-
PDF
- Split View
-
Views
-
Cite
Cite
Florian F.P. Proescholdt, Markus M.M. Markart, Wolfgang W.E. Ertel, Postoperative radiotherapy in diffuse idiopathic skeletal hyperostosis: prophylaxis of recurrence after resection of osteophytes from C3 to C5 in a case of dysphagia, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt124, https://doi.org/10.1093/jscr/rjt124
Close - Share Icon Share
Abstract
In diffuse idiopathic skeletal hyperostosis (DISH), recurrence of hyperostosis after surgical removal is common. While both non-steroidal anti-inflammatory drugs (NSAIDs) and radiotherapy have been used in the prevention of heterotopic ossification, only NSAIDs have been applied for prophylaxis in DISH. As a previously undescribed prophylaxis of recurrence in DISH, we report a case treated with local radiotherapy.
INTRODUCTION
Diffuse idiopathic skeletal hyperostosis (DISH) is a common disease in which tendons and capsules are subject to calcification leading to hyperostosis and functional impairment. Diagnosis of DISH is established by the presence of both spinal and extraspinal radiographic characteristics. Typical appearance of the cervical spine includes irregular and pointed osseous appositions of the superior and inferior vertebral margin [1]. The key organ is the enthesis, where calcification occurs under yet incompletely identified circumstances. Among the abnormal conditions occurring in patients suffering from DISH, the elevated levels of insulin-like growth factor I and hyperinsulinaemia are observed. Dickkopf-1 (DKK-1), a recently identified inhibitor of osteoblast differentiation, may be a key player in the formation of osseous appositions [2].
Epidemiologically, DISH is associated with metabolic syndrome and a risk of coronary heart disease [3]. Interestingly, the presence of radiographical features of DISH does not correlate with back pain [4]. In severe cases, dysphagia may occur and surgical treatment is required [5]. Conservative treatment includes anti-inflammatory drugs and corticosteroids [6].
A study observing the long-term outcome of surgical treatment showed recurrent dysphagia 10 and 11 years after surgery in 2 of 7 patients, one of them requiring renewed surgery. While only two patients were symptomatic, radiological follow-up showed recurrent hyperostosis in all patients who had undergone surgical resection. Spinal segments without mobility were less prone to recurrent hyperostosis than mobile segments [7].
Heterotopic ossification after orthopaedic trauma is a common problem following accidental or surgical trauma to joint regions. Frequently affected regions are hip and elbow. In prophylaxis of heterotopic ossification, both non-steroidal anti-inflammatory drugs and radiotherapy are efficient [8].
So far, there has been no report of radiotherapy for prophylaxis of relapse in diffuse idiopathic skeletal hyperostosis.
CASE REPORT
A 77-old-female with type 2 diabetes, arterial hypertension, obstructive sleep apnoea syndrome, atrial fibrillation and chronic kidney disease presented to the hospital with progressive dysphagia over a period of 6 months, currently of Mellow grade 2. She complained neither of neck pain, nor pharyngeal pain. Also, the history of present illness was negative for symptoms of malignant disease, trauma, cerebral ischaemia and surgical intervention. Clinical examination showed a mildly overweight female at a BMI of 33 with no external signs of obstructed oesophageal passage or respiratory distress. Neurological examination showed intact function of the cranial nerves. The preoperative Mallampati score was 2.
The X-ray and CT scan of the cervical spine revealed significant hyperostosis of the ventral cervical spine segments C3–C7. Hyperostosis was most extensive at segments C3–C5 causing stenosis of the pharyngeal lumen at the level of the larynx (Fig. 1). Due to accompanying joint pain, additional radiological examinations were performed. CT of the right shoulder showed extensive osseous proliferation of the medial humeral head reducing the articular space of the glenohumeral joint, as well as calcification of the rotator cuff (Fig. 2). In the left ankle, the CT scan revealed ossification of the deltoid ligament, and Kellgren grade 4 arthrosis of the tibiotalar and talocalcaneal joints (Fig. 3).

