-
PDF
- Split View
-
Views
-
Cite
Cite
Renato P.M. Neves, Vânia C. Oliveira, Luís M.D. Costa, Daniel F.E. Soares, Pedro F.F. Cardoso, Paulo G. Costa, Joaquim F.S. Lopes, Major complications following total en bloc spondylectomy for giant-cell tumor, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt131, https://doi.org/10.1093/jscr/rjt131
Close - Share Icon Share
Abstract
The authors present the case of a 32-year-old Caucasian female with a giant-cell tumor of the eighth thoracic vertebra, causing unremitting pain, segmental kyphosis and imminent local instability. A total en bloc spondylectomy by a posterior-only approach was performed, complemented with anterior-column reconstruction with a titanium mesh and structural allograft, as well as pedicle screw fixation. Despite the surgery being uneventful, several complications developed over the ensuing weeks: bilateral hemothorax, empyema and sepsis, requiring numerous revision surgeries for postoperative infection. The same pathogen was identified in different samples collected, including a sample from the allograft used. Only the aggressive therapeutic measures adopted allowed improvement in clinical and analytic parameters. The present report alerts to the possible complications following major spine surgery, and raises concerns on the safety of the bone allografts provided, renewing the interest in the development of alternative bone substitutes.
INTRODUCTION
Traditional excision of primary or metastatic lesions involving the spine was based on local curettage or piecemeal resection [1]. However, these techniques show obvious disadvantages, mainly because of the higher risks of local contamination by neoplastic cells and the inability to completely remove the lesion. These factors contributed to high local recurrence rates [2].
The first case of a total en bloc spondylectomy is attributed to Bertil Stener in 1971, but it was only in 1994 that larger series were published by Tomita et al. as well as Fidler [3]. According to the technique described by Tomita, it is possible, by means of an isolated posterior approach, to complete an extra-lesional excision with adequate histological margins, allowing a potentially curative treatment [4].
CASE REPORT
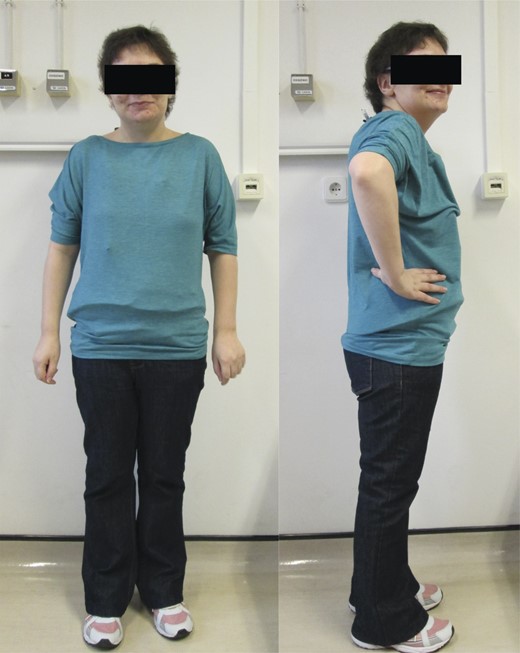
We present the case of a 32-year-old female, referred because of pain localized in the mid-dorsal region, with onset several months earlier and progressive worsening. The pain aggravated with local palpation and trunk movement. Lately, she also manifested weakness in the lower limbs.
The radiographic study identified an expansive lesion in the eighth thoracic vertebra (T8), with local kyphosis and imminent instability. She performed a computed tomography (CT) scan and magnetic resonance imaging (MRI), which better defined the bone involvement and already revealed invasion of the medullary canal (Fig. 1). A percutaneous CT-guided core-needle biopsy was then undertaken, and the histologic report confirmed the diagnosis of giant-cell tumor.

Preoperative imagiologic study; involvement of T8 by the giant-cell tumor as presented in plain radiograph (A), CT scan (B) and MRI (C and D). Notice the tumor mass protruding into the vertebral canal.
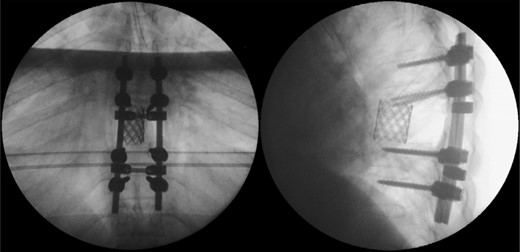
Due to the advanced stage of the lesion, with associated instability that could result in major neurologic deficits in a short time period, a total en bloc spondylectomy of T8 by a posterior-only approach was performed (Fig. 2). The operation followed the technique proposed by Tomita et al. and was complemented with anterior-column reconstruction with a titanium mesh filled with structural allograft, as well as pedicle screw instrumentation, from T6 to T10 (Fig. 3). During the procedure, the eighth dorsal nerve routes were sacrificed.
