-
PDF
- Split View
-
Views
-
Cite
Cite
Takeshi Kondo, Placental infarction probably associated with late term premature delivery, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt125, https://doi.org/10.1093/jscr/rjt125
Close - Share Icon Share
Abstract
Here the histopathology findings of placental infarction associated with late preterm birth are reported. The subject was a male neonate delivered at 34 weeks and 5 days of gestation with a birth weight of ∼2500 g. His mother had been diagnosed with a threatened premature birth at 27 weeks of pregnancy. The size and weight of the placenta was considered appropriate for gestational age. On the cut surface of the placenta, a white-colored focal infarct was noted beneath the site of the umbilical cord insertion. There were small focal infarcts scattered within the marginal area. There were no particular vascular abnormalities or apparent thrombi. The placental villi were of appropriate maturity for the gestational age and the villous vessels showed no structural abnormalities. This case highlights the benefits of examining the histopathology of postpartum placentas for preterm children to explore their significance in premature birth.
INTRODUCTION
Premature birth is a leading cause of infant mortality in developed countries. Although it has been studied extensively, its pathogenesis remains largely unknown [1]. In recent years, late preterm birth (34–36 gestational weeks) has been gaining more attention [2]. The placenta is a record of the fetal environment and its examination may provide information about fetal growth and subsequent development [3]. Detailed placental histopathology is needed, especially for cases of preterm birth. Here I report the histopathology findings of a case of placental infarction associated with late preterm birth.
CASE REPORT
The subject was a male neonate delivered at 34 weeks and 5 days of gestation with a birth weight of ∼2500 g. His mother had been diagnosed with threatened premature birth at 27 weeks of pregnancy. The child showed no apparent congenital abnormalities at birth and no noteworthy developmental problems appeared thereafter.
After standard formalin fixation, the placenta was examined histopathologically. The placenta was ∼19 cm in diameter and its weight was considered appropriate for gestational age (no measurement data are available). There were no obvious abnormalities in its gross appearance. The umbilical cord was inserted centrally (Fig. 1A). On the cut surface of the placenta, a white focal infarct was noted beneath the site of the umbilical cord insertion (Fig. 2A). There were small focal infarcts scattered within the marginal area, but these findings are generally not considered abnormal (Fig. 2A and B).

Gross appearance of the formalin-fixed placenta, viewed from the fetal side (A) and the maternal side (B). No macroscopic abnormalities were detected.
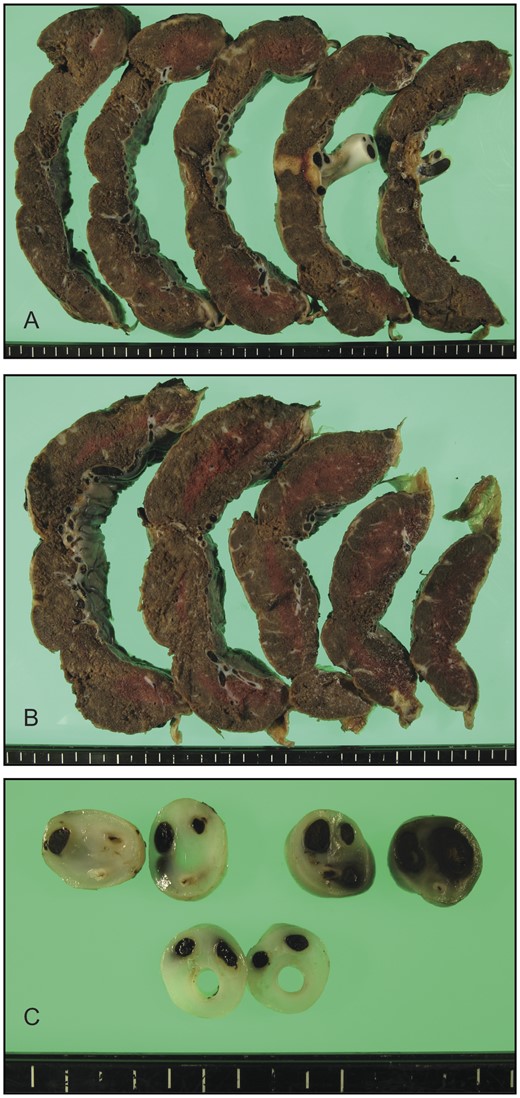
Cross-sectional views of the formalin-fixed placenta. (A and B) Focal infarct was detectable immediately beneath the site of umbilical cord insertion. (C) Cross sections of the umbilical cord depicted no structural abnormalities.
Microscopy confirmed the presence of focal infarcts, but no massive fibrin depositions were seen (Fig. 3A and B). There were no particular vascular abnormalities or apparent thrombi were detected. The placental villi were of appropriate maturity for gestational age and the villous vessels showed no structural abnormalities (Fig. 4A). No signs of chorioamnionitis were detected (Fig. 4B). No signs of funisitis or structural abnormalities were identified in the umbilical cord, which had two arteries and one vein (Fig. 4C). Using immunohistochemistry, the villi showed minimal immunoreactivity for complement split product C4d (Fig. 5).
