-
PDF
- Split View
-
Views
-
Cite
Cite
Fadil Khoyratty, Ahmed Sweed, Susan Douglas, Tawfik Magdy, Osteoma with cholesteatoma of the external auditory canal: neck manifestation of this rare association, Journal of Surgical Case Reports, Volume 2013, Issue 6, June 2013, rjt048, https://doi.org/10.1093/jscr/rjt048
Close - Share Icon Share
Abstract
Osteoma and cholesteatoma of the external auditory canal is a rare clinical finding, presenting specific challenges in patients suffering from this dual pathology of the ear. We report on a unique complication of this association in a patient suffering with recurrent neck abscesses. Neck disease secondary to cholesteatoma has become nearly extinct with better clinical imaging and sensible antibiotic usage.
INTRODUCTION
External auditory canal (EAC) cholesteatoma is a rare disease, with an estimated incidence of 0.1–0.5% in patients presenting with an otological complaint. An osteoma involving the EAC has been estimated to occur in 0.05% of patients having ear surgery. The chances of discovering an osteoma with underlying cholesteatoma of the EAC are rare, with only a few reports describing this association in the current literature [1].
With the advent of new imaging techniques and widespread use of antibiotics, the incidence of complications associated with cholesteatoma has decreased dramatically over the past 10 tears. As a result, neck masses secondary to aural cholesteatoma have become increasingly rare. A review of all published English literature (PubMed database) revealed only five reports (nine cases) identified before 1989, and no cases have been reported in the past 20 years [2].
CASE REPORT
A 24-year-old female with Rett syndrome developed recurrent unilateral neck abscesses over a 6-month period.
Rett syndrome is a severe neurodevelopmental disorder characterized by the progressive loss of intellectual functioning, fine and gross motor skills and communicative abilities, deceleration of head growth and the development of stereotypic hand movements, occurring after a period of normal development [3].
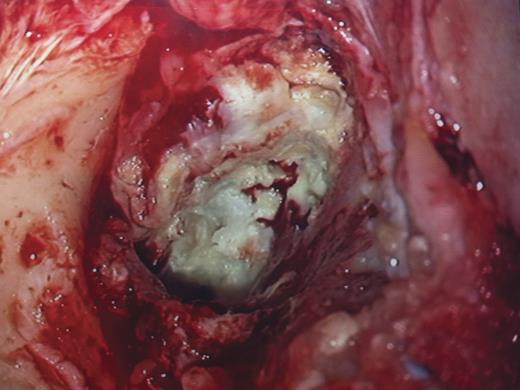
At initial consult, a 2 cm abcess overlying the left mastoid tip and a bony swelling arising from the EAC with overlying normal skin (Fig. 1) obstructing the view of the left ear canal and tympanic membrane was noted. Following incision and drainage of the abscess in theatre, the patient returned 2 weeks later with a self-draining left neck wound. As she was otherwise systemically well, the patient was treated as an outpatient with a course of oral antibiotics and listed for excision of the EAC osteoma and exploration of her left mastoid cavity. Due to the patient's global learning disabilities, audiological assessment and imaging of her ears were only possible under general anaesthesia. A combined decision was taken to proceed to surgical exploration, as it was felt that these adjunctive tests will not impact on her immediate management and would subject the patient to an additional anaesthetic challenge.

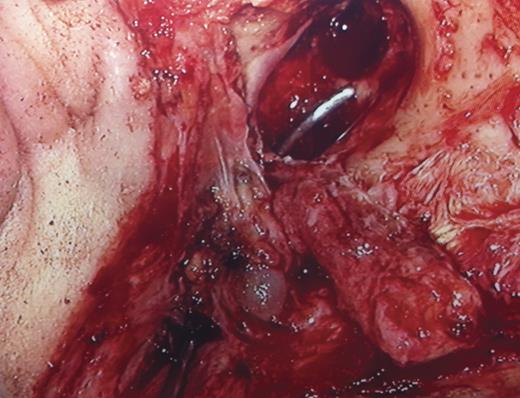
At surgery, transmeatal exicision of the EAC osteoma revealed an underlying cholesteatoma that has caused bony erosion of the inferior canal wall (Fig. 2) and formed a fistulous connection to the overlying neck skin (Fig. 3). The post-aural sinus and fistula were excised through a post-auricular incision. A cortical mastoidectomy was performed to explore the mastoid cavity, which was found to be disease free. The temporalis fascia was harvested and used to reconstruct the inferior canal wall defect. Histopathologic examination of the excised tissues confirmed the synchronous dual pathology involving the EAC (Figs 4 and 5).
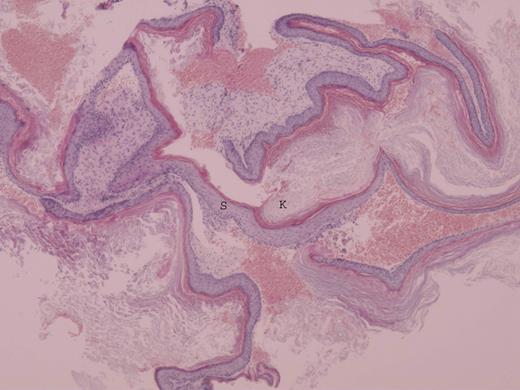
Photomicrograph of cholesteatoma showing stratified squamous epithelium (S) and overlying lamellar sheets of keratin (K) (H&E ×10).