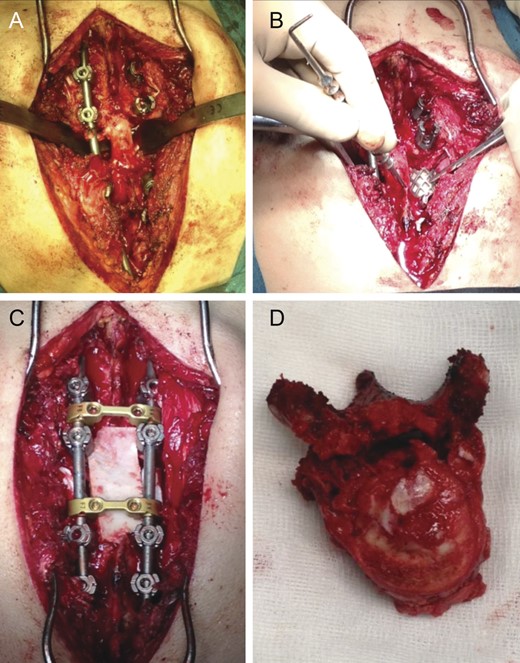
Intraoperative photographs; after total en bloc spondylectomy (A), anterior-column reconstruction was accomplished with placement of a titanium cage with structural allograft (B) and was complemented with pedicle screw-rod fixation (C). (D) Resected vertebra.
The surgery went uneventful, taking 5 h to complete. The immediate postoperative period was favorable, without reported neurologic deficits (besides the ones attributed to T8 nerve root ligation).
The patient started the pulmonary rehabilitation protocol by the second postoperative day, showing encouraging progression. However, by the third day, she initiated complaints of progressive dyspnea with associated impaired gas exchange. A CT scan confirmed bilateral hemothorax requiring bilateral thoracentesis (Fig. 4), after which she immediately recovered from the previous symptoms.

It was only by the 19th postoperative day, which the patient showed worsening of her general status with fever, dyspnea, decreased gas exchange and an increase in inflammatory markers. A new CT scan was performed, revealing a moderate fluid collection in both lungs, compatible with empyema (Fig. 5). The patient evolved to a septic state, which required her to be transferred to the intensive care unit.

Postoperative thoracic CT scan; large septated empyema, extending from the surgical site to both pleural cavities, was found to be the cause of deterioration of the patient's general condition.
Due to the ongoing postoperative infection, a new operation was undertaken with surgical debridement of the infected tissues, allograft and titanium mesh extraction, which were replaced by iliac crest tricortical autograft for anterior support (Fig. 6). The posterior pedicle instrumentation was kept, after copious irrigation of the surgical wound. Drains were placed in the thoracic cavity and paravertebral spaces.
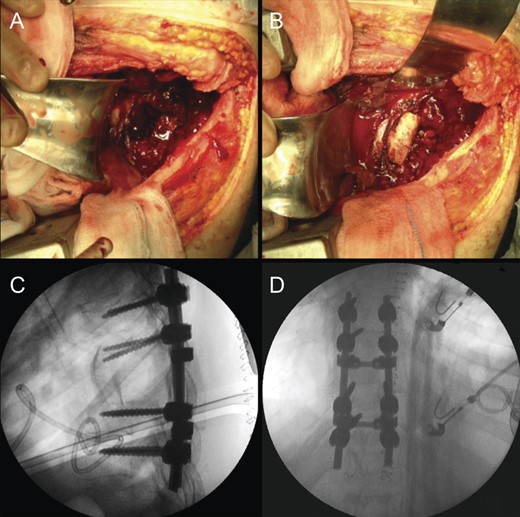
Revision procedure; a thoracotomy was performed for pus drainage and debridement, as well as removal of the anterior cage and allograft (A). A tricortical iliac bone autograft was used to maintain anterior-column stability (B). Postoperative radiographic study (C and D).
