-
PDF
- Split View
-
Views
-
Cite
Cite
J Richardson, M Richardson, R Nijjar, Fistula after pyloroplasty – A novel approach to the management of a leak following oesophagectomy, Journal of Surgical Case Reports, Volume 2012, Issue 2, February 2012, Page 9, https://doi.org/10.1093/jscr/2012.2.9
Close - Share Icon Share
Abstract
Management of upper gastrointestinal anastomotic leaks is an inter-disciplinary challenge. We present a case of late pyloroplasty leak following 3-stage oesophagectomy. We describe a novel, combined endoscopic and fluroscopic procedure to introduce a T-tube into the anastomotic leak proving an ideal plug at the site of leak which enabled the patient to consume a normal diet and return home safely.
INTRODUCTION
Data synthesized from existing randomised controlled trials show that pyloric drainage procedures reduce the occurrence of early post-operative gastric outlet obstruction after oesophagectomy with gastric reconstruction (1,2). Pyloromyotomy and pyloroplasty are generally considered simple procedures, however, they may be complicated by stricture, leak, and even death (3). Because of these complications some advocate not performing an emptying procedure during oesophagectomy (3). We report a novel approach to the management of pyloroplasty leak following 3-stage oesophagectomy.
CASE REPORT
A 61-year-old gentleman presented in January 2010 with dysphagia for solids and regurgitation.
An urgent endoscopy was performed. It revealed a mid to distal oesophageal cancer (25-32cm). This arose from a long segment of multifocal dysplastic Barrett’s metaplasia (22-39cm). Full pre-operative staging investigations diagnosed a poorly differentiated mid to distal oesophageal adenocarcinoma (T3, N1, M0).
The patient was recruited to the OEO5 trial in April 2010 and underwent neo-adjuvant chemotherapy with 5-fluorouracil and cisplatin. In May 2010 he underwent 3-stage McKeown oesophagectomy with a formal Heineke-Mikulicz pyloroplasty (2-layer, interrupted closure with omental patch). A covering tube drain and feeding jejunostomy were placed.
Final histology of the resected specimen revealed T3, N1 (2/22), M0, poorly differentiated adenocarcinoma with microscopically involved margins (circumferential) with vascular and lymphatic invasion.
On post-operative day 7 a routine post-operative contrast swallow was performed. This identified a spill of contrast due to a 5mm anterior defect at the level of the oesophago-gastric anastomosis suggestive of focal ischaemia. This was managed with washout and drainage and a covered oesophageal stent. A further contrast swallow revealed contrast aggregating around the drain (Figure 1) and that the covered oesophageal stent was appropriately positioned with no evidence of on-going leak (Figure 2).
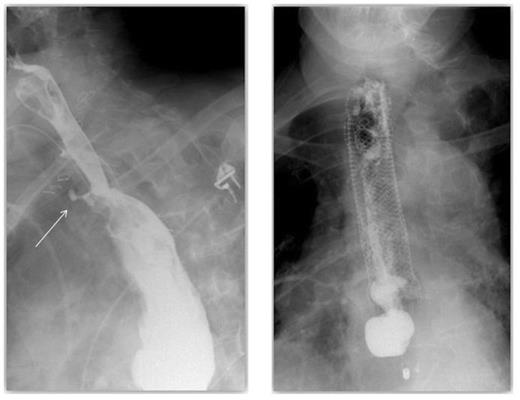
A contrast swallow demonstrating contrast aggregating around the drain & A covered oesophageal stent appropriately positioned with no evidence of leak
On post-operative day 11, at routine dressing change on the ward, a full thickness abdominal wall dehiscence was identified. The patient proceeded to laparotomy where turbid intra-peritoneal fluid was identified. There was no evidence of intra-peritoneal bile. The patient was managed with washout, drainage and re-suturing of the abdominal wall over a vicryl mesh. The original intra-abdominal tube drain was left undisturbed.
On post-operative day 16 a late pyloroplasty leak was diagnosed on contrast swallow (Figure 3). This presented as a persistent leak of bile stained discharge from the abdominal drain. After failure of initial conservative treatment an attempt to control the leak was made.
The defect at the pyloroplasty suture line was now visible endoscopically and a covered pyloric stent was located appropriately across the defect. Due to proximal stent migration this was unsuccessful in controlling the leak (Figure 4). The patient still had a controlled fistula from the pyloroplasty suture line.

