-
PDF
- Split View
-
Views
-
Cite
Cite
AS Sur, M Peters, HS Sur, S Adjepong, Benign gastric ulceration as a cause of gastro-colic fistula, Journal of Surgical Case Reports, Volume 2012, Issue 2, February 2012, Page 7, https://doi.org/10.1093/jscr/2012.2.7
Close - Share Icon Share
Abstract
Gastro-colic fistulas as a complication of benign gastric ulcers are relatively uncommon. The authors report a 59 year old caucasian female with a known hiatus hernia and gastro-oesophageal reflux disease presenting with diarrhoea and weight loss. Barium enema is the investigation of choice although it is important to exclude malignancy. Management is by en-bloc resection of the fistula with primary gastro-intestinal reconstruction.
INTRODUCTION
Gastro-colic fistula is a rare cause of vomiting, diarrhoea and weight loss and one that must be considered if the more common differential diagnoses such as gastroenteritis are excluded. There are numerous causes of gastro-colic fistulas but those caused by benign gastric ulceration are a rarity. The investigation of choice is a barium enema. Other investigations to exclude malignancy must be carried out. The optimal intervention is surgical with en-bloc resection of the fistula with primary gastro-intestinal reconstruction.
CASE PRESENTATION
A 59 year old female presented to the Emergency Department with a two week history of diarrhoea and weight loss. The diarrhoea occurred more after meals and the patient had lost 2-3 stone over the last 2 weeks.
She was known to have a hiatus hernia and a gastric ulcer that was diagnosed a month previously and was being actively treated for pyloric stenosis by oesophagogastroduodenoscopy and dilatation.
On examination she was apyrexial and looked cachectic. Systemic examination was non-specific and did not reveal and pathological findings.
Laboratory findings revealed marked dehydration but erect chest x-ray and abdominal x-ray was unremarkable. Stool culture failed to reveal any infective cause of this diarrhoea.
The patient underwent further investigation commencing with an oeasophagogastroduodenoscopy which demonstrated the hiatus hernia, gastritis and a gastric ulcer as well as pyloric scarring and deformity. A biopsy sample was taken showing features consistent with non-specific active chronic gastritis. No cause for the patient’s symptoms was established.
She then had a barium meal and follow through which clearly demonstrated a gastro-colic fistula. This was confirmed by colonoscopy which demonstrated the fistula. There were no signs of neoplasia and the no malignancy was witnessed on biopsy. These findings were confirmed on CT.
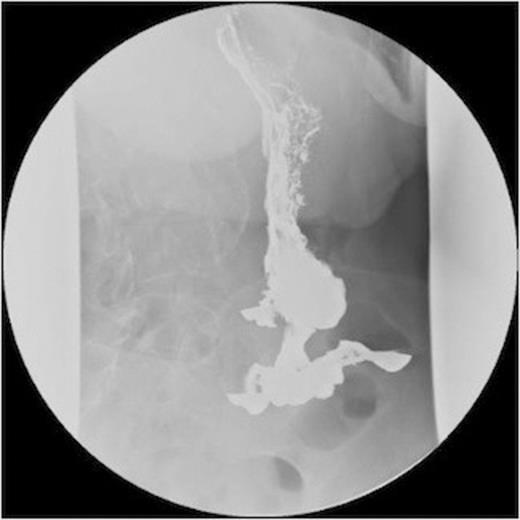
A series of radiographs from barium swallow demonstrating gastro-colic fistula

A series of radiographs from barium swallow demonstrating gastro-colic fistula
The patient underwent a laparotomy and resection of the gastro-colic fistula. The transverse colon was mobilised and a segment of the colon resected with the fistula. Partial gastrectomy was carried out en-bloc with the fistula. A Bilroth I gastro-duodenal anastamosis was undertaken with two layers of PDS. Colo-colic anastamosis was performed in a single layer of PDS. A feeding jejunostomy and a drain in the sub-hepatic space were placed before closure of the abdomen.

A series of radiographs from barium swallow demonstrating gastro-colic fistula

A series of radiographs from barium swallow demonstrating gastro-colic fistula
DISCUSSION
Gastro-colic fistulas are a direct communication between the stomach and the colon and are a relatively rare condition. More common causes are invasive carcinomas of the stomach or colon, post-operatively, secondary to Crohns disease, diverticular disease and intra-abdominal abscesses and due to infections such as tuberculosis or syphyllis (1). Gastro-colic fistula secondary to benign gastric ulcer disease is uncommon with only 111 reported cases in English literature (2). Most patients with benign gastro-colic fistula were middle-age women with a history of recent anti-inflammatory drug therapy (3).
The literature reports patients with gastro-colic fistula presenting with a syndrome of severe diarrhoea, weight loss, anaemia and feculent vomiting. This is a result of colonic contents regurgitating into the stomach and entering the small bowel, leading to a derangement of digestive and absorptive functions of the small bowel (4). Patients may give a history of peptic ulcer disease. Majority of patients will be malnourished and dehydrated at time of presentation. Occult or frank gastrointestinal bleeding occurs in 25% to 33% of those with benign disease (3).
The patient will often have derangement of their electrolytes. Biochemical test will be suggestive of vitamin deficiencies and decrease serum protein. Haematologically, there may be anaemia and a slight leucocytosis. If a nasogastric tube to passed, aspiration of feculent material may hint towards the diagnosis (1).
Barium studies are the investigation of choice in diagnosing gastro-colic fistula (1). Thoeny, Hodgson and Scudamore, in the 1960, reported a 95% success rate with barium enema. There have been reports of computer tomography to delineate the fistula and identify underlying pathology (5,6). Gastroscopy and colonoscopy are less sensitive in establishing diagnosis but are important in obtaining multiple biopsies to excluding malignant disease (7).
As majority of these patients are malnourished at the time of presentation, nutritional support via IV hyperalimentation is an important adjunct (1). There have been reports in the literature of effective treatment gastro-colic fistula secondary to benign gastric ulcer with antacid medication. In these cases, healing time varied between 2 to 16 weeks with an average of 9 weeks (3).
Surgical intervention is traditionally the treatment of choice by en bloc resection and primary reconstruction (1).