Blood cultures, as well as those from pus samples collected intraoperatively and from the explanted mesh and allograft identified Enterobacter aerogenes as the pathogenic agent. The same bacterium was isolated in a sample of allograft sent for cultures on the day of the index operation. A pathogen-directed course of i.v. antibiotic therapy was initiated.
Ten days after the revision operation, the patient was diagnosed with a lower respiratory tract infection, with Acinetobacter baumannii being identified in sputum samples.
Concurrently, a newly resurged septated empyema had developed in the paravertebral space, which demanded for a combined anterior and posterior approach, for complete drainage (Fig. 7). Twelve days later, an additional posterior open drainage was necessary to address a subcutaneous abscess. Samples collected intraoperatively from this last operation isolated methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa as pathogens.
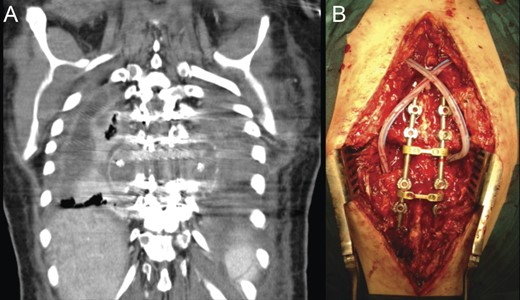
(A) CT scan coronal reconstruction showing recurrence of paravertebral empyema. (B) Intraoperative image following posterior debridement.
The several complications sustained, as well as the prolonged hospitalization, took a significant toll on the patient, leading to considerable physical and psychological burden.
In response to the therapeutic measures adopted, there was a progressive improvement in clinical and analytic parameters, which allowed the discharge from the hospital, 79 days after initial admission. A custom-molded thoracolumbar brace was prescribed, as well as maintenance of physical therapy to regain muscle strength.
Currently, after 9 months from the initial surgery, the patient remains stable and asymptomatic with no evidence of infection or tumor relapse (Fig. 8). The follow-up imaging studies show encouraging evolution without bone graft resorption or failure of the instrumentation (Fig. 9).
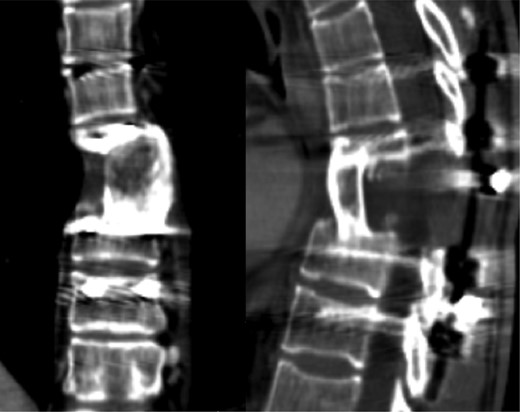
CT scan with no evidence of tumor relapse or instrumentation failure.
DISCUSSION
Giant-cell tumors of the spine, despite being considered benign and relatively rare [5], may become potentially aggressive, due to continuous growth and involvement of adjacent structures [6]. In the spine, this may lead to loss of segmental stability and potentially serious neurological deficits.
The underlying principle behind total en bloc spondylectomy is to allow complete resection of a tumor within its compartment, thus obtaining safe histological margins that reduce the local recurrence rate and improve the long-term survival, as has been confirmed by several published studies [3, 7–10].
Despite the stated potential benefits of this already well-established technique, it remains an aggressive procedure that can lead to serious complications, such as the ones mentioned that can threaten the patient's life.
In this case, the fact that the causing pathogen (E. aerogenes) was already present in the allograft used raises the concern about the quality of the bone allografts provided, and renews the interest in the development of alternative bone substitutes.
Total en bloc spondylectomy is regarded as a very demanding surgical technique, by the difficulty of execution and risks that entails [2]. Therefore, it should only be undertaken by highly trained spine surgeons. Nevertheless, it remains the best treatment option for selected cases (mainly primary tumors or limited metastatic lesions involving the spine), providing the best outcomes, as reflected by lower recurrence rates and the best long-term survival.
REFERENCES
- sepsis
- empyema
- bone substitutes
- giant cell tumors
- hemothorax
- pain
- reconstructive surgical procedures
- safety
- surgical mesh
- surgical procedures, operative
- thoracic vertebra
- titanium
- european continental ancestry group
- kyphosis
- acquired kyphosis
- congenital kyphosis
- pathogenic organism
- postoperative infections
- allografting
- spinal procedure
- spinal pedicle screw
- bone graft, allogeneic