CT of the cervical spine in a sagittal view. Osteophytes of the ventral cervical spine segments C3–C5 protrude towards the oesophageal lumen.

CT of the right shoulder in a coronary plane. Hyperostosis is present at the medial side of the humeral head, as well as at the humeral insertion of the rotator cuff.
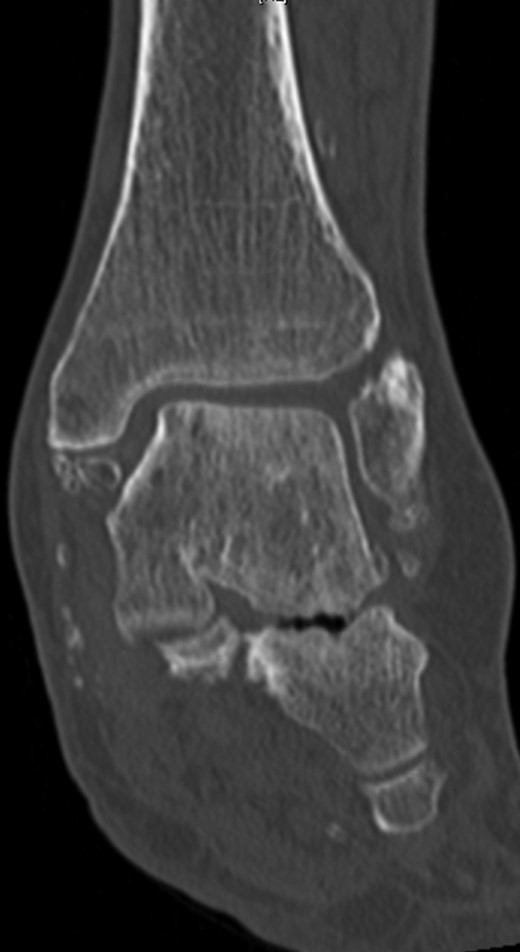
CT of the left ankle in a coronary plane. Ossification is present in the deltoid ligament. The tibiotalar and talocalcaneal joints show Kellgren grade 4 arthrosis.
Surgical access to the cervical spine through a right-sided standard anterolateral approach showed osseous vegetations, which were strongly attached to the ventral spine and caused ventral displacement of the oesophagus. There was no infiltration of neighbouring tissues. Hyperostotic tissue at levels C3–C5 was carefully removed. Within 24 h, a single-dose 6-MeV photon of 7 Gy was applied. Indometacin treatment was initiated with 50 mg twice daily. A control CT examination showed successful removal of hyperostosis from segments C3 to C5 with intact vertebrae and proper configuration of the cervical lordosis without signs of instability (Fig. 4).

CT of the cervical spine in a sagittal view. Osteophytes from C3 to C5 are removed. Sagittal alignment of the spine is preserved.
Dysphagia improved from the first postoperative day. Indometacin treatment was continued for 6 weeks. After 18 months dysphagia had regressed to grade 0 and there were no radiological signs of recurrence.
DISCUSSION
The patient in this case presented with a medical history common in DISH patients: obesity, arterial hypertension and type 2 diabetes mellitus. The symptoms—dysphagia and absence of neck pain—as well as the presence of extraspinal hyperostosis were typical [9]. Diagnostics were conducted with X-ray and CT scan according to the current standard. Surgical treatment is a standard procedure in severe dysphagia; it was performed without complications. Stability of the affected spinal segments was preserved protecting ligamentous structures during surgery. This was crucial since instability of spine segments after surgical resection of hyperostosis is a risk factor for recurrent ossification [7]. Radiotherapy of the affected segments was performed within 24 h. This has been described as a prophylaxis of formation of heterotopic ossification after orthopaedic trauma [8].
Eighteen months after surgery there were no clinical or radiological signs of recurrence. However, recurrence may occur up to 10 or 11 years after surgery. What makes this case unusual is the application of radiotherapy for prophylaxis from recurrence of ossification. Radiotherapy may provide protection from recurrence in DISH. However, further research is required in order to examine whether there is statistical significance.



