-
PDF
- Split View
-
Views
-
Cite
Cite
Robert Döring, Bernhard Ciritsis, Thomas Giesen, Hans-Peter Simmen, Pietro Giovanoli, Direct nerve suture and knee immobilization in 90° flexion as a technique for treatment of common peroneal, tibial and sural nerve injuries in complex knee trauma, Journal of Surgical Case Reports, Volume 2012, Issue 12, December 2012, rjs019, https://doi.org/10.1093/jscr/rjs019
Close - Share Icon Share
Abstract
There are different ways to treat peripheral nerve injuries with concomitant defects in the lower extremity. One option is a direct nerve suture followed by immobilization of the knee in flexion as it is described for gunshot wounds that lead to lesions of the sciatic nerve and its terminal branches as well as isolated nerve lesions. We used this technique to treat a case of multiple nerve injuries of the lower extremity combined with a complex knee trauma including a lesion of both bones and the posterior capsule. To our knowledge, this technique has not yet been described for such a combined injury in literature.
INTRODUCTION
In trauma surgery, accidents involving vehicles are among the most common injuries presented to surgeons. Among vehicle accidents, motorcycle accidents take a special position due to the unique nature of the vehicle and high velocities combined with little to no protection to the driver.
It has been suggested that motorcycle accidents are a significant risk factor to both traumas of the lower extremity [1] and peripheral nerve lesions [2]. Regarding tibial and peroneal nerve injuries, they are most frequently combined with knee injuries with and without fractures and lacerations [3, 4].
When a peripheral nerve is traumatically separated, the common approach is to reconnect the separated nerve endings by a suture, adapting the functional nerve endings end-to-end. If a substantial defect to the nerve and a gap occurs, more complex solutions have to be applied. Commonly, an autologous graft is interposed as a makeshift nerve, usually the sural nerve. However, the outcomes are poorer than that of a direct suture, be it a primary (up to 7 days after trauma) or secondary suture (thereafter) [5].
In the following case, the authors have applied a recent method that has been published by Oberlin and Rantissi for isolated gunshot injuries to nerves of the lower extremity [6].
CASE PRESENTATION
A 18-year-old patient lost control while driving a motorcycle in Bosnia and crashed into the guardrail. He was first treated at a local hospital, where examinations showed a IIIC° (Gustilo and Anderson) open knee fracture with lesions of both the popliteal artery and vein as well as damage to the peroneal and popliteal nerves. Arterial and venous reconstruction by means of an end-to-end anastomosis of the popliteal vessels was carried out and, due to a suspected compartment syndrome, the patient underwent a fasciotomy the next day. The patient was transferred to the trauma division of the University Hospital of Zurich, Switzerland, 4 days thereafter.
Upon clinical presentation, the patient reported that he had no sensitivity in his lateral foot in the affected leg; plantar sensitivity was present yet very weak. Plantar flexion and dorsal extension were not possible and the lateral flexors of the foot had been affected by a paresis as well. The left foot was warm with a good ultrasound signal for the Arteria tibialis posterior pulse but no signal for the Arteria dorsalis pedis.
Examinations revealed multiple soft-tissue lesions, including an avulsion of the lateral femoral condyle, ruptures of the joint capsule as well as of the biceps femoris, gastrocnemic and plantaris muscles. In addition, the common fibular and sural nerve had been entirely separated and the tibial nerve as well as the popliteal vein and artery had been severely damaged. A direct suture of the nerve endings with a regularly extended knee was not conceivable; yet it was noted that if the knee was in 90° flexion, the nerve endings could be approximated enough so that a direct suture was possible (Figs 1–2). Hence, the wound was thoroughly cleaned and debrided, and an external fixator bridging the knee joint was installed. A direct suture of the nerves was performed by the plastic surgeons using Ethibond 9-0 and fibrin glue. Hereafter, the ruptured muscles and the joint capsule were sutured by the trauma surgeons. The patient developed well, so that the external fixation device could be removed 6 weeks postoperatively without any complications.