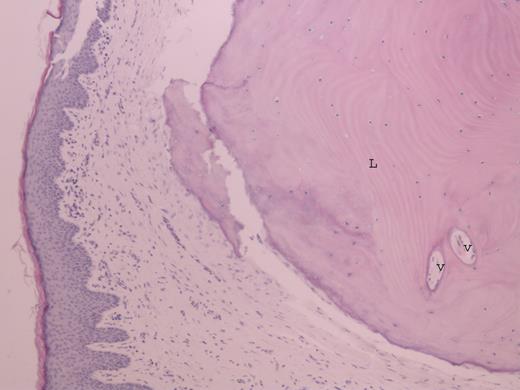
Photomicrograph of osteoma within the skin of external auditory canal showing lamellar bone (L) and fibrovascular channel (V) (H&E ×20).
The patient's symptoms settled after surgery and the neck abscess healed completely. There was no clinically detectable neck disease or cholesteatoma formation in the left ear canal at her 12-month clinic review.
DISCUSSION
The treatment of patients with EAC osteoma very much depends on the location, size and associated level of symptomatology. A symptomatic small EAC osteoma can be managed conservatively, whereas surgical excision would be warranted in cases where there is evidence of conductive hearing loss or recurrent infections secondary to a large obstructive bony canal lesion. A laterally based pedunculated osteoma would be easily reached transmeatally, wheareas a more medially located broad base osteoma would require a postauricular approach for complete exicision [4].
Although most osteomas are clinically indolent, the main complication associated with EAC osteoma is EAC cholesteatoma [1].Toynbee was the first to describe EAC cholesteatoma in 1850 and reported it as being ‘specimens of molluscum contagiosum in the EAC [5]’.
Histopathologically, this is represented as a focal hyperplastic squamous epithelium of the EAC with accumulation of chronic inflammatory cells in the adjacent stromal tissue. Invasive growth of the EAC cholesteatoma into the deeper mesenchymal tissue results in accumulation of necrobiotic keratin debris in the newly formed central cavity. This is pathognomonic for the diagnosis of EAC cholesteatoma [6].
Naim et al. [6] defined a clinico-histopathologic classification of EAC cholesteatoma with a proposed surgical approach for each stage of the disease. The recommendations were: (i) A transcanal approach for Stage I disease—hyperplasia of the canal epithelium (ii) An endaural approach for Stage II—periostitis and Stage III disease—defective bony canal and finally (iii) A post-auricular incision followed by canal wall down technique for Stage IV disease—erosion of the adjacent anatomical structure.
Table 1 gives a summary of the reported cases of osteoma with cholesteatoma of the EAC. It demonstrates the experience of dealing with this rare association of osteoma and cholesteatoma of the EAC which when considered individually are of unknown aetiology. The disease sequelae are influenced mainly by the aggressiveness of the underlying cholesteatoma whose correct management depends on the surgical approach undertaken, enabling a favourable prognosis. The cases at presentation (Table 1) had either stage III or IV disease, despite being diagnosed in an era where improvements in sepsis control and clinical imaging have had significant impact on cholesteatoma disease outcome [2]. This is partly because of the insidious nature of EAC cholesteatoma concealing serious tissue destruction while remaining asymptomatic or presenting with relatively few symptoms [7].
