear and breakage of the implants [6, 7]. However, intraoperative extracorporeal autogeneous irradiated bone grafting (IORBG) after femoral tumor resection also sometimes fails to achieve long-term survival due to non-union or fracture of bones and breakage of implant [1, 2]. Most especially, a pathologic fracture in a femoral lesion has a marked effect on the patient's quality of life [6].
Here, we present a useful salvage surgery to reconstruct femoral diaphyseal defects due to IORBG fracture with custom-made intercalary endoprostheses in two elderly patients.
CASE REPORT
In 2002 and 2005, two patients with femoral intercalary resection of malignant tumor underwent IORBG reconstruction with intramedullary nail or plate. At 32 and 96 months after IORBG reconstruction, both patients had IORBG fractures. We used custom-made endoprostheses in these two patients to reconstruct femoral diaphyseal bone defect after excision of failed IORBG.
The intercalary endoprosthetic system (K-MAX, KYOCERA Medical Corporation, Kyoto, Japan) for femoral and tibial diaphyseal bone tumors is custom made with titanium alloy. The prosthesis took ∼3 weeks to manufacture, and the cemented stems were proximally and distally linked by a taper locking system with a bolt passing through parts of the prosthesis [6].
Resection of the graft bone at the appropriate level and removal of the implant were carried out. The proximal and distal intramedullary canals were reamed to the appropriate size. Stems were meticulously secured with bone cement to achieve the appropriate rotational alignment. Once the cement had fully hardened, taper lock was placed onto each prostheses. Active physiotherapy was started on the second postoperative day, wherein, the patient was allowed to partially weight bear with gradual progression to full weight bearing by the time of discharge.
Functional outcome was assessed using the Musculoskeletal Tumor Society (MSTS) functional evaluation system for reconstructive procedures after skeletal resection [9]. The MSTS score is composed of pain, function, emotional acceptance, walking ability, gait and use of walking aids, with a higher score indicating better functional outcome.
Case 1: A 61-year-old male was treated at the age of 54 for primary soft-tissue sarcoma of the thigh which invaded the femur (Fig. 1A–D). Wide en bloc resection of the tumor with involved femoral diaphysis, isolation of the tumor with involved bone, extracorporeal irradiation with 50 Gy as a single bolus dose to the isolated bone and reimplantation of the irradiated bone into the host with intramedullary nail were performed (Fig. 2A). At 74 months after primary surgery, graft bone fracture and intramedullary nail breakage occurred at the proximal diaphysis (Fig. 2B). Segmental intercalary resection, implant removal and reconstruction with custom-made intercalary prosthesis were performed (Fig. 2C and D). The best MSTS score was 20 of 30.
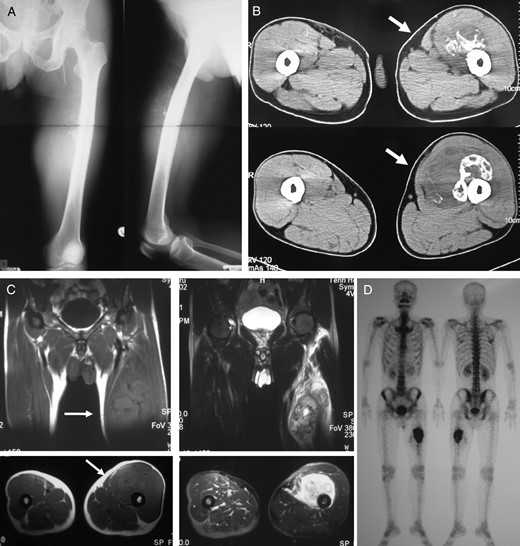
A 54-year-old male with primary soft tissue sarcoma. Plain radiograph (A) and CT (B) showing lytic destructive lesion in left femoral diaphyseal bone. T1- and T2-weighted magnetic resonance imaging (C) showing a soft tissue mass (20 × 20 × 12 cm) around femoral bone. Bone scintigraphy (D) showing increased uptake in femoral diaphyseal bone.
