-
PDF
- Split View
-
Views
-
Cite
Cite
Lorenzo Dioscoridi, Giampaolo Perri, Giancarlo Freschi, Chylous mesenteric cysts: a rare surgical challenge, Journal of Surgical Case Reports, Volume 2014, Issue 3, March 2014, rju012, https://doi.org/10.1093/jscr/rju012
Close - Share Icon Share
Abstract
A mesenteric cyst is defined as a cyst that is located in the mesentery of the gastrointestinal tract and may extend from the base of the mesentery into the retroperitoneum. It is often asymptomatic and therefore it is usually found as an incidental finding. Preoperative diagnosis may be possible with computed tomography and magnetic resonance imaging. However, the correct diagnosis can only be made with histology. The first-choice therapy is the complete removal of the cyst, which must be accurately planned according to the anatomy of the lesion, its dimensions and its relationships with major abdominal structures. We present two clinical cases: the one of a 30-year-old man with a mesenteric cyst that was removed by laparoscopy and the other of a 61-year-old woman who underwent open excision of a huge retroperitoneal cyst.
INTRODUCTION
Mesenteric cysts are identified in ∼1 of 100 000 hospital admissions [1]. Mesenteric cysts can occur anywhere in the mesentery of the gastrointestinal tract and also may extend from the base of the mesentery into the retroperitoneum: 60% of mesenteric cysts occur in the small-bowel mesentery, 24% in the large-bowel mesentery and 14.5% in the retroperitoneum [2, 3].
Chylous mesenteric cysts have an estimated incidence of 7.3% of all abdominal cysts. It was firstly described by Von Rokitansky in 1842 [4].
Patients generally present with vague abdominal pain sometimes associated with a palpable mass. Although often asymptomatic, 10% of patients with such cysts present as an acute abdomen [3, 4]. The mainstay of therapy is the complete surgical removal of the cyst [4].
CASE REPORTS
First case
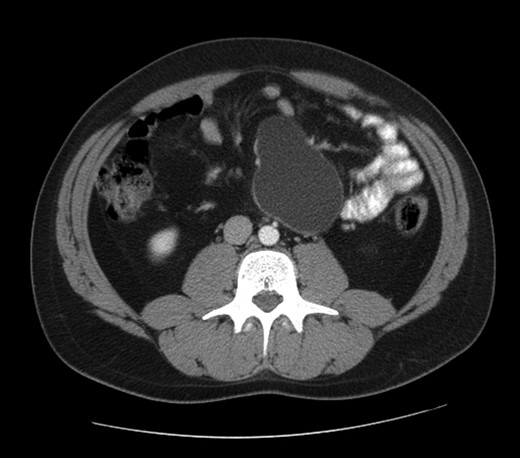
A 30 year-old man presented with diffuse abdominal pain in the last 6 months, without other abdominal or systemic symptoms. At the physical examination, a rounded swelling in the upper left quadrant was appreciated. The abdominal ultrasonography confirmed a rounded cystic formation, with regular walls, in the mesogastric region. A computed tomography scan showed a cystic mass measuring 95 × 60 mm, interjected between jejunal loops and located close to the inferior mesenteric artery and aorta (see Fig. 1).
With the informed consent of the patient, we planned to remove the mass with laparoscopic technique.
The first trocar was placed in a supra-umbilical port with Hasson's ‘open’ technique. The second trocar was placed in right hypocondrium. With the omentum raised up and the small intestine disposed to the right, the cyst was seen and the third trocar was placed in the left lumbar region.
The dissection started with an incision of the peritoneal covering of the mass that was then peeled away from the underlying fat tissue. During the dissection, the cyst was damaged and a dense white milk-like fluid spilled out. The cyst was completely dissected and removed.
The laboratory tests on the cyst's liquid confirmed chylous content (just chemical physical properties of the fluid content were analyzed, without the cyst's histology). The postoperative course was regular and the patient left the department on the fifth postoperative day.
Second case
A 61-year-old woman came to our department for regurgitation, dyspepsia and dry cough. The patient had the diagnosis of GERD associated with a hiatal hernia (to which are related the presenting symptoms).
A routine abdominal ultrasonography, performed during hospitalization, surprisingly showed a mesogastric cystic formation between aorta and the caval vein.
The abdominal computed tomography scan with contrast revealed a huge (10 cm of diameter) retroperitoneal cyst, oval shaped and containing dense fluid, located within the caval vein and the aorta, under the origin of the renal artery, partially dislocating the caval vein to the right (see Fig. 2).
