-
PDF
- Split View
-
Views
-
Cite
Cite
Edward Rawstorne, Christopher J. Smart, Simon A. Fallis, Nigel Suggett, Component separation in abdominal trauma, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt133, https://doi.org/10.1093/jscr/rjt133
Close - Share Icon Share
Abstract
Component separation is established for complex hernia repairs. This case presents early component separation and release of the anterior and posterior sheath to facilitate closure of the abdominal wall following emergency laparotomy, reinforcing the repair with a biological mesh. On Day 11 following an emergency laparotomy for penetrating trauma, this patient underwent component separation and release of the anterior and posterior sheath. An intra-abdominal biological mesh was secured, and the fascia and skin closed successfully. Primary abdominal closure can be achieved in patients with penetrating abdominal trauma with the use of component separation and insertion of intra-abdominal biological mesh, where standard closure is not possible.
INTRODUCTION
Component separation is a surgical technique that permits large complex abdominal wall hernia to be repaired. The technique separates the muscle components of the abdominal wall, so that they can be mobilized and used to reconstruct midline deficiencies of the abdominal wall [1]. The external oblique aponeurosis is released from the linea semilunaris which enlarges the musculofascial surface area and allows for the rectus abdominis to be mobilized centrally [2]. This has achieved good results with acceptable hernia recurrence rates of 9–32% [3, 4]. Studies have shown lower rates of recurrence with reinforcing the repair with a biologic mesh [5, 6].
Component separation was initially described as an elective technique for closing abdominal wall deficiencies resulting from previous surgery or trauma [7, 8]. It has since been described as an early technique (within 6 days) for closure of the open abdomen in patients suffering severe burns requiring a decompressive laparotomy [9]. This case reports early component separation for closure of the abdominal wall following emergency laparotomy for penetrating trauma.
CASE REPORT
A 51-year-old male received a penetrating stab wound to the abdomen and underwent an immediate emergency laparotomy. Findings at laparotomy were splenic hilar injury, a through-and-through enterotomy of the stomach and transection of the left renal vein. The stomach was repaired, a splenectomy was performed and ligation of the left renal vein was undertaken with temporary clamping of the aorta. The abdomen was packed, and a temporary topical negative pressure closure of the abdomen was undertaken. The patient required 24 units of packed red cells, 20 units of fresh frozen plasma and 4 units of platelets to achieve resuscitation. Twenty-four hours later, the patient was returned to the operating room for a relook laparotomy. The transverse colon had patchy ischaemia, so a damage control resection of the colon was undertaken. Minor bleeding points on the abdominal wall were controlled. The topical negative pressure closure was reapplied. On the fourth postoperative day, a second relook laparotomy was undertaken. The colon was anastomosed. The abdomen was unable to be closed, and the topical negative pressure dressing was reapplied. On the ninth postoperative day, a further attempt was made to close the abdomen but this was not successful. The topical negative pressure closure was reapplied.
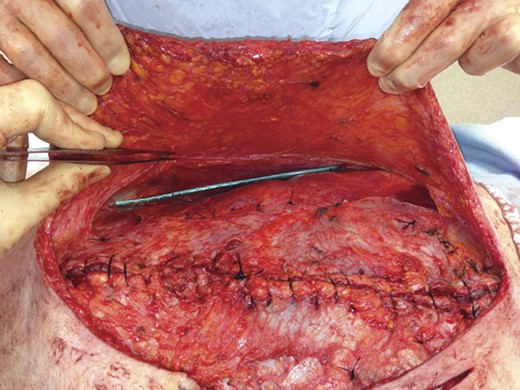
On the 11th postoperative day, a component separation was performed. The topical negative pressure dressing was removed leaving the defect shown with the anterior sheath retracted away from the midline (see Fig. 1) . The overlying skin was released bilaterally from the abdominal wall, and the anterior rectus sheath was released. To achieve this, the external oblique was incised at Point A, and the incision taken high to the costal margin and as low as possible to allow maximal release. The internal oblique is then exposed (Point B), and the released edge is visible at Point C (see Fig. 2).

Defect following removal of topical negative pressure dressing.
![Component separation showing the released anterior sheath [(A) incised external oblique aponeurosis; (B) internal oblique; (C) released edge of external oblique aponeurosis].](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2014/1/10.1093_jscr_rjt133/2/m_rjt13302.jpeg?Expires=1772271898&Signature=Kwe~67yq6I4bpNCk7uDUeJrunlHPHPtlxohXHfESZmsxBqMca0dns0-brIK6MIBStKgLB0hAlSiytcQg-2TULPq24tBNpDCBxQT-NP88kCGk3KIXgH7o7O2IrwyGzbEXzz3nBhxNWx0O0En6HHV8xzd8E70ykVGXB~FgR82VtOdHgPlsHkDJlpnisEhy5cof5GMK8CCYiwkeZ-G7d3LJ0GRtKx0WDN-0LcOJUPYN57SOrUxrsOLbKB5M7il9mWafIhhr9HoqXy~LsAtlIyk-xEpUwaSvG~13wJCXhhn9XamwgtoXePQqV3m0JiAi12HGMTpzlIYXALSdBBN5qYXyxw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Component separation showing the released anterior sheath [(A) incised external oblique aponeurosis; (B) internal oblique; (C) released edge of external oblique aponeurosis].
A posterior sheath release was then performed to provide medial movement of the sheath, so that it could be closed in the midline (see Fig. 3). A 25 × 25-cm biologic mesh (Strattice™ Reconstructive Tissue Matrix,–LifeCell Corp.) was rotated to a diamond shape and secured in the pre-peritoneal space, to the lateral fascia (see Fig. 4). The rectus muscle was closed, and the component separation allowed for the anterior sheath to be closed in the midline (see Fig. 5). Primary skin closure was undertaken, and the patient returned to the ward.


The rectus muscle has been closed, and a drain is placed prior to closing the skin.
On the 16th postoperative day, he suffered a witnessed ventricular fibrillation cardiac arrest. He was resuscitated and subsequently anticoagulated. The following day a computed tomography scan revealed a large abdominal wall haematoma anterior to the rectus sheath. He returned to theatre on the 17th postoperative day. The fascia was found to be intact, and the haematoma evacuated. Topical negative pressure was reapplied. On the 21st postoperative day, the skin was reclosed. He returned to the ward and was discharged on the 49th postoperative day, following implant of a cardiac defibrillator, with an intact wound (see Fig. 6).

DISCUSSION
This case presents an abdomen following penetrating trauma that was difficult to close on a number of occasions. The aim of closure was to prevent a prolonged open wound managed with vacuum assisted closure. The option of using a biologic mesh as a bridge between the fascia was considered, but this would have made it much more difficult to achieve skin closure and increased the chances of recurrence requiring a second definitive repair 6–12 months in the future. The primary closure of fascia was undertaken to protect against the need for further surgery [10]. The advantages of this repair were that no further surgery was required, after this patient was discharged. The disadvantages of this repair are that it may have resulted in abdominal compartment syndrome unlike vacuum assisted closure that provides a steady and slow abdominal closure. The cause of the cardiac complication in this patient is unknown, but the resulting anticoagulation resulted in significant bleeding from the abdominal wall that required evacuation of the haematoma. It serves as a reminder that these patients may have comorbidities that influence choice of abdominal wall closure and, in the initial stages following trauma, the minimum is often best. This patient was successfully discharged and was well with no evidence of recurrence at 6-month follow-up.
Primary abdominal closure can be achieved in patients with penetrating abdominal trauma, where standard closure is not possible with the use of component separation and insertion of pre-peritoneal biological mesh.



