-
PDF
- Split View
-
Views
-
Cite
Cite
L Henderson, A Johnston, B Mockford, B Craig, Posterior hip dislocation and ipsilateral isolated femoral neck fracture: A novel fixation method, Journal of Surgical Case Reports, Volume 2012, Issue 10, October 2012, Page 14, https://doi.org/10.1093/jscr/2012.10.14
Close - Share Icon Share
Abstract
It is accepted that a traumatic hip dislocation is a surgical emergency, this holds for the uncommon dislocation of the hip with femoral neck fracture however the surgical dilemma involves head salvage or replacement.
This case report describes the method and technique for stabilisation of the rare and challenging isolated posterior hip dislocation with an ipsilateral femoral neck fracture.
A 38-year-old gentleman was involved in a high-speed road traffic collision sustaining a posterior dislocation with ipsilateral femoral neck fracture. This was managed emergently with open reduction and osteosynthesis. The technique was by the modified placement of three cannulated screws through a posterior approach. The use of antegrade guide wires allowed accurate placement in a triangular configuration and temporary fixation to facilitate hip reduction prior to retrograde insertion of three 6.5mm cannulated screws.
The patient, although developing radiological avascular necrosis, continues to work and has returned to hobbies at 4.5 years.
INTRODUCTION
Traumatic hip dislocation with associated femoral neck fracture in the absence of an acetabular fracture is a rare and challenging injury. These are typically high-energy injuries in young patients and may result in significant morbidity and loss of future function resulting from avascular necrosis and secondary osteoarthrosis (6,7).
The decision for surgical treatment of these injuries will involve either surgical fixation or prosthetic replacement and with the limited number of cases described there remains little in the literature to support a definitive treatment option (2,3,5,8).
This case reports a posterior hip dislocation with isolated ipsilateral femoral neck fracture treated by a modified technique of a standard 3-parallel screw fixation method with long-term follow-up.
CASE REPORT
A 38-year-old male motorcyclist was involved in a high-speed collision. He was transferred to the local district general hospital where examination revealed an abducted, shortened and externally rotated left lower extremity with no evidence of neurovascular injury.

Posterior dislocation of the femoral head with no associated acetabular fracture
Antero-posterior radiograph of the pelvis confirmed a displaced transcervical femoral neck fracture with associated dislocation of the femoral head. Computed-tomography, confirmed a posterior dislocation of the femoral head with no associated acetabular fracture (Fig. 1,2,3).

Posterior dislocation of the femoral head with no associated acetabular fracture
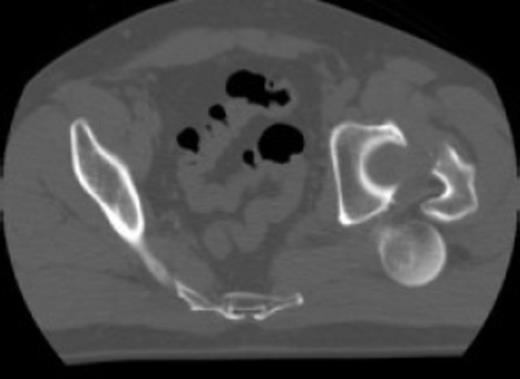
Posterior dislocation of the femoral head with no associated acetabular fracture
The patient was transferred to the Regional Trauma Unit where he underwent emergency open reduction and osteosynthesis within eight hours from injury.
The patient was positioned in the lateral decubitus position and a hard mass was palpable within the left buttock, a posterior approach was used via a curved posterior oblique incision. The femoral head was identified free within the gluteus maximus with no residual soft tissue attachments, the femoral head had buttonholed out through the capsule superior to the piriformis tendon. The short external rotators were incised with the residual posterior capsule and the acetabulum was cleared of any comminution fragments. The femoral head was accurately reduced and temporarily fixed with the antegrade placement of three guide wires exiting through the lateral femoral cortex. The guide wires were placed in a triangular configuration with the proximal end deep to the articular cartilage, this provided temporary stabilization of the fracture. The hip was carefully reduced and definitively fixed with three 6.5 mm retrograde partially threaded cannulated screws in the same configuration as the previously placed guide wires. Following fracture stabilisation the hip joint was stable to dislocation in all movements.
Postoperative care included early-supervised non-weight bearing mobilization for three months. Radiographs at three months showed no early displacement or evidence of avascular necrosis (Fig. 4). The patient progressed to protected full-weight bearing for a further three months.


At one year the patient was walking with a stick and mild limp, he had ninety degrees of hip flexion with limited internal and external rotation. Plain radiographs at this stage confirmed the fracture to be united with no evidence of avascular necrosis. The patient remained on yearly review and continued to function well. He returned to hobbies such as fishing and shooting and was pain free at three and a half years. The most recent review at four and a half years confirmed the presence of avascular necrosis (Fig. 5) however from a symptomatic point of view he is still able to maintain an active lifestyle with little pain.
DISCUSSION
Traumatic fracture dislocations of the hip are associated with high-energy injuries. The mechanism for a fracture of the femoral neck with posterior dislocation has been described as occurring in two stages – the initial dislocation followed by an adduction force resulting in the fracture (1). These injuries typically occur in the young active patient, 75% age less than fifty years, resulting in a treatment dilemma for the surgeon (7). A review of the literature does not result in a general consensus on whether this specific injury should be treated by primary open reduction and ostesynthesis or primary hip arthroplasty.
The literature describes 18 cases of posterior dislocation with combined femoral neck, femoral head or acetabular fracture. However there are only 5 cases of dislocation with an isolated femoral neck fracture. Of these five cases three were treated with hip arthroplasty and two with open reduction internal osteosynthesis (8).
In this case the patient was a young male who worked as a manual labourer. Although at the time of surgery there was no soft tissue attachment to the femoral head it was felt primary osteosynthesis was the treatment of choice because of both his age and occupation. A posterior approach was used as this was the direction of the dislocation, which resulted in significant disruption to the posterior tissues and it was felt preservation of anterior structures would protect both residual blood supply and hip stability. The best biomechanical stability for cannulated screws involves the placement of three screws in an inverted triangular configuration (4). The difficulties arising from this case was a technical issue in maintaining the reduction of the fracture to facilitate reduction of the hip joint prior to definitive stabilisation. Also following a posterior approach, with the leg in a flexed and internally rotated position, operative access to the lateral cortex of the femoral shaft is difficult and the use of intraoperative screening in the lateral decubitus position is awkward. These difficulties were resolved by using the technique described by placement of three antegrade guide wires buried deep to the articular surface. This provided a method of temporary stabilisation to facilitate reduction of the hip joint followed by accurate placement of three parallel-cannulated screws in the sunchondral bone without the requirement for intraoperative screening.
Although at almost 5 years from surgery this patient has subsequently developed avascular necrosis we did achieve stable fixation and fracture healing by the method described. Despite the radiological presence of avascular necrosis he continues to have satisfactory function for daily activities and has declined total hip arthroplasty. Although this is a rare injury with a high incidence of a poor outcome, we propose emergent internal fixation and osteosynthesis in these young patients, this method provides safe and reliable fixation overcoming the operative difficulties of surgical access and use of intraoperative imaging.



