-
PDF
- Split View
-
Views
-
Cite
Cite
Andrea Della Chiesa, Beat Scherrer, Johannes J. Kuttenberger, Metastatic breast cancer in the mandibular condyle mimicking temporomandibular joint (TMJ) disease, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt130, https://doi.org/10.1093/jscr/rjt130
Close - Share Icon Share
Abstract
Metastases or tumour to the jaws are rare and those to the temporomandibular joint (TMJ) are even rarer. The symptoms like preauricular pain, swelling and clicking are generally associated with TMJ disease. But the same symptoms are also found in tumours of the jaws or other diseases. We report on the case of a 48-year-old woman with a 12-year history of breast cancer who was referred to our department for clarification of preauricular swelling and pain. The possible aetiology of TMJ disorders and the frequency and localization of metastases to the jaws are discussed.
INTRODUCTION
Preauricular pain and swelling are often caused by temporomandibular joint (TMJ) disorders, rarely these symptoms can also be caused by a tumour or infection [1–3].
Malignancy of the bone is caused more often by metastasis than by primary tumour.
Primary metastases to the jaw are rare. Of all the malignant tumours located in the maxilla and face only 1% are metastases and those in the mandibular condyle are even rarer [1].
In a retrospective study of metastatic disease in the jaw, 60% had no history of malignancy [2]. In one case, the first manifestation of the metastasis of a primary lung cancer was a non-reducible dislocation of the mandible [4].
The mandible is more often involved than the maxilla. The distribution of the metastases in the mandible forms an ‘M’ curve pattern, with a rare occurrence in the condyle [5].
The most frequent site of primary tumours which metastasize to the jaw are breast followed by lungs, kidneys, prostate and thyroid [2, 5].
CASE REPORT
A 48-year-old woman was referred to our clinic for clarification of a preauricular swelling, headache and pain of the right TMJ.
She had a 12-year history of metastatic adenocarcinoma of the left breast. Mastectomy, axillar lymphadenectomy and primary chemotherapy of the left breast had been performed. Due to distant metastases right adnexectomy and radiotherapy of the left iliac bone were done.
Because of multiple bone metastases the patient had also received hormone and bisphosphonate therapy.
Several months before referral the patient complained about symptoms in the right TMJ region and was then sent to an otorhinolaryngologist, who suspected a parotitis. The investigation with ultrasound showed a healthy parotid gland and an enlarged articular capsule. Aspiration cytology from the preauricular swelling was then performed. No malignant tumour cells were detected. After the aspiration she felt better and the swelling disappeared. The symptoms were interpreted as a degenerative arthritis.
Approximately 4 months later symptoms returned. A computed tomography (CT) scan of the head was ordered by the oncologist. An osteolytic lesion and partial sclerosis of the right condylar head and neck were found, as well as effusion in the right TMJ (Fig. 1). The signs were interpreted as arthritis of the TMJ.
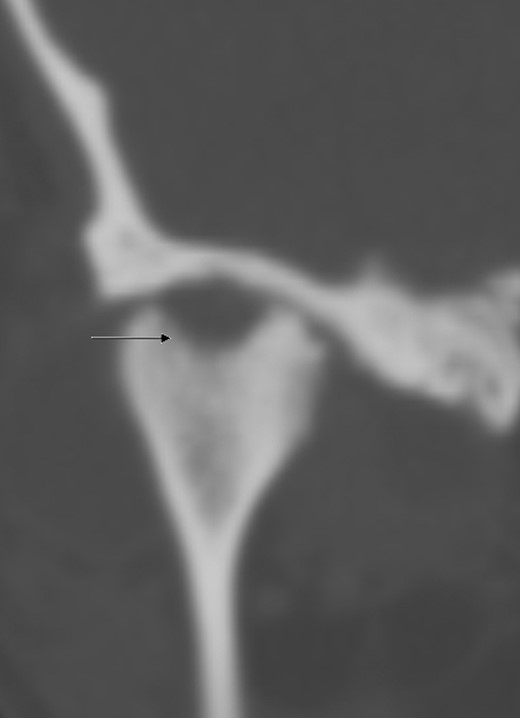
CT scan of the head (coronal section), arrow indicates osteolysis of the right condylar head.
Because of persistence of the swelling, massive preauricular and temporal pain and a slight impairment of mouth opening the patient was referred to us.
Clinically, a preauricular swelling on the right side which caused asymmetry was visible. The overlying skin was normal. Palpation was painful and consistence was fluctuant. No deviation was found at mouth opening. Mouth opening was 43 mm, but subjectively reduced. Occlusion was, despite the preauricular swelling, correct.
After clinical examination an magnetic resonance imaging (MRI) scan was done. A large joint effusion in the right TMJ was found and interpreted as an arthritis (Fig. 2).
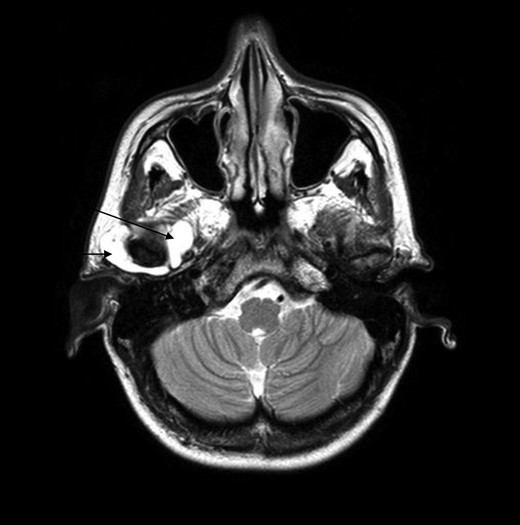
MRI scan, the arrows point out the huge effusion medial and lateral of the right TMJ.
