-
PDF
- Split View
-
Views
-
Cite
Cite
Tsukasa Nakamura, Shumpei Harada, Toshimasa Nakao, Koji Masuda, Gareth Wilkinson, Hirotaka Sako, Norio Yoshimura, Successful liver resection for the unusual case of peripheral intra bile duct growth of liver metastasis from colorectal carcinoma, Journal of Surgical Case Reports, Volume 2013, Issue 8, August 2013, rjt055, https://doi.org/10.1093/jscr/rjt055
Close - Share Icon Share
Abstract
Peripheral intrabiliary liver metastases (PILM) from colorectal carcinoma are rare, and this feature, which resembles primary cholangiocarcinoma, potentially misleads the accurate diagnosis and subsequent surgical treatment. A 67-year-old man with a medical history of descending colon carcinoma demonstrated an abnormal rise in CA19-9. There was a strong possibility of peripheral cholangiocarcinoma, because Computed tomography detected tumour infiltration into bile duct three. The patient underwent anatomic segment eight and lateral lobe resection. Pathological findings revealed that every tumour was metastatic liver carcinoma due to descending colon carcinoma. Cases of liver metastasis which resemble peripheral cholangiocarcinoma might be difficult to distinguish preoperatively. The correct diagnosis is important in making decisions regarding the surgical management of such patients. Nonanatomic hepatectomy is often performed for liver metastases from colorectal carcinomas. Anatomic hepatectomy, however, should be recommended in cases of PILM.
INTRODUCTION
Anatomical resection of the liver for metastases due to colorectal carcinoma is an estabished surgical procedure. Following the procedure, however, up to 80% patients develop intrahepatic recurrence [1]. Moreover, surgical margin recurrence, particularly at the edge of the Glisson pedicle, accounts for approximately one quarter of these cases [2, 3].
In the case of PILM, there is significant confusion between metastasis and primary intrahepatic cholangiocarcinoma. This is important as it can lead to a significant delay in the initiation of appropriate treatment [4, 5]. Nonanatomical hepatectomy could be recommended for liver metastases due to colorectal carcinoma [3, 6]. Given that intrabiliary tumour growth and surgical margin recurrence of Glisson's capsule, anatomical hepatectomy should be perfomed based on accurate pre-operative diagnosis.
CASE REPORT
A 67-year-old male patient underwent emergency left hemi-colectomy due to ileus caused by descending colon cancer. The pathological examination was consistent with adenocarcinoma (T3N1M0). Sixteen months following resection, there was a significant increase in routine follow-up carcinoembryonic antigen 19-9 (CA19-9): 607.7 U/ml.
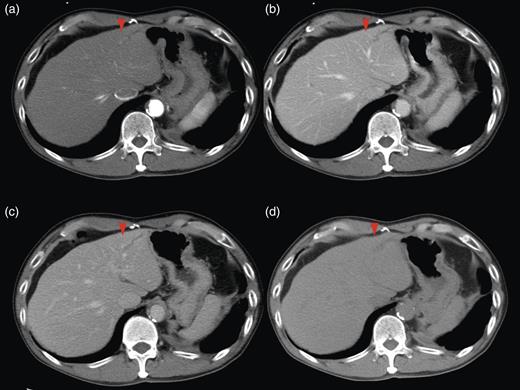
Computed tomography (CT) demonstrated two solitary lesions in segment (S) eight. Furthermore, S3 hepatic duct dilatation was clearly detected on CT scanning (Fig. 1).
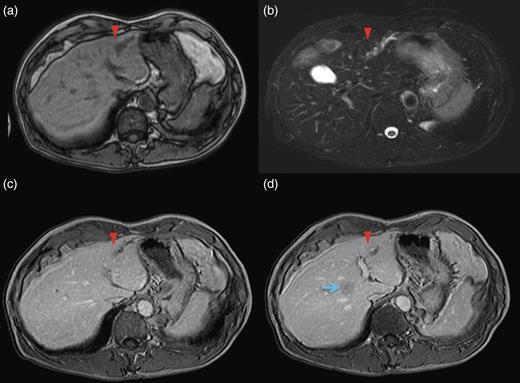
Magnetic resonance imaging (MRI) of the lateral segment lesion showed an irregular line shape lesion: hyper-intensity in T2-weighted; hypo-isointense in T1-weighted image (Fig. 2). These CT and MRI findings supported the identification of a fulfilment of tumour in B3. Endoscopic retrograde cholangiopancretography (ERCP) demonstrated a stricture involving the B2 and B3 hepatic ducts but not involving the left hepatic duct. Considering the patient's medical history along with the clinical features, the final diagnosis was secondary liver metastases due to primary descending colon adenocarcinoma, with the possibility of peripheral cholangiocarcinoma.
In order to obtain efficient bile duct tumour clearance as well as to maintain liver function (15-min retention rate of Indocyanine green: 19%), the patient underwent anatomic S8 resection and lateral segmentectomy (Fig. 3). The metastasis in the lateral segment demonstrated intra bile duct tumour growth.