| Reference (Please see List) . | Year . | Age . | Sex . | Intraoperative findings . | Classification and management as per Naim et al. 2005 . | Adopted surgical approach . | Canalplasty perfomed . | Outcome . |
|---|---|---|---|---|---|---|---|---|
| 1 (Article in Japanese) | 1986 | – | – | – | – | – | – | – |
| 1 | 1998 | 13 | F | Posterior canal wall erosion with serous otitis media | Stage III, Endaural approach with local anaesthesia | Transmeatal | No | Clinically disease free at 12 months |
| 1 | 2005 | 49 | M | Posterior canal wall erosion & involved middle ear cavity | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique(canal wall down mastoidectomy) | No | Clinically disease free at 6 months |
| 1 | 2006 | 12 | F | Posterior canal wall erosion, involved middle ear cavity & cerebellar abcess | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique (radical mastoidectomy) | No | – |
| Present case | 2011 | 24 | F | Inferior canal wall erosion with neck abscess | Stage IV, post-auricular incision followed by canal wall down technique | Transmeatal & post-auricular incision (cortical mastoidectomy) | Yes, temporalis fascia graft | Clinically disease free at 12 months |
| Reference (Please see List) . | Year . | Age . | Sex . | Intraoperative findings . | Classification and management as per Naim et al. 2005 . | Adopted surgical approach . | Canalplasty perfomed . | Outcome . |
|---|---|---|---|---|---|---|---|---|
| 1 (Article in Japanese) | 1986 | – | – | – | – | – | – | – |
| 1 | 1998 | 13 | F | Posterior canal wall erosion with serous otitis media | Stage III, Endaural approach with local anaesthesia | Transmeatal | No | Clinically disease free at 12 months |
| 1 | 2005 | 49 | M | Posterior canal wall erosion & involved middle ear cavity | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique(canal wall down mastoidectomy) | No | Clinically disease free at 6 months |
| 1 | 2006 | 12 | F | Posterior canal wall erosion, involved middle ear cavity & cerebellar abcess | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique (radical mastoidectomy) | No | – |
| Present case | 2011 | 24 | F | Inferior canal wall erosion with neck abscess | Stage IV, post-auricular incision followed by canal wall down technique | Transmeatal & post-auricular incision (cortical mastoidectomy) | Yes, temporalis fascia graft | Clinically disease free at 12 months |
| Reference (Please see List) . | Year . | Age . | Sex . | Intraoperative findings . | Classification and management as per Naim et al. 2005 . | Adopted surgical approach . | Canalplasty perfomed . | Outcome . |
|---|---|---|---|---|---|---|---|---|
| 1 (Article in Japanese) | 1986 | – | – | – | – | – | – | – |
| 1 | 1998 | 13 | F | Posterior canal wall erosion with serous otitis media | Stage III, Endaural approach with local anaesthesia | Transmeatal | No | Clinically disease free at 12 months |
| 1 | 2005 | 49 | M | Posterior canal wall erosion & involved middle ear cavity | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique(canal wall down mastoidectomy) | No | Clinically disease free at 6 months |
| 1 | 2006 | 12 | F | Posterior canal wall erosion, involved middle ear cavity & cerebellar abcess | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique (radical mastoidectomy) | No | – |
| Present case | 2011 | 24 | F | Inferior canal wall erosion with neck abscess | Stage IV, post-auricular incision followed by canal wall down technique | Transmeatal & post-auricular incision (cortical mastoidectomy) | Yes, temporalis fascia graft | Clinically disease free at 12 months |
| Reference (Please see List) . | Year . | Age . | Sex . | Intraoperative findings . | Classification and management as per Naim et al. 2005 . | Adopted surgical approach . | Canalplasty perfomed . | Outcome . |
|---|---|---|---|---|---|---|---|---|
| 1 (Article in Japanese) | 1986 | – | – | – | – | – | – | – |
| 1 | 1998 | 13 | F | Posterior canal wall erosion with serous otitis media | Stage III, Endaural approach with local anaesthesia | Transmeatal | No | Clinically disease free at 12 months |
| 1 | 2005 | 49 | M | Posterior canal wall erosion & involved middle ear cavity | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique(canal wall down mastoidectomy) | No | Clinically disease free at 6 months |
| 1 | 2006 | 12 | F | Posterior canal wall erosion, involved middle ear cavity & cerebellar abcess | Stage IV, post-auricular incision followed by canal wall down technique | Post-auricular incision followed by canal wall down technique (radical mastoidectomy) | No | – |
| Present case | 2011 | 24 | F | Inferior canal wall erosion with neck abscess | Stage IV, post-auricular incision followed by canal wall down technique | Transmeatal & post-auricular incision (cortical mastoidectomy) | Yes, temporalis fascia graft | Clinically disease free at 12 months |
EAC inflammation and sepsis [1] are additional complicating factors possibly explaining the extra-temporal extension of the disease in the latest two reports. Fig. 6 demonstrates the aural symptom duration in relation to the age of the osteoma at presentation in the individual cases described. The relatively short symptom duration and associated sequelae concords with the aggressiveness of cholesteatomas in the setting of EAC sepsis. Chronic inflammation has been shown to play a key role in the multiple etiopathogenic mechanisms of acquired cholesteatoma. Persistent chronic infection can enhance the aggressiveness of cholesteatomas, due to activation of osteoclasts and release of inflammatory mediators [2].
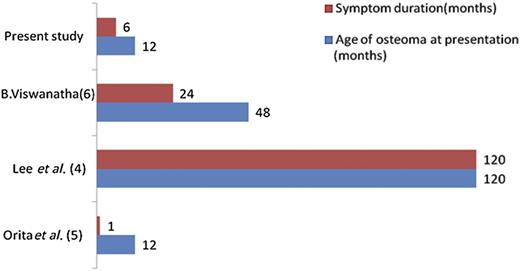
Variable temporal relation of osteoma with aural symptomatology. Note: EAC sepsis has been noted in all reported cases.
Although imaging and hearing thresholds are useful tools in assessing potential complications (performed in three out of four reported cases in Table 1), they are not essential for disease grading . In the absence of such adjunctive tests, we strongly recommend exploring the EAC and mastoid cavity if needed because of the previously reported complications [8] as well as eradication of intracranial or extracranial disease depending on the clinical presentation.
REFERENCES
Author notes
Paper has been presented at the South West Otolaryngology Association, Bristol, UK on the 24th of January 2013.



