-
PDF
- Split View
-
Views
-
Cite
Cite
Kaylie E. Hughes, James Arthur, An atypical case of large bowel obstruction, Journal of Surgical Case Reports, Volume 2013, Issue 6, June 2013, rjt042, https://doi.org/10.1093/jscr/rjt042
Close - Share Icon Share
Abstract
In Europe up to nine per cent of people suffer from renal calculi during their lifetime. Staghorn calculi are common and account for ∼11% of cases. Classic presentations include persistent loin pain, recurrent pyelonephritis or cystitis-like symptoms, renal colic or occasional haematuria. We present what we believe to be the first documented case of large bowel obstruction caused by a benign colonic stricture formed secondary to extravasation of a staghorn calculus.
INTRODUCTION
Staghorn calculi are relatively uncommon, accounting for 11% of nephrolithiasis cases. They evolve from simple calculi, which grow rapidly over months to form complex renal stones, filling the renal pelvis and branching outwards to occupy one or more renal calyces, characteristically resembling the horns of a stag [1]. Patients classically present with recurrent pyelonephritis, cystitis-like urinary symptoms, persistent flank pain, renal colic or haematuria. Perforated staghorn calculi have been known to present as subcutaneous abscesses or with leg emphysema mimicking gas gangrene, following secondary urinary infection with gas-forming bacteria [2, 3]. Below is a description of what is believed to be the first recorded case of a silent perforated staghorn calculus presenting as large bowel obstruction
CASE REPORT
A 63-year-old woman self-presented to the emergency department with a week's history of worsening abdominal pain, distension, faeculent vomiting and two days of absolute constipation. She denied any urinary symptoms or previous urinary tract infections. There were no red flag symptoms for colonic malignancy.
Examination revealed a soft distended abdomen, which was generally tender but more so in the left upper quadrant, with no palpable masses. Obstructive tinkling bowel sounds were heard on auscultation. Rectal examination and other system examinations were unremarkable.
Routine bloods were all within normal parameters, including white cells of 8.9, except for a marginally raised CRP of 28. Urinalysis on admission had a trace of protein and one plus of blood. Urine culture revealed no growth.
Abdominal X-ray confirmed large bowel obstruction with a cut-off point in the proximal descending colon. A large staghorn calculus was evident in the left kidney with a second smaller well-defined area of calcification just lateral to the renal parenchyma. (Fig. 1)

X-ray showing large left-sided stag horn calculus, with a second adjacent fragment outside the renal parenchyma with evidence of bowel obstruction.
Conservative management of bowel obstruction was initiated, a nasogastric tube was inserted and the patient was made nil by mouth while intravenous fluids were started.
A subsequent CT scan confirmed the presence of xanthogranulomatous pyelonephritis and established that the second area of calcification was a 1.5 × 1.0 × 2.5 cm perforated extra-renal fragment of calculus positioned adjacent to the proximal descending colon.
This stimulated a diffuse inflammatory response in the left upper quadrant, resulting in a prominent thick-walled proximal descending colon with an abrupt calibre change in the mid descending colon, mesenteric fat stranding, a thickened ileo-psoas muscle with fragments of calculi in the left iliac fossa, gross lymphadenopathy and inflammatory changes around the spleen. (Fig. 2)
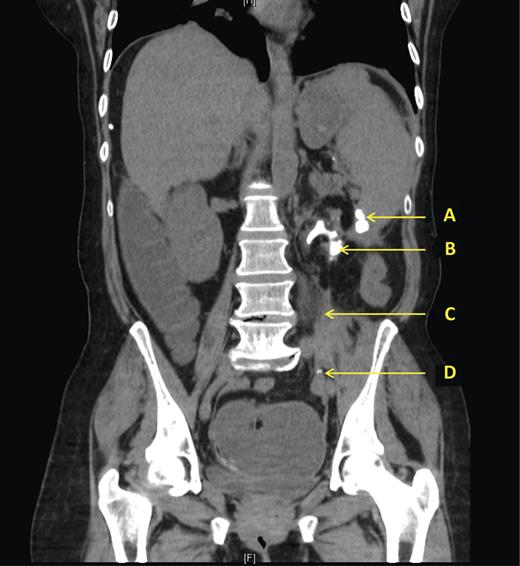
CT scan showing (A) Extra-renal fragment of calculus adjacent to transition point in thickened descending colon. (B) Staghorn calculus within atrophic left kidney with surrounding inflammation. (C) Thickened inflamed psoas muscle. (D) Fragments of calculus in LIF.