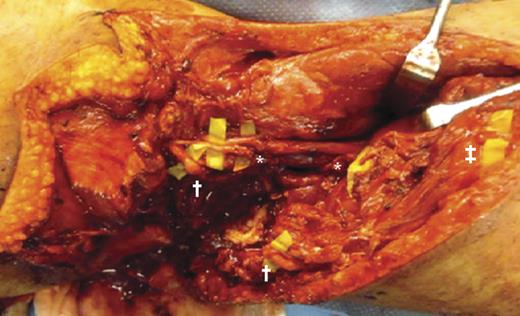
Intraoperative photography reveals gaps of tibial (*), common peroneal (†) and sural (‡) nerves associated with lesions of the gastrocnemic muscles.

Intraoperative photography after fixation of the knee in 90° flexion and sutures of tibial (*) and common peroneal (†) nerve. Junction of the sural (‡) nerve has not yet been performed.
Half a year after the patient’s discharge from the hospital, the wounds had healed and his motoric skills had improved greatly, even though the healing of the peroneal nerve and its associated muscles was impaired. He was able to flex his knee joint to entirely (M5), flex the ankle joint 10° (M3) and bend his toes partially (M3). However, the extension and inversion/eversion of his foot as well as extensions of the toes were not possible. Still, he was able to walk without crutches and stand on the left leg without aid (Figs 3 and 4). Furthermore, the patient reported that the deficits in sensitivity were consequently diminishing with residual anesthesia of the very distal shank and foot. An electroneuromyography of the common fibular nerve and the tibial nerve was performed 6 months postoperatively. Hereby it was found that the long peroneal muscle had been re-innervated by the superficial branch of the fibular nerve, whilst there was not only axonal but also severe myogenous damage (electrically silent muscles) to all the muscles innervated by the profound branch of the fibular nerve. We concluded that this was due to the compartment syndrome. Concerning the tibial nerve, a re-innervation of the medial head of the gastrocnemic muscle was seen.

Clinical examination 6 months after trauma showed well-healed wounds and the possibility to stand on the left leg without aid.
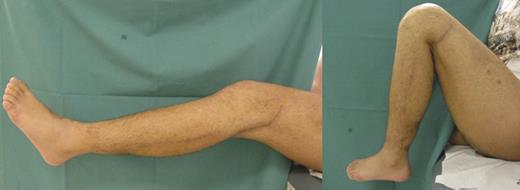
Good range of motion (flexion/extension 140-10-0°) 6 months after trauma.
To the current date, we are very satisfied with the results the patient has achieved; he reportedly planned to re-enter work life soon after his last visit.
DISCUSSION
Treatment options for peripheral nerve injuries include direct nerve repair, nerve grafting and nerve transfer. Actual recommendations prefer a direct nerve suture due to better results, if possible [5, 7]. It is well known that nerve sutures with tension provide fibrous reaction and poor results [8, 9]. The problem surgeons’ face when adapting nerves in traumatized patients with more complex injuries is the fact that most commonly there is a loss of matter and therefore a gap between the functional nerve endings and hence a tension-free suture cannot be achieved.
In case, the gap happens to be close to a joint, a flexion in this joint can lead to both nerve endings approaching each other, anatomically making a primary suture without tension possible. In order to protect the freshly sutured nerve from traction, it is necessary to arrest the affected joint. In 1966, this technique was used for the first time by Bourrel et al. for a secondary suture 15 months after section of the sciatic nerve [10] with remarkable results. In their 2011 paper, Oberlin and Rantissi reported 12 cases with isolated nerve lesions in which they performed primary sutures in combination with joint fixation and immobilization for 6 weeks, leading to very good results.
In the case under consideration, we found a similar initial situation regarding nerve lesions, as shown in the aforementioned publications, but with additional injuries to both bone and posterior joint capsule. We chose not to bridge the defect with a graft but rather to resort to the method suggested by Oberlin and Rantissi. Overall, the healing process of the patient was equally pleasing and a nearly normal range of motion in the knee joint could be reached. Even though a restitution ad integrum is highly unlikely in this case, our patient is able to participate in daily life, handle day-to-day business and re-enter his occupation with an overall good quality of life.
Conflict of interest
None declared.



