-
PDF
- Split View
-
Views
-
Cite
Cite
Joseph Ward, Vyomesh Bhatt, Neal Barnard, Malignant peripheral nerve cell sheath tumour of the upper lip: a rare case, Journal of Surgical Case Reports, Volume 2010, Issue 5, July 2010, Page 6, https://doi.org/10.1093/jscr/2010.5.6
Close - Share Icon Share
Abstract
We present the case of a malignant peripheral nerve sheath tumour (MPNST) that developed on the upper lip of an 86 year old woman. MPNSTs are highly aggressive sarcomas that very rarely occur in the face. We know of no other reported cases of a malignant peripheral nerve sheath tumour arising from the upper lip.
INTRODUCTION
Malignant peripheral nerve sheath tumours (MPNSTs) have an incidence of 1 per 1,000,000 people per year (1) and comprise around 3% of soft-tissue sarcomas (2). Tumours arise from Schwann cells or perineural cells that ensheath axons and extend along neural tracts. They are aggressive cancers that have high rates of recurrence and a poor prognosis (3). Occurrence in the head and neck region has been shown to be a predictor of adverse outcome. Up to half of all treated tumours will metastasize haematogenously (4). We can identify only two cases (5,6) in the literature of MPNST affecting the lips, in both instances the lower lips were affected. There were no reported cases of a malignant peripheral nerve sheath tumours originating from the upper lip. Here we report a case of MPNST situated in the midline of the upper lip involving the nasal floor and anterior alveolus.
CASE REPORT
An 86 year old woman presented with a painful lump on her upper lip extending into the dome and floor of the nose. The lesion had apparently enlarged over 4 weeks extending through the lip into the floor of the nose. Investigations included, fine needle aspiration (FNA), CT and MRI. A diagnosis of MPNST was made based on histological examination of an incisional biopsy (Fig. 1).
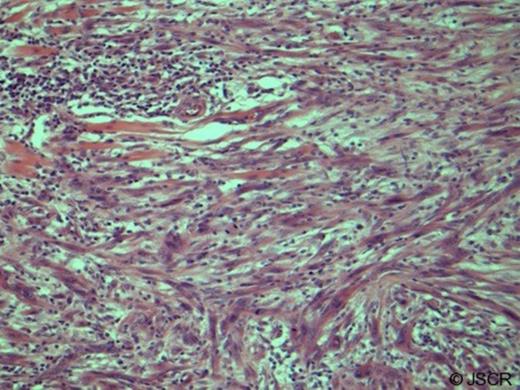
Malignant peripheral nerve sheath tumour showing pleomorphic, mitotically active spindle cells infiltrating the dermis and muscles of facial expression (haematoxylin and eosin, original magnification x20 low power). Immunohistochemistry showed that the lesion was an Actin+ S-100+ neoplasm providing diagnosis of MPNST.
The multidisciplinary team (MDT) decision was to resect the lesion with wide-margins (2cms in 3 dimensions) based on the high reported incidence of both perineural and perivascular spread6 in this tumour group, thus necessitating a rhinectomy, cheilectomy and anterior alveolectomy. The upper lip was reconstructed using a modified Karapandzic flap (Fig. 2, Fig. 3).
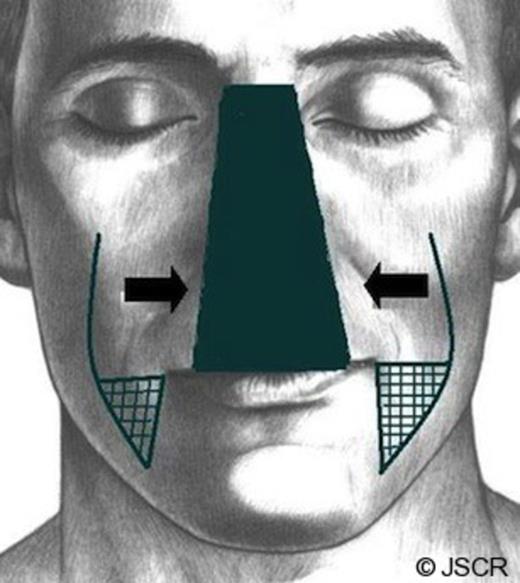
An illustration of a modified Karapandzic flap. The flap is raised around the nasal defect rather than the oral fissure to reconstruct the upper lip. The vermillion is reconstructed using mucosal advancement flaps from moth limbs of the reconstruction.

Osseointegrated implants were placed in the paranasal bone and remaining alveolus for prosthetic reconstruction of the nose. Operative margins were well clear of tumour on histopathological examination with no perineural or perivascular involvement. The option of adjunctive radiotherapy was offered but turned down by the patient. The patient remains under surveillance following rehabilitation with no evidence of recurrence at 16 months.
DISCUSSION
A recent small case series and review by Matin-Duverneeuil et al. identified 35 cases of MPNSTs in the maxillo-mandibular region over the last 70 years.(3) We know of only 2 cases of MPNSTs affecting the lips, although a few cases of benign schwannomas affecting the upper lip have been reported. (5,6) The rate of growth is probably attributable to the poorly understood but strongly genetic aetiology of MPNST. Neurofibromatosis-1 (NF-1) patients having been shown to be 113 times (7) more likely to develop MPNSTs than a standard population and microdeletions in the NF1 gene and over expression of proteins such as platelet derived growth factor receptors (PDGF) appear to be central events that predispose to increased lifetime risk of this disease with early onset. (1) Surgery is the accepted treatment of choice for well defined MPNSTs and the use of a Karapandzic flaps for upper lip reconstruction has previously been shown in a case series to produce reliable aesthetic and functional results. (8) Pathological confirmation of MPNSTs is difficult because FNA of MPNSTs has been reported to reveal an admixed range of divergent cell-types. Immunohistochemistry can cloud diagnosis because of variable immunoreactivity for the definitive neural marker, S-100. This tumour was S-100+ Actin+ allowing the diagnosis of MPNST to be confirmed post-resection. Adjuvant radiotherapy is effective at reducing the high local recurrence of MPNSTs but provides no survival benefit.1 Interestingly radiotherapy is also a risk factor for the disease accounting for 10% of cases.(9) Chemotherapy is understudied and as such is controversial for treating MPNST. It is reserved for aggressive unresectable cases.(10) Overall prognosis for MPNSTs is good with a 43% cause specific mortality at 10 years (4) but many patients suffer local recurrence with a consequent increase in related distant metastases (~90% of patients at post-mortem). Poor prognostic factors for recurrence and overall survival are the degree of cellular differentiation and tumour grade respectively.



