-
PDF
- Split View
-
Views
-
Cite
Cite
AB Sosulski, JZ Fei, JP DeMuro, Partial cholecystectomy resulting in recurrent acute cholecystitis and choledocholithiasis, Journal of Surgical Case Reports, Volume 2012, Issue 9, September 2012, Page 17, https://doi.org/10.1093/jscr/2012.9.17
Close - Share Icon Share
Abstract
Partial cholecystectomy has been documented in the literature as a safe alternative in the management of patients with acute cholecystitis when the degree of inflammation prevents a safe dissection to identify the biliary structures for complete removal of the gallbladder. Partial cholecystectomy however is not without risk of recurrence, and the need for further surgical or endoscopic intervention in management of complications. We review a case in which partial cholecystectomy was performed without any relief of symptoms, to review the possible postoperative complications, and caution that these patients will need to be considered for a completion cholecystectomy.
INTRODUCTION
Partial cholecystectomy, whether open (1,2) or laparoscopic (3), has been described as a safe and effective operation. It is indicated in cases of severe acute cholecystitis, gangrenous cholecystitis or necrotizing cholecystitis, where the degree of inflammation precludes safe visualization of biliary structures. Partial cholecystectomy removes the majority of the gallbladder, leaving a portion of the neck, and occasionally the posterior wall of the gallbladder, in place. (4) It is reportedly tolerated well, with few minor postoperative complications, however the issues that do occur include recurrent symptoms, choledocholithiasis and persistent biliary fistula. (5) Historical accounts have documented partial cholecystectomy performed in the 1950s with washout and removal of gallbladder contents with placement of a drain in the orifice of the cystic duct when dissection of the hilar structures would be too dangerous, or the gallbladder was densely adherent to the liver bed. (6) It should be noted that even though technically possible, partial cholecystectomy is less than the ideal procedure, which is a complete cholecystectomy, with total removal of the gallbladder and closure of the cystic duct remnant.
Partial cholecystectomy may not provide a cure in all patients because leaving a portion of the gallbladder in situ in connection to the common bile duct may contribute not only to the formation of new stones, but also leaves a path intact for continued biliary colic and obstruction. We review a case in which partial cholecystectomy was performed due to severe inflammation in a young otherwise healthy patient.
CASE REPORT
A 22 year-old male presented with a history of several months of nausea, vomiting, right upper quadrant abdominal pain and in the last two weeks, jaundice. Seven months prior, he had undergone a partial cholecystectomy at an outside institution for severe acute cholecystitis. The case was attempted laparoscopically, however due to lack of visualization, it was converted to an open approach. The gallbladder was dissected from the fundus in a retrograde fashion, but extended far posteriorly, and was noted to be beyond surgical reach, secondary to the acute inflammation. A partial cholecystectomy was done with a surgical TA stapler across the infundibulum leaving approximately 25% of the gallbladder, including the entire cystic duct. The patient was discharged after a short postoperative stay.

MRCP shows the residual gallbladder (“X”), and the dilated common bile duct with stones (white arrows)
Over seven months, he had continued frequent recurrent attacks of acute cholecystitis, and choledocholithiasis. His symptoms included frequent nausea, vomiting, persistent sharp right upper quadrant pain, fever, and jaundice, which precipitated multiple Emergency Department visits to multiple institutions. The patient presented to our institution with an outside ultrasound that demonstrated multiple residual stones, a sonographic Murphy’s sign, and dilated common bile duct of 9 mm. Choledocholithiasis was confirmed by MRCP (Fig. 1) and gallstones were visualized in the remaining portion of the gallbladder by CT, (Fig. 2) although there was no evidence of gallbladder wall thickening or pericholecystic fluid. Preoperatively, an ERCP with sphincterotomy was performed to extract the remaining common bile duct stones (Fig. 3).
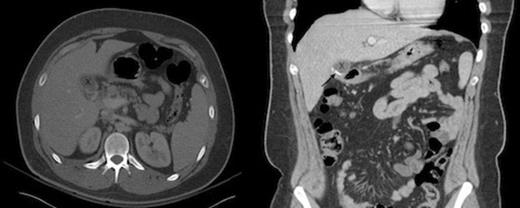
CT of the abdomen demonstrates the residual portion of the gallbladder, marked by an “X” in both the axial and coronal views. The staple line, indicated by a black arrow, is seen best on the coronal imaging
At operation, the previous transverse right upper quadrant incision was reentered, and dissection continued down to the liver. There were dense adhesions throughout the entire right upper quadrant. The previously stapled remnant of gallbladder was identified as partially intrahepatic, and located at the most inferior portion of the liver. Care was taken to dissect and mobilize the gallbladder from Calot’s triangle. The cystic duct and artery were then each ligated and a completion cholecystectomy was performed. Due to the still severe inflammation, the estimated blood loss was 1800 cc. On pathology, the specimen contained multiple gallstones, with acute cholecystitis. The patient tolerated the surgery well and was discharged home the following day, and made a full recovery with no further symptoms.
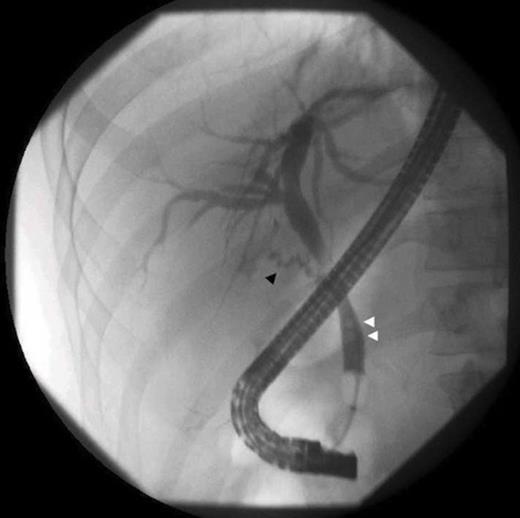
ERCP shows a residual cystic duct (black arrow), and choledocholithiasis (white arrows)
DISCUSSION
In patients with acute cholecystitis, partial cholecystectomy can be performed, when the severity of inflammation precludes safe dissection of the hilar structures. Depending on the extent of the resection and the structures left in situ, there is a definite risk of recurrence of symptoms, including recurrent acute cholecystitis (7), gallstone pancreatitis (8) and choledocholithiasis. The morbidity of recurrent gallbladder issues will require further endoscopic and/or surgical interventions in at least some patients, as the underlying pathophysiologic process responsible for the acute cholecystitis has not been definitively managed. All efforts should be made to remove remaining gallstones from the remaining portion of the gallbladder; as this was not done in our patient it explains the lack of recovery from the partial cholecystectomy.
Analogous to a cholecystostomy tube placement, partial cholecystectomy should therefore be considered another option for temporizing the patient experiencing severe acute cholecystitis. However, there needs to be an awareness that the patient will need to be considered for definitive surgical management with a completion cholecystectomy. In our case, this was done via an open approach due to the adhesions and the posterior position of the remnant gallbladder, but in more favorable cases it has been performed laparoscopically. (9)