The patient's symptoms did not settle with conservative management, and as a result, she underwent an emergency left hemi-colectomy, left nephrectomy and extraction of the fragmented calculi. Recovery was uneventful. Histology confirmed an inflammatory stricture with hypertrophy and fibrosis but no malignancy. Stone analysis interestingly showed a struvite stone. Kidney histology revealed end-stage kidney disease with nephrosclerosis and chronic pyelonephritis. The parenchyma had been replaced with extensive fibro-fatty tissue and chronic inflammatory cell infiltrate with small areas of calcification. It contained thick-walled blood vessels and a few atrophic completely hyalinized renal glomeruli and various-size tubules with cast-like esosinophilic amorphous material. Many non-caseating granulomas were present in the hilar area with most containing a central calcification.
DISCUSSION
Staghorn calculi are more common in women with peak age at presentation being the fifth decade of life [1]. As with this case, most are unilateral at the time of diagnosis. They can be subcategorized into two groups based on composition; infective and metabolic stones.
Infective stones account for 80% of cases and formation correlates with urinary tract infection with urease-producing bacteria: Proteus, Staphylococcus and Klebsiella species [1]. Urease splits the urea in urine into ammonia and carbon dioxide. The elevated ammonia concentration causes a rise in the pH resulting in alkaline urine (pH ≥7.2). In the presence of magnesium and phosphate, this creates an ideal environment for inducing the crystallization of struvite (magnesium-ammonium-phosphate) and carbonate-apatite, encapsulating large numbers of bacteria within the stone's matrix during the process. Predisposing factors include vesico-ureteric reflux, indwelling catheters and anatomical abnormalities such as horseshoe kidney [1, 4].
Metabolic syndromes generate increased solute levels within urine, which when supersaturated precipitate giving rise to metabolic stones. Hypercalcaemia, hyperparathyroidism and hypercalciuria can create calcium oxalate calculi, the most prevalent stone, closely followed by uric acid stones (the product of hyperuricaemia). Rarer stones include calcium phosphate stones resulting from renal tubular acidosis, while cystinuria, an autosomal recessive condition, produces cysteine stones [4]. Dehydration stimulates calculi formation by concentrating urine [1].
Interestingly, this case highlights how a staghorn calculus can form in the absence of a metabolic syndrome or any prior noted history of urinary tract infections. The calculus in question had obviously been present for a long time because the kidney was completely atrophic with no parenchyma and was thus non-functioning. Throughout that time, the patient remained asymptomatic despite the fact that the calculus continued to enlarge at such a rate that extravasation of multiple calculi fragments occurred, resulting in irritation and inflammation to the surrounding structure. Yet, the patient sought help only when the consequential inflammation resulted in such severe colonic muscle hypertrophy that a benign stricture had been generated; completely occluding the bowel lumen causing large bowel obstruction.
Once diagnosed, staghorn calculi should be actively treated in order to prevent the development of life-threatening urosepsis or end-stage renal failure. The aim of treatment is to entirely eliminate the stone and preserve renal function [1, 4].
Due to the introduction of less invasive treatment modalities extracorporeal shockwave lithotripsy and percutaneous nephrolithotomy, open nephrectomy is now rarely used. It is only indicated for persistently symptomatic patients with atrophic kidneys contributing >10% towards the full renal function [5]. In this case, a nephrectomy seemed the obvious treatment option, preventing the development of future inflammatory strictures and eliminating urosepsis risk. Performing a synchronous left hemi-colectomy was required to treat the irreversible stricture, allowing resolution of her bowel obstruction.
Stag horn calculi account for 11% of renal calculi, yet this report presents what is believed to be the first documented case of large bowel obstruction presenting secondary to extravasation as a consequence of a previously undiagnosed stag horn calculus.



