-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Cai, Khurram Siddique, Michelle Hamer, Sanjoy Basu, Acute Chest Presentation following a Laparoscopic Nissen Fundoplication, Journal of Surgical Case Reports, Volume 2010, Issue 6, August 2010, Page 5, https://doi.org/10.1093/jscr/2010.6.5
Close - Share Icon Share
Abstract
We describe a case of an acute paraoesophageal hernia in the early post-operative period following a laparoscopic Nissen fundoplication. Patient developed intraoperative tension pneumothorax requiring an immediate chest drain and subsequently needed respiratory support of a continuous positive airway pressure (CPAP) ventilation. A short discussion of this rare but deleterious complication and the difficulty of making a prompt diagnosis are included as delayed revision surgery can be technically challenging with a poor outcome.
INTRODUCTION
Laparoscopic Nissen fundoplication is an established operative procedure with a low morbidity and mortality for patients with symptomatic hiatus hernias. However, a rare but a serious life-threatening complication: para-oesophageal hernia, can occur following an uneventful operation. We describe a case here that was initially a diagnostic conundrum, had a successful outcome following an early corrective surgery.
CASE REPORT
A 52-year-old fit and healthy gentleman with no previous cardiovascular or respiratory co-morbidity was admitted for an elective laparoscopic Nissen fundoplication.
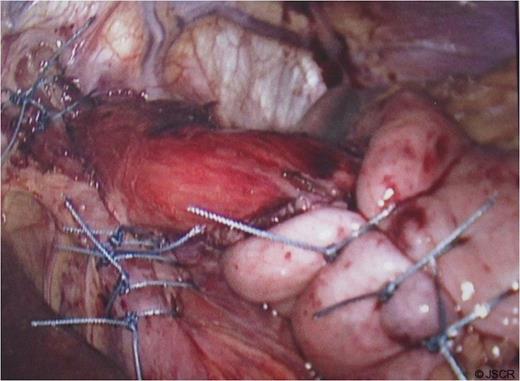
At operation, a large hiatal defect of 5cm and a moderate size sac was found (Fig 1) that was mobilised and adhesions divided to obtain 3cm of oesophageal length in the abdomen. Following division of the upper short gastric vessels, a posterior hiatal repair with seven interrupted ethibond stitches and a loose 360 degree full wrap with the fundus of the stomach with three interrupted ethibond stitches were performed. Wrap was further fixed to the diaphragm and right crus with another three ethibond stitches (Fig. 2).
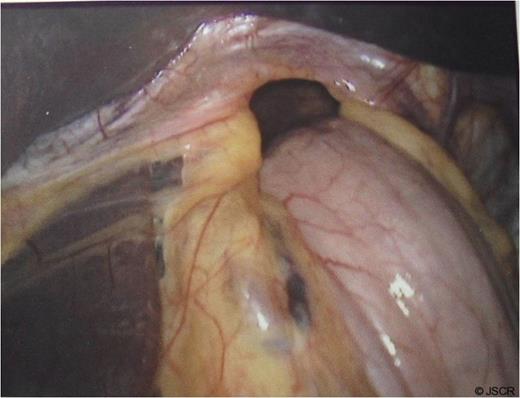
Hiatus hernia with portion of stomach seen going into the chest
During the sac dissection, the patient developed tension pneumothorax due to an iatrogenic tear of the right pleura requiring a chest drain. He was closely observed in the high dependency unit with pain relief through PCA (morphine) and intravenous paracetamol and oral feeding commenced post-operatively. Arterial blood gas showed pO2 of 10.7 and PCO2 of 6.54 on 60% oxygen and an early post-operative chest x-ray revealed bilateral pulmonary infiltration (Fig. 3). Non-cardiogenic pulmonary oedema was suspected and the patient was started on 5mmHg pressure CPAP.
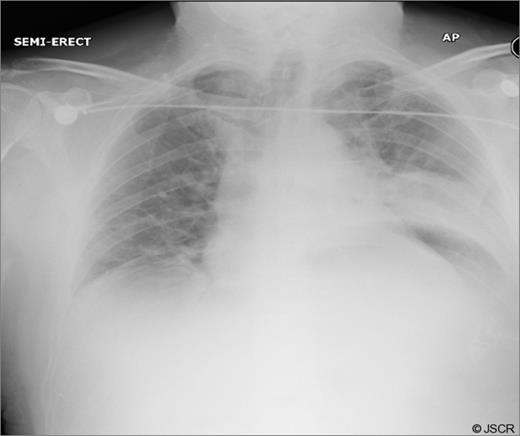
Early post-op chest x-ray showing patchy shadowing/ consolidation over the left side of chest
On day 1, patient complained of a central retro-sternal chest pain. In the absence of air leak, the right sided chest drain was removed and the PCA was increased to 1.5mcg boluses of morphine. Electrocardiogram revealed a sinus rhythm with no ST changes. Troponin I levels were raised at 0.1. Cardiology opinion was a myocardial trauma secondary to the operation.