Because of the history of breast cancer and the persistent pain and swelling, an arthrocentesis, lavage and application of 20 mg Kenacort into the right TMJ was performed. The histology showed synovial cells, hystiocytes, erythrocytes, but no malignant cells.
One week later there was no swelling visible and the patient was painless.
A full-body skeletal scintigraphy was done, which did not show an obvious pathology in the right TMJ (Fig. 3). Due to this, a SPECT/CT was performed for clarification. High uptake of nuclides was seen around the osteolysis of the right condyle (Fig. 4). Sclerotic changes without increased uptake were noted in the left condyle (Fig. 5).
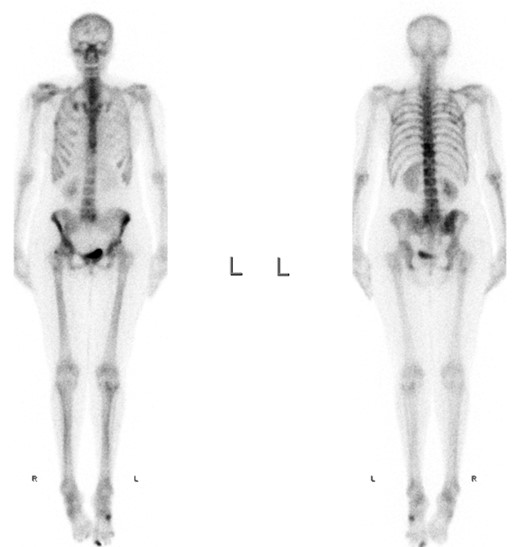
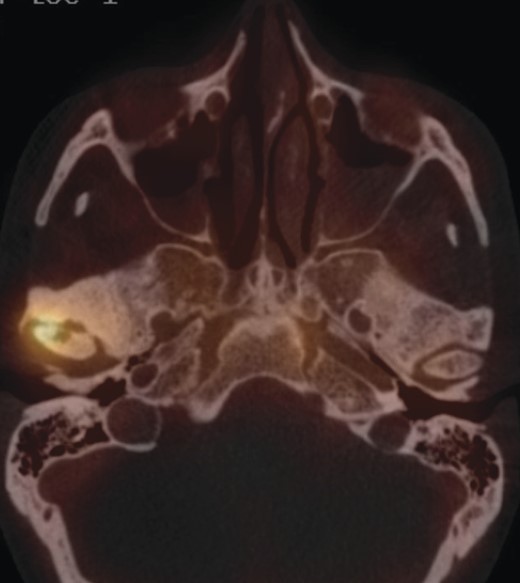

The sclerosis of the left TMJ was suspected to be a non-active metastasis.
In summary, from the radiological findings bilateral TMJ metastases were diagnosed, which were, however, not confirmed histologically.
Because of persisting symptoms in the right TMJ, a palliative radiotherapy was done to the right condyle with a total dose of 40 Gy (16 fractions). After that the patient was free of pain.
At the last clinical follow-up (November 2013) the patient was free of complaints and no swelling was detectable.
DISCUSSION
Although this case does not meet the Meyer and Shklar criteria [1] for considering the lesion in the mandibular condyle to be metastatic, for the patient's comfort no biopsy was taken. The radiological findings in the TMJ, however, were very similar to the metastatic changes on different skeletal sites and so bilateral TMJ metastases can be suspected.
In the majority of the cases malignant diseases in the oral and maxillofacial region are primary neoplasms, metastatic disease is rare [1]. Only two cases have been described with bilateral spread to the TMJ [6].
The involvement of the left TMJ is only suspected by the sclerotic change in the condylar head, whereas metastases to the right TMJ are highly probable.
In one-third of metastatic malignancies in the oral and perioral tissue the primary tumours are diagnosed after the metastases lead to symptoms [7].
Approximately 30% of the metastases to the jaw are caused by carcinomas of the breast [3].
Metastatic carcinomas are five times more common in the mandible compared with the maxilla [5].
The initial symptoms and radiographic signs of metastasis to the TMJ are not specific and can in 50% mimic other TMJ diseases [6, 8, 9].
A ‘preauricular swelling’ can, as in our patient, be one of the leading clinical signs, but it is however non-specific. There are multiple causes for preauricular swelling as arthritis/degenerative diseases, infections like Lues or tuberculosis, systemic disorders like hystiocytosis X [9], metastatic or primary tumour like Jacob's disease [10].
Radiological signs of metastases are often osteolytic. But there are also some osteoplastic tumours like prostate carcinomas or osteoplastic and osteolytic like in breast cancer [8, 9].
The typical sign for arthritic disease, along with swelling and pain, is abrasion [9]. As in our case these symptoms can also be present in metastases. Differentiation, however, between TMJ disorder and metastases to the condyle is difficult.
Local recurrence of the disease (cancer) or metastases can appear after a long period of disease-free survival [3]. In our patient the first metastases wwere diagnosed in 2003, 4 years after the primary tumour, and the symptoms in the right TMJ appeared in 2011.
The prognosis in patients with condylar metastases is bad, in 70% there were already other distant metastases [8].
Thus, in patients with TMJ disorder symptoms especially with a history of other malignancies, metastases always need to be considered.
Therapy in patients with condylar metastases is often palliative and the medium life expectancy is around 5 months [10].
The most frequent primary tumours with metastases to the jaw are in the order of frequency: breast, lungs, kidneys, prostate and thyroid.
Exclusion or diagnosis of metastases has to be done early so that no time will be lost for adequate therapy to increase survival and quality of life.
CONFLICT OF INTEREST STATEMENT
None declared.



