-
PDF
- Split View
-
Views
-
Cite
Cite
MW Morris, CD Anderson, LC Drake, SM Redfield, C Subramony, WB Vanderlan, Giant biliary cystadenoma, Journal of Surgical Case Reports, Volume 2012, Issue 9, September 2012, Page 15, https://doi.org/10.1093/jscr/2012.9.15
Close - Share Icon Share
Abstract
Biliary cystadenoma (BCA) is a rare cystic tumor which originates from intrahepatic or extrahepatic biliary ducts. Intrahepatic BCAs are more common, demonstrate a female predominance, and generally asymptomatic. Radiographic evaluation assists in the preoperative differentiation of these tumors from other cystic liver masses while resection remains the only means for definitive diagnosis. We report a case of massive mucinous intrahepatic BCA initially diagnosed as a nonresectable malignancy presenting in a female patient with progressively increasing abdominal pain and girth. Enucleation of the mass with non-anatomic resection was employed for surgical management of this intrahepatic BCA.
INTRODUCTION
Biliary cystadenoma (BCA) is a cystic benign tumor which originates from intrahepatic or extrahepatic biliary ducts. These rare tumors are most often encountered as an intrahepatic lesion in female patients. Clinical presentation depends on the site of the lesion. Intrahepatic lesions may present asymptomatically as an incidental finding or with abdominal pain and fullness. Extrahepatic BCA, by distinction, can present with obstructive jaundice and cholangitis. Definitive diagnosis prior to excision is complicated by the broad differential for cystic liver lesions. Computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound (US) in combination with clinical awareness improve noninvasive diagnosis. We present a case of symptomatic intrahepatic BCA initially diagnosed as a nonresectable malignancy requiring hospitalization due to failure of outpatient pain management and per os intolerance. Following resection the patient’s abdominal pain resolved.
CASE REPORT
A 27 year old female presented with three weeks of progressive and intractable abdominal pain with radiation to her right flank. The patient’s medical history was significant for obesity and symptomatic cholelithiasis. Laparoscopic cholecystectomy had been previously afforded for treatment of presumed biliary colic, but was unsuccessful in alleviation of pain. Depression was reported in response to a diagnosis of nonresectable intrahepatic malignancy following CT imaging at an outside institution. Physical exam was significant for abdominal tenderness and a palpable right upper quadrant mass extending into the left upper quadrant.
Laboratory evaluation was within normal limits except for mild hyperglycemia at 130 mg/dL, hyperbilirubinemia (total bilirubin = 1.7mg/dL, conjugated bilirubin = 1.02mg/dL), transaminitis (AST = 181 units/L, ALT = 423 units/L), and leukocytosis of 12,700 WBC/mm3. Carbohydrate antigen 19-9 and carcinoembryonic antigen were not measured. Dual phase CT imaging performed at our institution demonstrated a right hepatic multi-loculated cystic mass measuring 23 cm x 17 cm x 25 cm with internal septations and intrahepatic biliary dilation (Fig. 1).
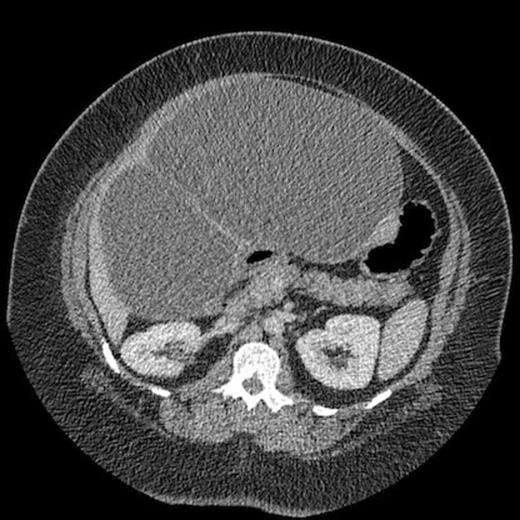
Computed tomography demonstrating large intrahepatic septated cystic lesion
The patient was admitted to the Acute Care Surgery service upon transfer from an outlying hospital. Discussion between the admitting team, radiology and the hepatobiliary transplant team, lead to a diagnosis of intrahepatic biliary cystic adenoma. Surgical resection was offered and the patient consented.
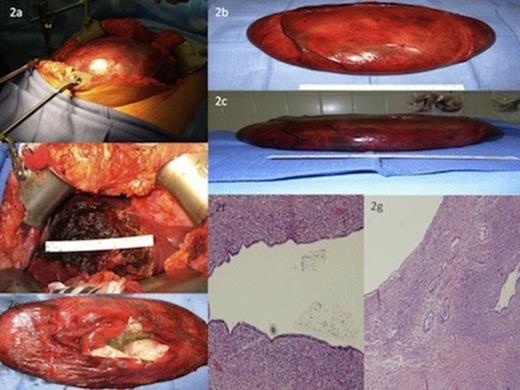
Gross appearance of Hepatic cystadenoma.Fig. 2b & 2c: Gross appearance of enucleated Hepatic Cystadenoma following Decompressive Cystotomy.Fig. 2d: Exposed Hepatic Parenchyma following Argon Beam Coagulation and Thrombin – Soaked Gelfoam Application.Fig. 2e: Gross Specimen demonstrating Ovarian Stroma Characteristics.Fig. 2f: Photomicrograph demonstrates normally arranged cuboidal epithelium and mucin overlying dense ovarian stroma.Fig. 2g: Photomicrograph demonstrates infiltrative atypical glands.
