-
PDF
- Split View
-
Views
-
Cite
Cite
C Tsue, Y Sakamoto, Y Nakajima, K Kishi, Potential pitfalls in volume reduction for the treatment of Proteus syndrome, Journal of Surgical Case Reports, Volume 2012, Issue 10, October 2012, Page 13, https://doi.org/10.1093/jscr/2012.10.13
Close - Share Icon Share
Abstract
Proteus syndrome is a rare congenital hamartomatous condition that is characterised by a wide range of malformations. Skin and skeletal developmental malformations are common and may manifest as significant physical anomalies. However, few reports have discussed surgical treatment.
A 37-year-old woman presented with disproportionate enlargement of the right buttock, which required volume reduction. The overgrown tissue was combined with vascular malformations, which in our patient were extremely thick. The patient experienced massive blood loss during the procedure, due to which a blood transfusion was performed.
Pathological findings revealed partial lipohyperplasia with venous malformations. Thus, during operations including incomplete excision, massive bleeding is always a possibility, but is not commonly described in these instances.
INTRODUCTION
Proteus syndrome is a rare congenital disorder with a highly variable clinical spectrum. Characteristically, the patients are normal at birth but progressively develop disease manifestations during childhood (1,2). Numerous case reports describe the clinical findings associated with the syndrome. However, to our knowledge, very few reports have discussed available treatment options. Previously we have described the surgical procedure and management of the craniofacial region (3). Here, we report a case that required volume reduction of the overgrown tissue naevi. The overgrown tissue was combined with vascular malformations, which in our patient were extremely thick. The patient suffered blood loss during the procedure, which is not commonly reported in these instances. In this report, we highlight potential pitfalls in the surgical treatment of dermal lesions.
CASE REPORT
A 37-year-old woman presented with disproportionate enlargement of the right buttock. A small 5 mm tumour was first observed in the right buttock when she was 12 years of age. Since then, the tumour gradually increased in size and the patient presented with a gigantic overgrowth of the right buttock, which extended significantly over the leg and toes. Facial features were unremarkable and her family history was not deemed to be contributory. The patient had already undergone a hysterectomy and right ovariectomy at another hospital when she was 25 years of age, because tumours of the uterus and right ovary were found. At the time, she had not yet been diagnosed with Proteus syndrome.
On first examination of the patient, we noticed that the right buttock resembled a cerebriform lesion. There were multiple nevi, which were distributed predominantly over the right waist, buttock, and right leg. These epidermal nevi had a mosaic distribution, but their location was limited to the right side (Fig. 1). Using the Proteus syndrome diagnostic criteria (4), we diagnosed this patient as having Proteus syndrome.

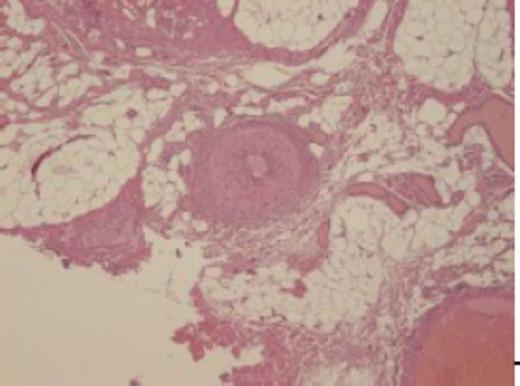
Histopathological findings. Note that the lesion is composed of lobules of mature fatty tissue with various sized vessels
The patient had difficulty sitting on a chair, and could not wear trousers; therefore, we sought to reduce the volume of the tumour. Volume reduction surgery of the right buttock lesion was performed under general anaesthesia. The buttock was divided into 3 areas: upper, middle, and lower. Both skin lesions and subdermal lesions were removed in the upper and lower areas. Although the medial side of the middle area was removed, the lateral side was retained to cover the defect, and just thinning of the subdermal tissue. At the time of reduction surgery, the perforators, which are ordinarily observed under a loupe, were visible to the naked eye and resembled primary vessels. A significant degree of haemorrhaging occurred from these enlarged vessels, which required a considerable amount of time to ligate. Finally, the reduction volume was chosen to achieve symmetry between the buttocks and femoral volume. In total, the reduction volume was 1350 g.

In order to adequately cover the excised region, we then elevated the skin flap. For the upper area, the bilobed flap was designed at the left buttock and positioned over the area of the defect. For the middle area, the remaining lateral-based skin lesion flap was restored. To close the wound under slight tension, the baggy medial skin lesion was trimmed to avoid creating dead space. For the lower area, the V-Y advancement flap was designed. In total, the operative time was 6 h 55 min. Total bleeding amounted to 1914 mL, and therefore, a blood transfusion was given. The pathological findings revealed partial lipohyperplasia with venous malformations (Fig. 2).
After 2 years, the patient was satisfied with the results, and was able to wear trousers and excrete easily; her quality of life (QOL) was also improved (Fig. 3).
DISCUSSION
Proteus syndrome is a rare, complex, and variable disorder characterized by the overgrowth of multiple tissues including the connective tissue nevi, the epidermal nevi, and the craniofacial hyperostosis (1). Of the numerous case reports on Proteus syndrome, most introduce clinical findings, and few describe surgical treatments for the disease (3,5,6). For the gigantic extremities, amputation is one surgical option (5). However, to improve postoperative QOL of the patients, we believe that volume reduction should be performed where possible.
Recent reports suggest that the most common histopathological features in Proteus syndrome are not limited to altered connective tissue nevi, but may also include vascular anomalies and lipomas (7,8). In our experience, Proteus syndrome is associated with lipohyperplasia with vascular anomalies. Therefore, for operations including incomplete excision, massive bleeding is always a possibility; therefore, the surgeons should be prepared for performing blood transfusions. Furthermore, electrosurgical vessel sealing tools such as LigaSure™ (Valleylab/Covidien) may be useful for the treatment of haemostasis, to fuse vessel walls and create a permanent seal, but also to shorten of the operative time (9).
In conclusion, we believe that publication of reports by attending surgeons in cases of Proteus Syndrome will allow for a comprehensive discussion of the disease, including the long-term course, preferred strategy for therapy, and an elucidation of the developmental mechanism.