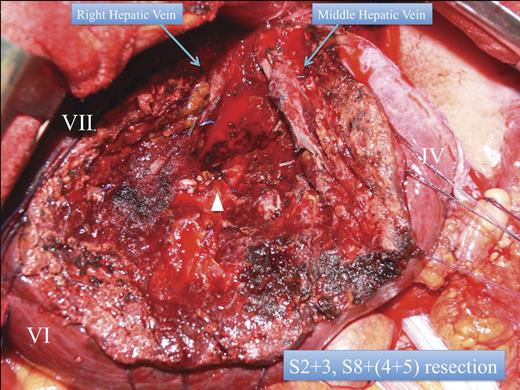
Anatomic lateral segmentectomy, and S8 segmentectomy. White arrow head: the right pedicle.
Although there was B3 intra bile duct growth, there was no pathological evidence of malignancy in the left main bile duct. For the S8 metastases, systemic S8 resection with indigo carmine S5 counter strain had also been performed. Subsequently, normal anatomic lateral segmentectomy was performed without extra hepatic bile duct resection or cholecystectomy. His clinical course was stable without complications, and he was discharged after 7-days of hospitalisation. The patient is currently suffering from amyotrophic lateral sclerosis, without any sign of local metastatic tumour recurrence 14 months post-operatively.
Pathological examination for the descending colon carcinoma revealed an adenocarcinoma which was well differentiated, with one out of ten lymph node metastasis identified (Dukes' C). Macroscopically, the surgical specimen of the liver demonstrated a papillary tumour with clear margin intra and extra hepatic duct growth. On microscopic examination, the histological differentiation of the three metastatic tumours was identical to that of the descending colon cancer. The lateral segment tumour was located in the intrahepatic duct which demonstrated cytokeratin (CK) 7(+), CK20(−) and caudal-type homeobox (CDX2) (−). These findings are consistent with liver metastases due to colorectal adenocarcinoma [7]. The S8 metastases did not reveal intra biliary tumour growth. Following this histological finding, the tumour invaded into hepatic duct, followed by the hepatic duct being filled with metastatic tumour at S3.
DISCUSSION
On pathological examination of surgical specimens, cases of liver metastases from colorectal carcinoma with intrabiliary growth account for more than 10% of the total caseload [4]. However, cases of liver metastasis which resemble peripheral cholangiocarcinoma are entirely rare and difficult to distinguish preoperatively. The correct diagnosis is important in making decisions regarding the surgical management of such patients in order to completely clear tumour infiltration. In addition to primary cholangiocarcinoma, other metastatic tumours such as those from bladder carcinoma should also be taken into consideration [8]. Whole-body imaging did not reveal any other abnormalities. Generally, in case of cholangiocarcinoma, CA19-9 (U/ml) tends to be higher than CEA (ng/ml) [9]. These results give further evidence of a diagnosis of cholangiocarcinoma with liver metastases. Despite the histological characteristics of the tumour, this type of metastases demonstrates a better prognosis compared with liver metastases without intrabiliary tumour growth [5, 10]. The typical pathological characteristics of liver metastases with intrabiliary growth are well or moderately differentiated tumours with a relatively long tumour-free period [5]. The mean duration of tumour-free period is 37.4 ± 25.4 months, which is longer than the tumour-free period of typical liver metastasis from colorectal carcinoma (6.1 ± 7.2 months) [5]. Furthermore, the 5-year survival rate is 80%, which is considerably higher than that of 57% in the case of liver metastases without intrabiliary tumour growth [4]. However, the recurrence rate with this type of tumour is high after surgical resection. In this case, because of combined liver metastases of typical type and the metastasis with biliary tract growth, pathological findings can be compared simultaneously. The tumour with intrahepatic duct growth was relatively well differentiated compared with other metastases.
With regard to surgical procedures for liver metastases due to colorectal carcinoma, nonanatomic partial hepatectomy is the most common surgical procedure [3, 6]. However, given the fact that around 10% of liver metastases from colorectal cancer demonstrate intrabiliary tumour growth [4, 5], it is reasonable to be more careful about performing nonanatomic hepatectomy. The decision of a surgical procedure for patients whose liver metastases clearly demonstrate intrabiliary growth will be anatomic hepatectomy. Nonanatomic partial liver resection is carried out in patients where investigations fail to reveal intrabiliary growth. If there was indeed growth in the biliary tract that was missed by imaging, there would be malignancy present after surgery.
In conclusion, generally, nonanatomic hepatectomy is performed for liver metastases from colorectal carcinomas. Anatomic hepatectomy, however, should be recommended in cases where preoperative imaging demonstrates intrabiliary tumour growth. It is reasonable, therefore, that liver metastases should be classified as non-intrabiliary growth type or intrabiliary growth type. Furthermore, it is of vital importance to take into account the discrepancy between preoperative diagnoses and pathological findings in regard to intrabiliary tumour growth.