Chest pain persisted and the patient required higher pressure CPAP to maintain adequate oxygenation. Auscultation consistently showed decreased air-entry in the lung bases. On day 3, a repeat chest x-ray showed a left lower lobe collapse above the gastric bubble in the mid zone of the chest (Fig. 4 & 5). CTPA done on the same day to exclude pulmonary embolism confirmed a para-oesophageal hernia that was pushing against the left lung base. Ultrasound scan of the left chest also showed movement of the diaphragm below the gastric bubble.
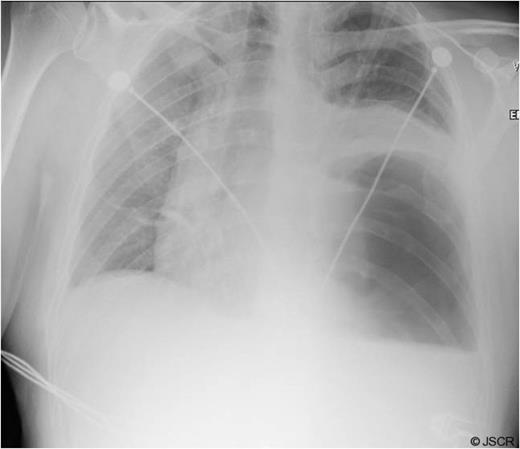
Chest x-ray on 3rd post-op day showing prominent left sided collapse/ consolidation

Post-op CT-scan demonstrating the left sided pleural effusion with collapse /consolidation & patchy opacification on the right side.
At laparotomy, 700ml of blood-stained fluid and a large paraoesophageal hernia involving the body of the stomach with vascular compromise that had slipped through the potential space between the wrap and the left crus into the left hemi-thorax created by extensive hiatal dissection was found. Hiatal repair and the 360 degree wrap fixed to the diaphragm and right crus were all completely intact. Reduction of the stomach restored the circulation and a gastropexy was done to the anterior abdominal wall with five interrupted ethibond stitches. A feeding jejunostomy was sited. Post-operatively, the patient suffered from acute lung injury requiring prolonged intubation and ventilation including a tracheostomy. He made a successful albeit a slow recovery and was discharged from the intensive care unit after 21 days.
DISCUSSION
Post-operative para-oesophageal hernia is a recognised but a rare and serious complication of laparoscopic Nissen fundoplication being reported in 0.8-6.7% cases (1-3). Higher prevalence has been reported following laparoscopic compared to open procedures (4). Reduced postoperative pain from adequate analgesia, early oral intake and return to activity raising the intra-abdominal pressure can lead to the development of early para-oesophageal hernias before true hiatal scar tissue formation. There is literature evidence of higher incidence amongst surgeons leaving the hiatus open compared to those closing it (5). Intra-operative left sided pneumothorax and the use of CPAP in the early post operative period has also been associated with the development of post-operative paraoesophageal hernias (6). Posterior hiatal cruroplasty, avoidance of postoperative retching and vomiting through regular use of prophylactic antiemetics reduces its frequency (7).
Patients with true paraoesophageal hernia present with dysphagia. However, they can be asymptomatic or can present with postprandial symptoms of gastric compression that includes chest pain and breathlessness (8). Prompt diagnosis is essential to prevent gastric necrosis, perforation, bleeding and even death (9). In patients with diagnostic dilemmas or suspicion for paraoesophageal hernias with previous laparoscopic Nissen fundoplication should undergo a contrast computerised tomography of the chest and abdomen or a barium swallow (2).
In our case, the operation was technically challenging due to the size of the hernia and the hiatal defect. However, the hernial sac was completely mobilised and a thorough posterior crural hiatal repair followed by a 360 degree wrap was performed. The wrap was further fixed to the diaphragm and right crus; thus closing any possible hiatal free space. The pneumothorax during the procedure was again on the right side settling uneventfully within 24 hours of the operation. The possible explanation for the development of this acute large paraoesophageal hernia in our case could be the immediate feeding and the distension of the stomach that was caused by the use of high CPAP post-operatively to maintain oxygenation: thus pushing the body of the distended stomach into the left chest through the dissected hiatus.
The persistent central retro-sternal chest pain with raised troponin and bilateral pulmonary infiltrations added confusion. There is literature evidence that varied clinical presentation can make diagnosis difficultand can even elude experienced radiologists as was evident here. Revision surgery can be technically challenging and is associated with higher morbidity (10). Our patient suffered an acute lung injury following the second surgery and required prolonged intubation, active support and extended hospital stay.
We present here such a case to remind us of the risk of non invasive ventilation in a post operative patient of laparoscopic Nissen fundoplication that was initially a diagnostic challenge, but, had a successful outcome due to the vigilant approach and a prompt surgical intervention.



