-
PDF
- Split View
-
Views
-
Cite
Cite
KE O’Sullivan, JB Conneely, JV Reynolds, Hyperemesis Gravidarum in a 37 Year-old Woman with a Gastric Band, Journal of Surgical Case Reports, Volume 2011, Issue 11, November 2011, Page 10, https://doi.org/10.1093/jscr/2011.11.10
Close - Share Icon Share
Abstract
The increasing availability of bariatric surgery services has seen the emergence of a series of significant complications. Many of these will present to centres without local bariatric expertise. In recognition of this, the American Society of Metabolic and Bariatric Surgery (ASMBS) has issued guidelines for non-bariatric surgeons to aid in the management of bariatric surgery related complications(2010). Implanted devices such as the adjustable gastric band require careful follow-up. In the context of pregnancy, it is recommended by some that the adjustable balloon be deflated to avoid complications, however, the device itself can still present a risk. We present a case that illustrates the necessity for maintaining a high index of suspicion of device-related complication.
INTRODUCTION
The increasing availability of bariatric surgery services has seen the emergence of a series of significant complications (1). We present the case of a patient who suffered such a complication during her pregnancy.
CASE REPORT
A 37 year-old woman at 10 weeks gestation was admitted to a maternity hospital with hyperemesis gravidarum. She had undergone gastric banding three years previously but had the band deflated prior to her planned pregnancy. Despite maximal medical therapy, she continued to experience intractable vomiting for four weeks. At this point, a surgical opinion was sought from the Upper G.I. service in a University Teaching Hospital. Clinical examination was consistent with mild dehydration. Haematological investigations revealed: Urea, 0.8 mmol/L; Cr, 22 μmol/L; K, 2.5 mmol/L; Alb, 26 g/L; Ca, 1.94 mmol/L; Phos, 0.23 mmol/L; Mg, 0.49 mmol/L.
The presumptive diagnosis was of band migration, and an urgent upper G.I. endoscopy was performed. This demonstrated a normal calibre proximal stomach, which narrowed sharply at the mid-body (fig 1.).

OGD showing a normal calibre proximal stomach, which narrowed sharply at the mid-body.
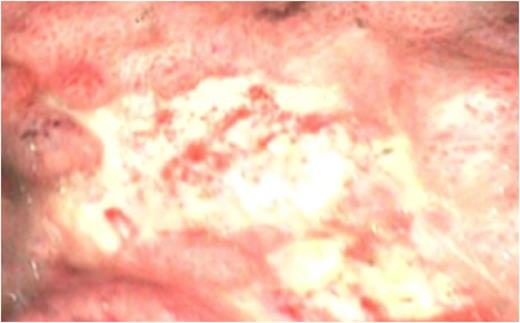
Multiple punctate mucosal lesions raised the suspicion of emerging gastric ischaemia secondary to band migration (fig.2), and the patient proceeded to an urgent laparoscopy.
This showed proximal herniation of the stomach through the band with dense omental adhesions, but no evidence of mural ischaemia. The band was disengaged and removed. Post-operative course was uneventful. Normal oral intake was resumed the following day and an Ultrasound scan confirmed a healthy intrauterine pregnancy. The patient was discharged two days later.
DISCUSSION
The prevalence of obesity worldwide is increasing dramatically, particularly amongst women of reproductive age. The WHO projects that 2.3 billion adults worldwide will be overweight by 2015, 700 million will be obese. This amounts to a significant rise on the current figures (WHO factsheet 311). (2)
Bariatric surgery has proven an invaluable tool in the fight against obesity in recent years and has been shown to reduce the long term mortality in operative candidates compared with those managed through medical or lifestyle means(Pontiroli and Morabito 2011).(3) Laparoscopic adjustable gastric banding (LAGB) has the advantage of being minimally invasive and reversible. It has therefore been the procedure of choice for the treatment of morbid obesity for several years in Europe. LAGB stands beside the roux-en y gastric bypass as the most frequently performed bariatric operation worldwide(Buchwald, Avidor et al. 2004; Davies, Maxwell et al. 2010). (4,5)
The escalating rates of obesity in the general population are mirrored in women of child bearing age. With respect to pregnancy, there are a myriad of antepartum, intrapartum, intraoperative, postoperative, and postpartum complications that are observed with a higher frequency in obese women compared with their healthy weight counterparts. In addition, the co-morbid medical conditions which accompany obesity prior to conception, such as hypertension and diabetes pose an additional threat(Buchwald, Avidor et al. 2004; Davies, Maxwell et al. 2010). (4,5)
Most case control studies demonstrate increased fertility associated with bariatric surgery, and LAGB has been shown to be safe in pregnancy, improving the prognosis of a previously obese mother (Bienstman-Pailleux and Gaucherand 2007).(6) Indeed, the risk of negative maternal and fetal outcomes can be reduced by LAGB if these patients are closely followed.
Clearly LAGB is associated with complications. In order of decreasing prevalence; pouch enlargement, band slippage, port displacement, band erosion, intrabdominal sepsis, port site infection and port breakage are most commonly reported in the literature. Overall prevalence of complications varies from 17.5 – 30% with rates of band removal reported at 12% (Eid, Birch et al. 2011; Stroh, Hohmann et al. 2011).(7,8) These complications also apply to the pregnant population, although less is known of the exact prevalence in that setting. Interestingl, clinical manifestations of complications include cessation of weight loss, epigastric pain, sepsis, with some patients remaining completely asymptomatic throughout (Stroh, Hohmann et al. 2011).(8) There is little mention of persistent vomiting as a known symptom of complication.
Nausea and vomiting is a common symptom, which accompanies pregnancy in 70-85% of all gravid women (Bottomley and Bourne 2009).(9) Hyperemesis gravidarum is a severe and intractable form of nausea and vomiting in pregnancy. Diagnosis is one of exclusion and may result in weight loss; nutritional deficiencies; and abnormalities in fluids, electrolyte levels, and acid-base balance. It is often unresponsive to medical interventions and takes time to resolve. The peak incidence is at 8-12 weeks of pregnancy, and symptoms usually dissipate by week 20 in all but 10% of patients.
This case highlights the ever-increasing need for a heightened awareness of the complications of bariatric surgery amongst both the obstetric and general surgical communities. Patients are undergoing bariatric procedures in escalating numbers and are therefore increasingly likely to present with complications to institutions without bariatric expertise. The gravid patient poses an added challenge and this case highlights an additional symptom of band erosion not previously documented. It has been proven that patients undergoing gastric banding often forget the complications associated with the procedure postoperatively and may be unlikely to highlight the issue to their healthcare provider(Madan, Tichansky et al. 2007).(10) It is therefore critical that a high index of suspicion for band related complications be maintained in all patients who have undergone LAGB and that expert bariatric advice be sought in a timely manner. In addition, adequate post operative follow-up and surveillance should be maintained to provide adequate support and continued guidance for these patients on an ongoing basis and by trained bariatric experts.



