-
PDF
- Split View
-
Views
-
Cite
Cite
Sarah F. Powell-Brett, James T. Royle, Timothy Stone, Rob G. Clarke, Caecum herniation through the Foramen of Winslow, Journal of Surgical Case Reports, Volume 2012, Issue 12, December 2012, rjs016, https://doi.org/10.1093/jscr/rjs016
Close - Share Icon Share
Abstract
Foramen of Winslow herniation is a rare occurrence with a high mortality; it presents a diagnostic challenge with subtle clinical and radiological features. We present a case of caecal herniation through the foramen of Winslow creating a closed loop obstruction which remained undiagnosed until laparotomy. Reduction was achieved with gentle traction after first decompressing the caecum whilst still within the lesser sac.
INTRODUCTION
Bowel obstruction secondary to herniation through the foramen of Winslow is an exceptionally rare condition that confers significant risk. It accounts for only 0.08% of all herniae [1]. There are fewer than 150 cases recorded to date, less than a third of these involving the caecum [2]. It carries a mortality of 36–49%, mainly through diagnostic delay [3].
Herein we describe a case of a woman with caecal herniation through the Foramen of Winslow causing subacute bowel obstruction. Emphasized in this report are the clinical and radiological indicators which may have expedited diagnosis and which may help with early identification of this condition. We also describe our operative management of this case.
CASE REPORT
A 41-year-old woman presented with a 2-day history of severe, central, cramping abdominal pain of gradual onset, which progressively radiated to the right side of her abdomen. It was relieved by lying on her right side, assuming the foetal position or by bending forwards on the floor. Conversely straightening or stretching her abdomen exacerbated the pain. The patient had not opened her bowels (although she was still passing small amounts of flatus) in 3 days and had been vomiting for 48 h.
Her laboratory results showed leukocytosis of 14.4 × 109, her other results were unremarkable.
Plain abdominal radiography (Fig. 1) displayed a dilated viscus in the left upper quadrant with absence of colonic shadow on the right side of the abdomen. Initially this was reported as a large distended stomach, but in retrospect was thought to be the caecum.

Abdominal X-ray showing dilated viscus in the right upper quadrant, initially reported as large distended stomach, in retrospect thought to be the caecum.
An ultrasound scan of her gall bladder was performed to rule out the possibility of acute cholecystitis; this showed a small amount of free fluid and a known ovarian dermoid cyst.
Computed tomography was used for diagnosis. Although initially reported as caecal volvulus, in hindsight there were features indicative of the herniation. (Figs 2 and 3).
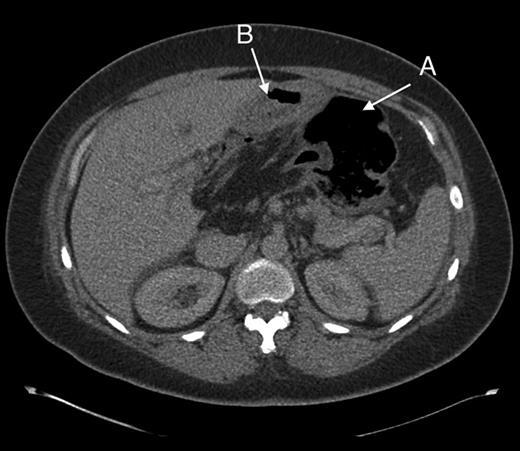
Axial section through upper abdomen showing (A) distended caecum and (B) behind the stomach.
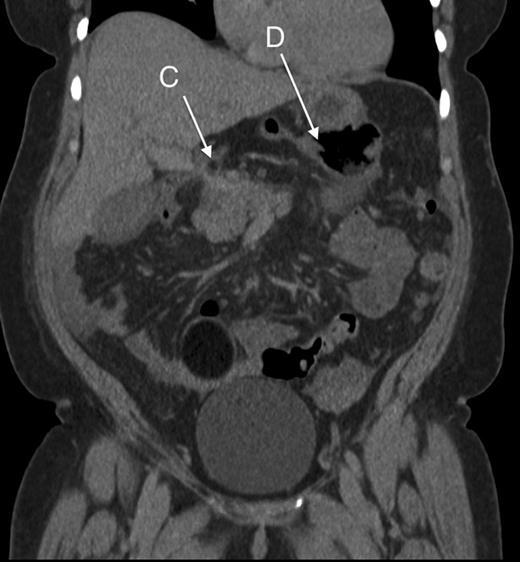
Coronal section showing part of the colon passing behind the portal vessels (C) and a distended caecum in the lesser sac (D).