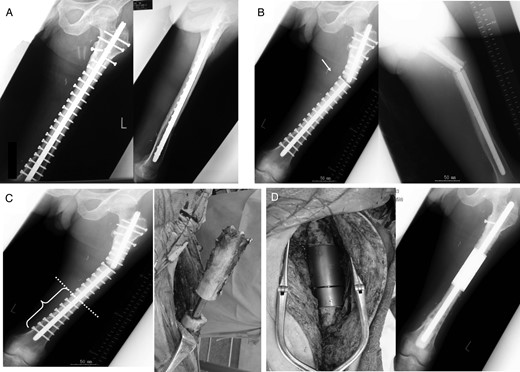
Radiographs showing extracorporeal irradiation after wide resection and stabilization with intramedullary nail (A). At 74 months after operation, radiograph showing fracture of graft bone with broken implant (B and C) and revision with intercalary endoprosthesis (D).
Case 2: A 71-year-old female was treated at the age of 68 for metastatic synovial sarcoma of the femur (Fig. 3A). Wide en bloc resection of the tumor and reconstruction with the use of IORBG were performed (Fig. 3B). At 32 months later, distal thigh pain due to fracture of the graft and breakage of plate occurred (Fig. 3C). Failed graft bone resection, implant removal and reconstruction with custom-made intercalary endoprosthesis were performed (Fig. 3D). The best MSTS score was 25 of 30. Aseptic loosening occurred at 29 months after the first endoprosthetic replacement which required a revision procedure (Fig. 3E and F). This was associated with osteolysis around the distal femoral end of the prosthesis.
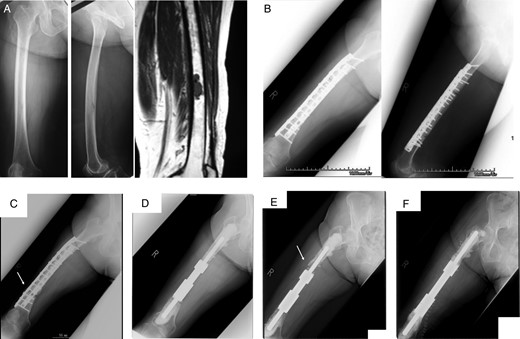
A 68-year-old female with metastatic synovial sarcoma in right femoral diaphyseal bone. Plain radiograph and MRI (A) showing metastatic bone tumor. Radiograph (B) showing wide resection included femoral diaphyseal bone and reconstruction with IORBG and plate. At 32 months after surgery, radiograph (C) showing graft bone fracture (arrow) and reconstruction with intercalary endoprosthesis (D). Aseptic loosening occurred 29 months after surgery (E), and revision surgery was performed (F).
DISCUSSION
There are several options for reconstruction of defects in the femoral diaphysis after resection of the tumor. However, the optional methods for reconstruction of defects are unclear.
Femoral diaphyseal replacements have demonstrated acceptable long-term survival and functional outcome [8]. Hanna et al. [8] reviewed 23 patients who underwent limb salvage by endoprosthetic replacement of the femoral diaphysis for primary bone tumor with a reconstruction survival of 85% at 5 years and 68% at 10 years.
Biological reconstruction is believed to be more time consuming than endoprosthetic replacement with a prolonged period of immobilization after surgery and a significant risk of non-union and/or fracture [7]. Fractures remained a major problem in patients with intercalary femur IORBG [1].
Generally, the patients with implant failure and non-union and fracture of graft bone require open reduction and internal fixation with bone grafting [1]. For our two elderly patients with fractures of the graft bones, the latter were salvaged using custom-made intercalary prostheses. When the patients were subjected to reconstruction with repeat bone graft for implant and IORBG failure, it is difficult for elderly patients to require a lengthy period of non-weight bearing for union. Prolonged immobilization is required for graft union, and there are high rates of failure after biological reconstruction, which makes its use less favorable for these patients, especially those receiving palliative treatment. Endoprosthetic reconstruction of the femoral diaphysis allows patients to recover early weight bearing and function without a lengthy period of no weight bearing. This method is a useful salvage surgery for elderly patients. Although both patients resumed daily life early, one patient underwent revision to an intercalary replacement at 29 months for aseptic loosening of the distal stem. As a risk of later failure and subsequent need for surgery, the indication on young patients should be considered.
Custom-made intercalary endoprosthesis is a useful surgical treatment for fracture of an IORBG reconstruction in limb salvage surgery especially in elderly patients.