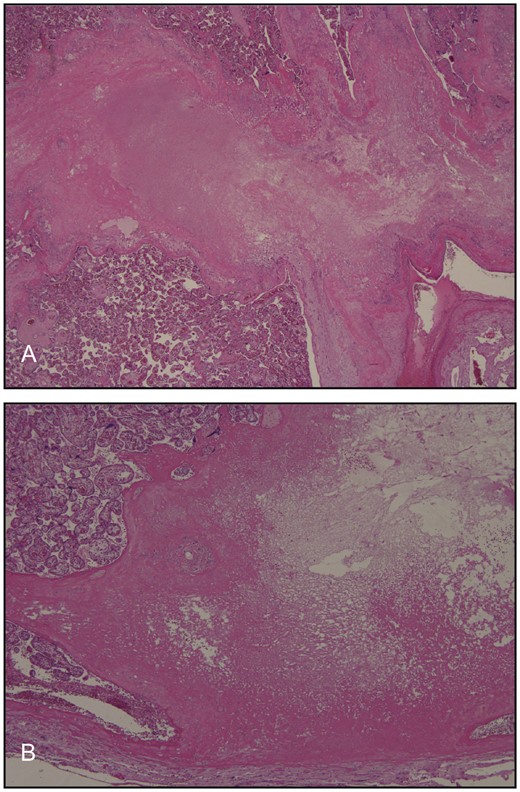
Histologic images corresponding to the placental infarcts shown in Fig. 2A.
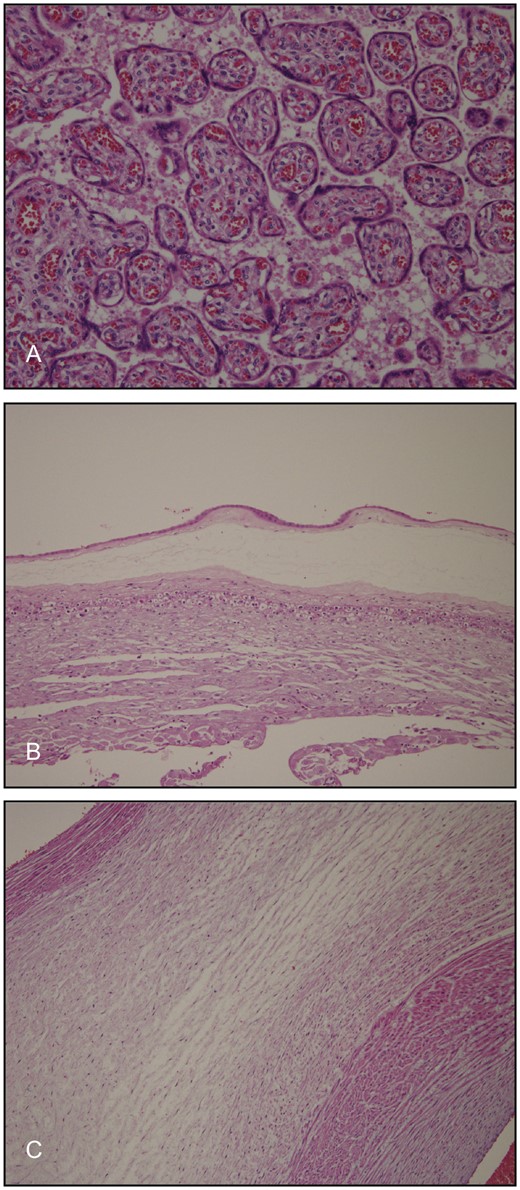
Microscopic images of the villous structures. The villi were of appropriate maturity for gestational age and the villous vessels showed no structural abnormalities (A). Histopathology revealed no signs of chorioamnionitis (B) or funisitis (C).
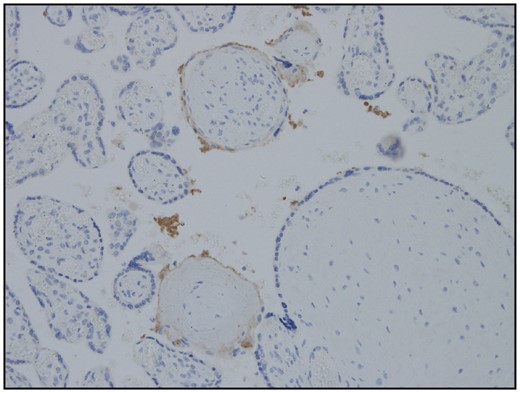
Immunohistochemistry showing minimal positivity for complement split fraction C4d.
DISCUSSION
A review of the available literature identified only a limited number of studies on placental histopathology findings related to threatened preterm birth. Several studies found marginal insertion of the umbilical cord at the periphery of the placenta in association with intrauterine growth restriction and premature labor. However, this feature was not present in this case.
Placental infarcts suggest poor perfusion of the fetoplacental unit [3]. The presence of infarcts—regardless of size—in the placenta of a preterm infant is an abnormal finding. Therefore, the size of infarcts and the timing of their formation are likely to have important clinical implications. It is generally assumed that central infarcts are more important than peripheral ones, and there is an association between pregnancy-induced hypertension and multiple placental infarcts. However, the mother in this case did not have hypertension. In addition, microscopy revealed no particular vascular abnormalities in the placenta and no thrombus formation.
Overall, these findings suggest that one or more humeral factors might contribute to the pathogenesis of threatened preterm delivery. In particular, we speculate that some thrombogenic factors are involved in the formation of placental infarcts. The placenta reported here had focal infarct just beneath the umbilical cord insertion and this observation suggests that thrombosis possibly led to the premature labor through various unknown mechanisms.
Complement fraction C4d, on the other hand, is commonly referred to as an indicator of antibody-mediated tissue injury [4]. The minimal expression of C4d in this case might give insight into placental infarction from the immunologic point of view.
Since not all placentas of preterm infants are investigated histopathologically, the presence of placental infarcts might go unnoticed for a considerable proportion of preterm children. In addition, the placentas of normal children are rarely examined. It is important to comprehensively evaluate placental pathology in the context of placental infarction. All pathomorphologic changes (pathomorphome) in placentas including those of normal infants should be analyzed routinely.
This case highlights the benefits of histopathology for postpartum placentas (evidence of fetomaternal interface) for both normal and preterm children to explore their possible causative significance in premature birth.