On the basis of the computed tomography findings, the patient was taken to theatre for her presumed caecal volvulus. At laparotomy however, the caecum was noted to be herniating through the foramen of Winslow causing closed loop obstruction. It could not be reduced by gentle traction, so the lesser sac was opened up and the caecum decompressed with a small enterotomy and suction to allow reduction. A right hemicolectomy with stapled side-to-side anastomosis was then performed to remove the compromised bowel and the foramen was left open. The patient had an uneventful postoperative recovery and was discharged 4 days later (Figs 4 and 5).
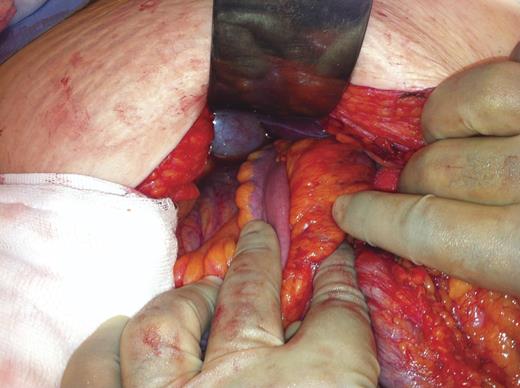
Terminal illeum disappearing behind the portal vessels, inferior to the gallbladder and into the lesser sac.
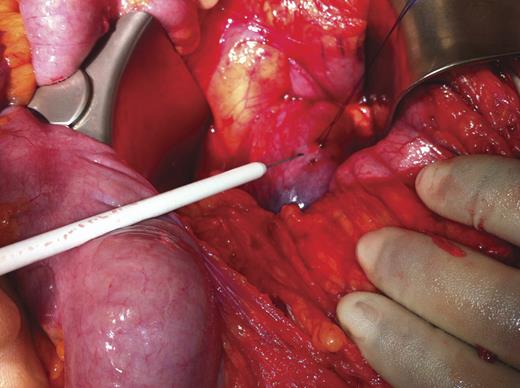
Having opened up the lesser sac, the distended herniated portion of caecum can be seen about to needle decompressed under cover of a purse string suture.
DISCUSSION
Foramen of Winslow herniation is a rare occurrence: it is difficult to diagnose both clinically and radiologically. Often the non-specific clinical signs and symptoms are misinterpreted and surgery is inadvertently delayed leading to bowel strangulation, which may explain the high mortality (around 49%) associated with this condition. The reasons for this herniation remain unclear, although several predisposing factors have been postulated by Moynihan: (a) a long or excessively mobile mesentery, (b) excessively large Foramen of Winslow, (c) absence of fusion of ascending colon to posterior abdominal wall [4].
Interestingly, specific descriptive features of her pain could have been indicative of her underlying diagnosis: she described a pain that was significantly improved with complete truncal flexion (knees right up to her chest was the only position affording any relief): this posture opens up the Foramen. This has been alluded to in several other case reports [5] and may be key to achieving an early diagnosis or at least increasing the index of suspicion and therefore encourage early escalation of investigation.
In retrospect there are several radiological features that could have clinched the diagnosis (see Figs 1–5), which have previously been described in the literature [6]. These include: (a) an absence of colon in the right gutter, (b) presence of mesentery between the portal vein and the inferior vena cava, (c) the presence of gas or fluid in the lesser sac, (d) the presence of terminal ileum and ascending colon displaced superiorly in the sub-hepatic space.
Operative management involves reduction through the defect, and most reports describe reduction being achieved via gentle traction or by opening up the lesser sac to help deliver it. However, because of the extent of distension in this case, this was not possible and decompression was required before the segment could be reduced. This is not a commonly used technique. There is debate as to the appropriate management to prevent recurrence, including right hemicolectomy, Foramen closure or caecal fixation. There is very little evidence for recurrent herniation and there is postulation that closure of the foramen poses risk to portal vessels and surrounding structures. Thus leaving the foramen open may be justifiable, especially in this case where a right hemicolectomy was performed.
To summarize, this was an interesting case of a rare condition that carries a high mortality resultant from mis-diagnosis and treatment delay. It is an entity that needs to be publicized further to heighten awareness of potential diagnostic indicators both clinically and radiologically. Of particular interest in this case is the unique pain relief found from extreme truncal flexion, which when elicited in a good clinical history should direct the clinician towards urgent escalation of investigation and treatment, and thus reduce mortality.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.