Due to the massive size of the lesion, decompression was judged necessary for resection (Fig. 2a). Cystotomy was performed and 2 liters of mucinous bilious fluid was evacuated, markedly decompressing the mass. Complete evacuation of all cystic fluid was considered unnecessary. A sample of cystic fluid was sent to pathology for cytologic evaluation. Closure of the cystotomy was performed with a 2–0 silk figure of eight suture. Enucleation of the mass was achieved with nonanatomic resection of segments 3, 4, and 5 (Fig. 2b,2c & 2d). Hemostasis of exposed hepatic parenchyma was achieved with argon beam cautery and thrombin soaked Gelfoam (Fig. 2d). Final pathology declared a mucinous biliary cystadenoma with dense ovarian-like stroma (Fig. 2e). Cytology was negative for malignancy.
Recovery was uncomplicated and the patient was progressed to ambulatory status and normal diet. She was discharged to home on postoperative day five. Symptomatic resolution was complete and without evidence of recurrence at six months post resection.
DISCUSSION
Intrahepatic biliary cystadenoma (IHBCA) is a rare clinical entity representing less than 5% of cystic liver disease cases (1). The true etiology of IHBCA remains idiopathic since first reported by Keen in 1892 (2). Abnormal embryonic development resulting in ectopic foregut or gonadal epithelium sequestered in the liver has been proposed (3,4). Presenting symptoms include abdominal pain, per os intolerance, abdominal distention, nausea, vomiting, and jaundice, yet patients may be asymptomatic at presentation (3-6). As in other reports, our patient presented with abdominal pain and decreased per os intake. To date no publication has established presenting symptoms that differentiate IHBCA versus other benign or malignant hepatic cystic diseases. Accurate diagnosis mandates clinical acumen combined with thorough preoperative evaluation.
Imaging results for IHBCA are nonspecific but characteristic. MRI, US and CT demonstrate intrahepatic cystic lesions with features such as mural nodules, varying wall thickness, papillary projections, and internal septations (5,7). Definitive diagnosis requires histologic examination following formal resection, liver transplant or enucleation (8). Resection or enucleation with clear margins is the treatment of choice for suspected IHBCA. Malignant degeneration and recurrence are 30% and 90%, respectively, for incompletely excised lesions (9). Cystotomy and internal drainage of IHBCA has been reported but carries risks of potential malignant degeneration of the residue, recurrence, and peritoneal seeding in the case of intrahepatic biliary cystadenocarcinoma (IHBCAC). The presence of mesenchymal stroma within an IHBCA increases the risk of malignant transformation and supports resection rather than conservative treatment (6,10). The presence of ovarian stroma within our patient’s IHBCA further justified resection due to increased malignant potential.
IHBCAC is distinguished histologically from IHBCA by the lack of epithelial architecture and nuclear stratification, basal membrane penetration, coarse capsular calcifications, septal proliferation, and cellular pleomorphism (1,10). Microscopic analysis demonstrated cysts lined with apical mucin and a single layer of cuboidal epithelium overlying a dense spindle cell ovarian-like stroma (Fig. 2f). A focus of infiltrative atypical glands with loss of mucin was identified within the cyst wall (Fig. 2g). However, there remained no nuclear pleomorphism, no basal membrane penetration, nor capsular calcifications.
IHBCA has specific demographic characteristics. Wang, et al., reported that the majority of IHBCA cases occurred in females aged 60 years or younger, which was consistent with our patient’s presentation (5). This same report contradistinctively noted that majority of IHBCAC cases occurred in male patients over the age of 60. Wang, et al., also determined that lesion size inversely correlated with the risk of malignancy. Adenomas presented with a mean maximum diameter of 13.03 ± 7.16 cm with the majority of cases over 8 cm in diameter, but carcinomas were smaller with a mean maximum diameter of 7.87 ± 4.46 cm and a majority measuring less than 8 cm in diameter. This inverse correlation of size to risk of malignancy seems counterintuitive and represented a decreased risk of malignancy in our patient.
IHBCA and IHBCAC are rare lesions lacking pathognomonic clinical findings with somewhat counterintuitive malignant potential. The rarity and counterintuitive nature of these lesions emphasizes the importance of involving hepatobiliary specialists. Resection remains the mainstay of treatment.