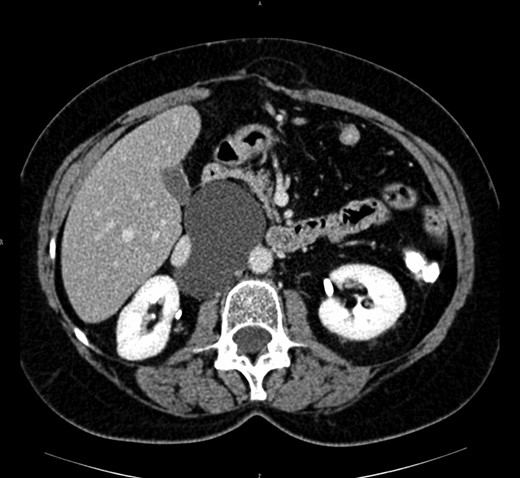
Computed tomography view of the mesenteric cyst partially dislocating the caval vein.
With the informed consent of the patient, a laparotomy was undertaken with removal of the cyst and a Nissen fundoplication was carried out.
The dissection started after the complete mobilization of ascending colon and the kocherization of the duodenum, with the complete detachment of the cyst from the major retroperitoneal blood vessels. The cyst was not damaged during the operation. Again, the laboratory tests on the cyst's liquid confirmed a chylous content. The postoperative recovery was normal and the patient returned home on the ninth postoperative day.
DISCUSSION
Our two cases highlight the asymptomatic nature of mesenteric cysts and its difficult diagnosis. The diagnosis can be challenging because chylous cysts mimic other pathologies, such as pancreatic pseudocysts or cystic tumors, pelvic diseases and aortic aneurysms. Preoperative diagnosis may be achieved with the imaging investigations (ultrasonography, computed tomography, nuclear magnetic resonance) [4–6]. Ultrasonography must be the first-line technique because it can localize the cystic mass and often the involvement of the near anatomical structures. Computed tomography scan confirms the ultrasonography's diagnosis and is really important in order to adequately plan the surgical approach [7, 8].
The treatment of choice is the complete surgical excision of the cyst [9, 10]. The first effective surgical treatment of a mesenteric cyst was performed in 1880s by Tillaux [2]. In 1897, O'Conor described the marsupialization of a chylous mesenteric cyst by suturing its edges to the skin [4, 5]. Wiesen et al. [5] reported the complete enteroscopic excision of a mesenteric chylous cyst developing into the lumen of the proximal jejunum. Some authors performed laparotomic or laparoscopic fenestration of the cyst, if it is located near a major abdominal vessel, but such a surgical option should be avoided due to the risk of malignancy [10].
In our first case, we performed the complete excision of the cyst by laparoscopy. The position of the trocars must be decided depending on the location of the tumor [3]. A second concern of the technique is the relation between the cyst and the major abdominal vessels. Our second case, with a huge retroperitoneal cyst highly interconnected with major abdominal blood vessels and a syncronous hiatal hernia, required a laparotomic approach. It is important in order to avoid any risk of chylous fistula to accurately seal and divide any vessel of the cyst. However, the chyle leakage from the cyst does not represent any particular concern, as long as the surgeon can accurately wash the surgical field and eventually insert a drain (see Fig. 3).
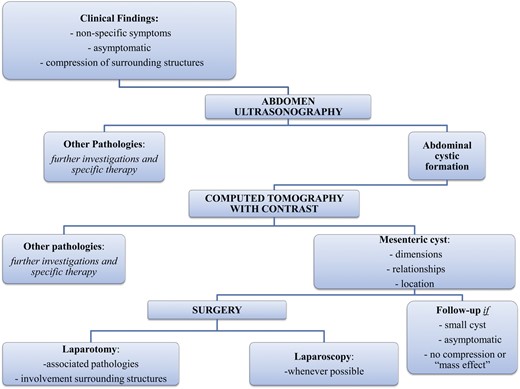
Chylous cyst could be totally asymptomatic or present with unspecific abdominal symptoms. It is a rare disease, but surgeons must consider the diagnosis in the presence of a cystic abdominal tumor.
The first-choice therapy is the complete removal of the cyst, which must be accurately planned according to the anatomy of the lesion, its dimensions and its relationships with major abdominal structures.



