-
PDF
- Split View
-
Views
-
Cite
Cite
Pallipuram Seshadrinathan Bhageerathy, Maria Cecilia, Ajit Sebastian, Anantharam Raghavendran, Priya Abraham, Anitha Thomas, Abraham Peedicayil, Human papilloma virus-16 causing giant condyloma acuminata, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt126, https://doi.org/10.1093/jscr/rjt126
Close - Share Icon Share
Abstract
A 28-year-old multiparous lady presented to the Gynaecology outpatient department with a 12 × 5 cm warty growth in the vulva. A biopsy of the growth revealed condyloma acuminata of the vulva. Simple vulvectomy was done. A PCR of the specimen detected the presence of human papilloma virus (HPV)-16 which is usually considered as a high-risk HPV type for carcinogenesis.
INTRODUCTION
We report a case of giant condyloma acuminata of the vulva in a 28-year-old immunocompetent female patient caused by human papilloma virus (HPV)-16. She was treated successfully with simple vulvectomy
CASE REPORT
A 28-year-old multiparous lady, married at the age of 18 years and having 2 living children presented to the Gynaecology outpatient department with a growth in the vulva. The lesions started 6 months earlier as pin-sized papules in her labia majora and fourchette, associated with itching. They gradually increased in size and eventually coalesced to form large tufts. There was no history of coital dysfunction or postcoital bleeding. She had no menstrual complaints, neither did it interfere with her bladder and bowel function.
Her husband was examined and found to be free of any gross lesions. The lady denied any history of extra-marital sexual contact or assault.
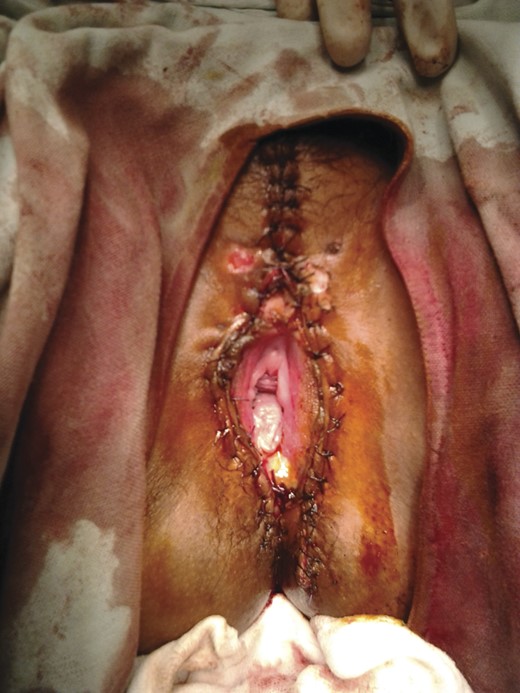
Examination of the lesion revealed a 12 × 5 cm warty growth, with a cauliflower-like surface, arising from right and left labia majora and minora. Similar lesions were also present on the clitoris with additional satellite lesions scattered around the perineum, perianal region and lower vagina. Upper vagina and cervix appeared normal (Fig. 1).

A Papanicolaou cervical smear was performed which revealed no abnormality. Her HIV, HBsAg and VDRL status were negative. Her haemoglobin was 10.9 g%. A biopsy, under local anaesthesia, was performed (to rule out verrucous carcinoma) which was reported as condyloma acuminata.
The lady underwent a simple vulvectomy under spinal anaesthesia. Labia majora and most of labia minora were excised sparing the clitoris. Lesions on the perianal areas were also excised. Smaller lesions were cauterized. Wound was closed with 2-0 vicryl. Post-operatively, ice dressing was applied to the wound (Fig. 2).
The post-operative period was uneventful and sutures were removed on 10th postoperative day.
The histopathological examination of the specimen was reported as condyloma acuminata with no evidence of malignancy. A PCR of the specimen revealed the presence of HPV-type 16 PGMY CHUV assay was performed on the sample to rule out mixed infection and the presence of only HPV-16 was confirmed [1].
Follow-up after 1 year did not reveal any new lesions.
DISCUSSION
Condyloma acuminatum is a sexually transmitted disease caused by HPV infection. HPV is an epidermotropic DNA virus which causes various benign and malignant lesions involving the anogenital region. Almost 120 types of HPV have been identified, of which 40 of them primarily infect the squamous epithelium of lower anogenital tract of men and women [2].
HPV types are classified based on their oncogenic potential into low- and high-risk types. HPV types 6, 11, 40, 42, 43, 44, 53, 54, 61, 72, 73 and 81 belong to low-risk group and types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68 belong to high-risk group [2].
Condyloma acuminata is commonly associated with low-risk HPV types 6 and 11. About 90% of genital warts are caused by HPV 6 and 11 [3]. Our case is unusual in that HPV-16 which is considered high-risk type for carcinogenesis was found to cause condyloma acuminata. A detailed literature search revealed a case of HPV-16/18 associated condyloma acuminatum of urinary bladder [4], but we could not find any other case reports of HPV-16 causing anogenital condyloma acuminata.
HPV-16 is the most common HPV found in invasive cancer, CIN 2 and CIN 3. It is responsible for ∼50% cases of carcinoma cervix [5].
Giant condyloma acuminata, also known as Buschke–Löwenstein tumour has an incidence of 0.1% in the general population with a male-to-female ratio of 2.7:1 [6]. It is characterized by a high recurrence rate after treatment. Malignant transformation into squamous cell carcinoma has been reported [7]. But foci of invasive cancer in giant condyloma specimen are found to be of uncertain significance and do no correlate with prognosis or recurrence [7]. Local invasion and recurrence are the major causes of morbidity in these patients. The preferred initial therapy is complete excision whenever feasible.
Various treatment modalities have been described, but surgical excision with wide margins is the only definitive treatment [8]. Virostatic agents such as podophyllin, colchicine, 5-FU, BCG and interferon can be used as adjuvant therapy especially in high-risk HPV types [8]. As relapse and even malignant transformation of condyloma have been reported, close follow-up and annual Pap smear are recommended, especially, for lesions positive for high-risk HPV types. The HPV vaccine could lead to a potential reduction in the incidence of genital warts as well as cervical, anal, vulvar, vaginal and penile cancers and its precursor lesions [9]. Just as current HPV vaccines will not prevent all cervical cancers, the quadrivalent vaccine will not prevent all cases of genital warts.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare. Institutional Ethics Committee approval and patient's consent has been obtained.



