-
PDF
- Split View
-
Views
-
Cite
Cite
KJ George, D Roy, A Shad, Haemorrhage into juxta-facet cysts causing bilateral foot drop, Journal of Surgical Case Reports, Volume 2012, Issue 9, September 2012, Page 7, https://doi.org/10.1093/jscr/2012.9.7
Close - Share Icon Share
Abstract
An 89 year old gentleman awaiting surgery for carcinoma of caecum presented with sudden back pain and developed foot drop two weeks later. MRI revealed multiple spinal metastases with a cyst in the canal at L4/5 causing spinal canal stenosis. Surgery revealed a juxta articular synovial cyst with haemorrhage in it. We discuss the presentation and management of juxtarticular cysts with a review of the literature.
INTRODUCTION
Foot drop is the dropping of the forefoot due to weakness and it is characterized by the inability to dorsiflex the ankle. The foot drop can be unilateral or bilateral. There are various aetiologies for foot drop; it can be caused by injury to the Peroneal Nerve, Neuromuscular disease, Trauma to the L5 nerve root (disc prolapse, direct trauma or iatrogenic), Degenerative diseases like poliomyelitis, spinal cord tumours, stroke, intracranial tumours and genetic, such as Charcot Marie Tooth disease and hereditary neuropathy. We present an unusual case which to our knowledge has never been reported before.
CASE REPORT
A 89 year old gentleman presented with sudden onset of low back pain which came on suddenly when he was standing. His mobility deteriorated gradually over the next two weeks until he developed bilateral complete foot drop. He had no sciatica of note and no disturbance of bowel or bladder function. He was awaiting a right hemi colectomy for carcinoma of the caecum. In the past he also had a nodular melanoma on his nose with node metastases 7 years ago. He had this excised with radical neck dissection and was free of recurrence. He also had past medical history of temporal arteritis, hypertension, left hip arthroplasty and left inguinal hernia repair.

On examination he had straight leg raise of 45 degrees bilaterally. He had normal tone in his legs. He had 1/5 power of bilateral ankle dorsiflexion and 3/5 power of dorsiflexion of big toe. All other muscle groups had 5/5 power. Both knee jerks were present and he had diminished bilateral ankle jerks. Rest of the neurological exam was unremarkable. Per rectal examination revealed normal anal tone and normal perianal sensation.
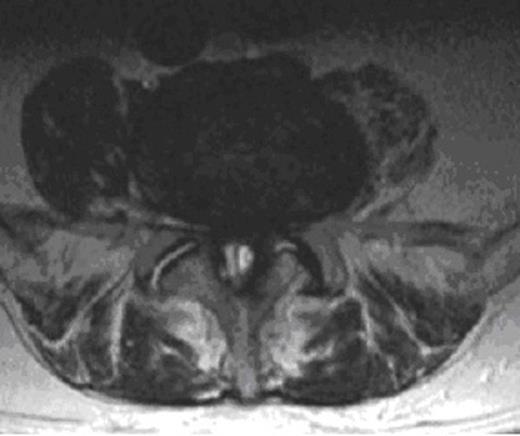
MRI of the whole spine revealed that he had multiple metastatic deposits throughout his spine with complete collapse of L3 vertebral body but intact disc space. Significant spinal canal stenosis at L4/5 level was seen due to a degenerative posterior disc bulge as well as a 2 x 1 x 1 cm size well capsulated, well defined lesion seeming to arise fromthe ligamentum flavum contributing to the canal narrowing.The appearances were thought to be either due to underlying haematoma from ligamentum flavum or a haemorrhagic synovial cyst. Significant cauda equina compression was noted.
He underwent emergency L4/5 lumbar laminectomy. A juxta articular synovial cyst containing straw coloured fluid was found compressing the theca and this was subsequently excised. Postoperatively he recovered well with improvement of ankle dorsiflexion to 4/5 power. Histology showed dense collagen bearing a small cyst lined by reactive synovium and containing some fibrin but no evidence of neoplasia is seen. Therefore a diagnosis of synovial cyst was made. He was subsequently referred to oncology for radiotherapy for his spinal metastases.
DISCUSSION
This gentleman awaiting treatment of bowel cancer presented with acute bilateral foot drop. Spinal metastasis causing vertebral body destruction and encroachment into canal was suspected. However this turned out to be from a completely different pathology in the form of a synovial cyst, even though he did have spinal metastases. An acute foot drop from a synovial cyst has not been reported before.
Synovial cysts are relatively uncommon in the spine but occur most frequently at the L4-5 level. The majority of these cysts are lined with synovial cells and contain a straw-coloured fluid. There have been several previous reports of symptomatic hemorrhagic synovial cysts in the lumbar spine. It is believed they result from either trauma or spinal instability. Most cases are associated with facet joint osteoarthritis and degenerative spondylolisthesis, but there is no correlation with age, gender, or degree of disc degeneration.
As in this case, most patients present with progressive low back and lower extremity radicular symptoms resulting from compression of the thecal sac or nerve roots. Patients may complain of focal tenderness over the facet joints with exacerbation of pain during extension. Other common findings not present in the current case, include motor and sensory deficits and positive straight leg raising test.
The recommended treatment of symptomatic synovial cysts is excision through laminectomy. In this case, a wide decompression was required to facilitate removal of the cyst. Other reported treatment options include computed tomography–guided fine needle aspiration and percutaneous injection of hyaluronidase (1).
Symptomatic lumbar facet cysts should be included in the differential diagnosis for patients presenting with progressive back pain and radicular symptoms. The symptoms are typically indistinguishable from disc herniation or spinal stenosis. Patients with significant facet degeneration and instability are predisposed to the development of facet cyst (2).
Haemorrhage into a lumbar synovial cyst causing an acute cauda equina syndrome has been reported (3). This was also treated with laminectomy and excision.
Normally synovial cysts cause a gradual onset of symptoms, however these two cases highlight that this can present acutely if haemorrhage occurs into it.