A late pyloroplasty leak diagnosed on contrast swallow & A contrast swallow demonstrating proximal stent migration and evidence of on-going leak
The patient was now stable and he requested to eat and drink. A surgical approach to the management of fistula after pyloroplasty was deemed inappropriate because of the recent surgery for intra-abdominal sepsis and the presence of an abdominal wall mesh.
A novel approach to the management of a fistula after pyloroplasty was employed. A combined endoscopic and fluoroscopic procedure was performed where a radiologically placed snare was inserted through the abdominal drain and manipulated into the gastric tube through the defect in the pyloroplasty. A gastroscope was used to introduce a T-tube into the gastric tube and into the snare. The abdominal drain and snare were withdrawn and the T-tube placed appropriately, plugging the hole in the pyloroplasty, under direct vision. A further guide wire was left in place along the tract of the tube drain and was used to deploy a pigtail drain alongside the pyloroplasty (Figures 5 and 6).
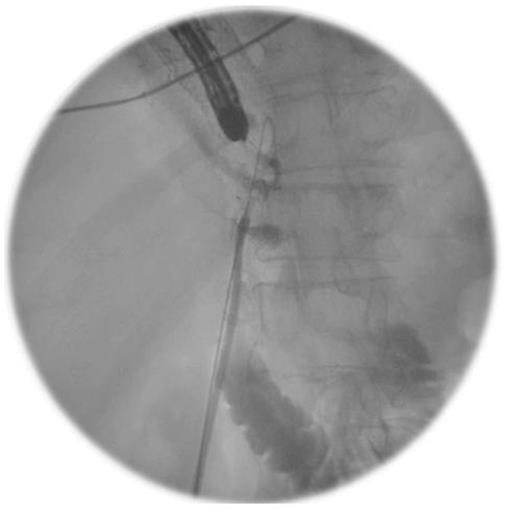
An Intra-operative image demonstrating the combined endoscopic and fluoroscopic procedure
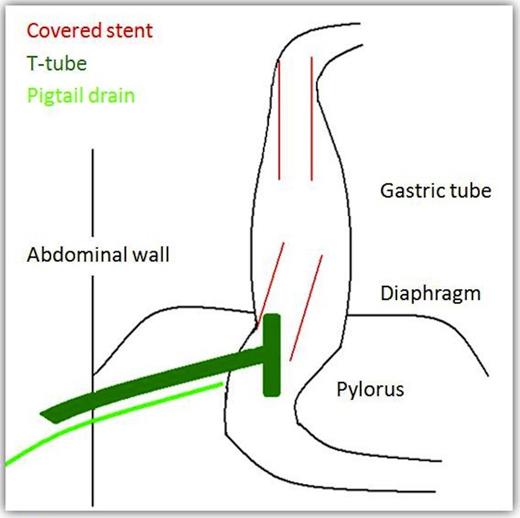
Follow up CT, with contrast both orally and through the T-tube, showed no evidence of ongoing leak from the pyloroplasty. The flanged T–tube satisfactorily plugged the hole through the anterior wall of the pyloroplasty, best demonstrated in the lateral decubitus position (Figures 7 and 8).
The T-tube was then capped off and the pigtail drain subsequently removed. The patient was commenced on oral fluids and progressed to oral diet. The patient was discharged with a capped off T-tube in situ and made a good recovery.
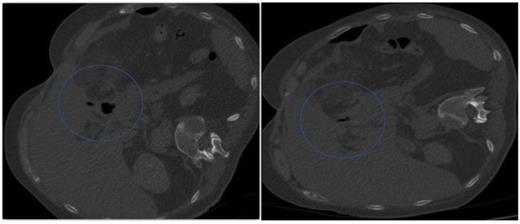
A follow-up CT demonstrating no evidence of on-going leak from the pyloroplasty & A follow-up CT demonstrating the flanged T-tube satisfactorily plugging the hole through the anterior wall of the pyloroplasty
DISCUSSION
Management of anastomotic leaks is an inter-disciplinary challenge (1). Anastomotic leaks are serious complications after upper gastrointestinal surgery. Treatment of leaks by direct suture repair, revision, patching, and application of fibrin glue to leaks have failed to gain widespread acceptance owing to a high failure rate (4). Alternative methods of controlling leaks such as the placement of covered stents are feasible but can be complicated by stent migration (4) and inadequate drainage of associated collections.
To our knowledge this is the only reported case of management of late pyloroplasty leak following oesophagectomy with a combined endoscopic and radiological placement of a T-tube. The T-tube provided an ideal plug at the site of leak which enabled the patient to consume a normal diet and return home safely.



