-
PDF
- Split View
-
Views
-
Cite
Cite
Amir Hossein Sarrami, Mohsen Sharifi, Majid Ahsan, Noushin Afsharmoghaddam, Multiple intestinal perforations as a primary manifestation of abdominal tuberculosis in a HIV-infected patient, Journal of Surgical Case Reports, Volume 2010, Issue 10, December 2010, Page 7, https://doi.org/10.1093/jscr/2010.10.7
Close - Share Icon Share
Abstract
Abdominal tuberculosis (TB) is the sixth commonest extra-pulmonary TB form after lymphatic, genitourinary, bone and joint, miliary and meningeal tuberculosis. Perforation is a serious and uncommon complication of abdominal tuberculosis which can occur even during the treatment. A 30-year-old man was admitted with a three-day history of abdominal pain who had emergency surgery for multiple perforations of the distal ileum.
INTRODUCTION
Abdominal tuberculosis (TB) is the sixth commonest extra-pulmonary TB form after lymphatic, genitourinary, bone and joint, miliary and meningeal tuberculosis. TB may involve any site of the gastrointestinal tract, but the commonest site of involvement is ileocecal region. Perforation is a serious and uncommon complication of abdominal TB. The authors present a case of abdominal TB which was manifested by multiple intestinal perforations.
CASE PRESENTATION
A 30-year-old man presented with a three-day history of abdominal pain. He was an intravenous drug addict with a positive serology for HIV and HCV. He had a history of anorexia, weakness and weight loss in last two weeks. Physical examination revealed pallor, hypotension and signs of peritoneal irritation. An upright chest X-ray showed presence of free intra-peritoneal air. The findings were compatible with diagnosis of peritonitis secondary to perforation; therefore an emergency laparotomy was carried out.
Surgical findings were of multiple perforations in the distal ileum and caecal perforations. Enlargement and thickening of mesenteric and regional lymph nodes were apparent. He was treated by ileal resection, right hemicolectomy, ileocolic anastomosis and peritoneal toileting.
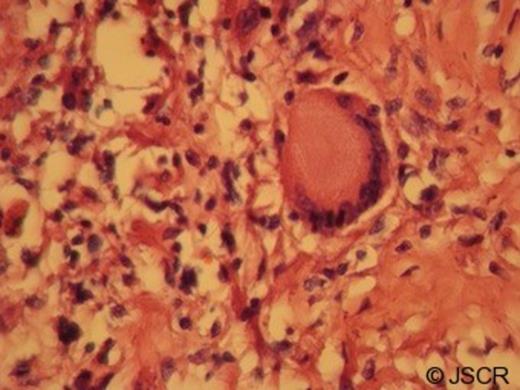
Macroscopically the ileum and caecum showed multiple caseating necrotic materials. On microscopic evaluation several caseating granulomatous inflammations composed of epithelioid histiocytes and Langhan’s giant cells were seen in the ileum, caecum and also mesenteric lymph nodes. Ziehl-Neelsen staining for Mycobacterium tuberculosis was negative. However, positivity of PCR assay for Mycobacterium tuberculosis on paraffin embedded tissue block confirmed the diagnosis.
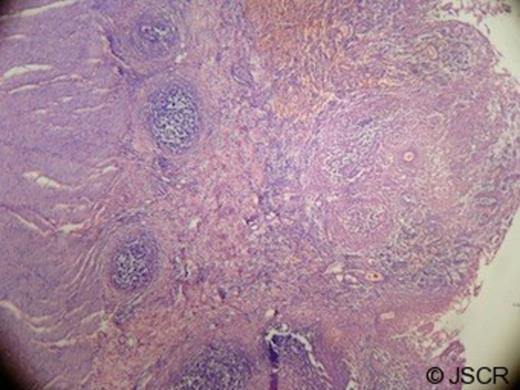
Low power photomicrograph showing mucosal ulceration of intestinal wall with hemorrhage and collection of lymphocytes (× 100)
No evidence of pulmonary tuberculosis was detected during further assessment. The patient was administered with anti-tuberculous therapy but unfortunately he died two months later.
DISCUSSION
HIV infection increases the risk of developing active tuberculosis and also modifies its clinical presentation. In HIV-infected patients extra-pulmonary TB ranges from 45 to 60%, and just in 5%, concomitant pulmonary TB exists. (1,2,3)
Abdominal TB is the sixth commonest extra-pulmonary TB form after lymphatic, genitourinary, bone and joint, miliary and meningeal tuberculosis. TB may involve any site of the gastrointestinal tract, but a majority of lesions occur in ileocecal region. (4,5,6)
Intestinal TB can present as an acute or chronic illness. This may be related to the microscopic features of the lesions which are divided into three forms: ulcerative, hypertrophic and ulcero-hypertrophic. (4) The host’s immune system influences the pattern of lesions. The ulcerative form which is associated with an acute and virulent clinical course occurs in those with a decreased immune response, while the hypertrophic form occurs in those with an increased immune response. (4) In our case, ulcerative form of the lesions might be due to immunosuppression induced by HIV.
The clinical manifestations of intestinal TB are nonspecific. Patients may present with abdominal pain, distention, altered bowel habit, nausea and vomiting. (5) Perforation is a serious and uncommon complication of intestinal TB. The low incidence of tubercular intestinal perforation which ranges from 1-15% can be owing to reactive fibrosis of the peritoneum. (2,5)
Definitive diagnosis of intestinal TB is established upon Ziehl-Neelsen staining for acid-fast bacilli, tissue culture and histology. In this case, we used PCR assay to facilitate diagnosis. PCR detection of mycobacteria is faster than culture (48 hours instead of weeks) and is useful for specimens which are not appropriate for culture. Moreover, it has high sensitivity and specificity which may be up to 82.6% and 95%, respectively. (7)
Histopathologic findings are very informative in diagnosis of intestinal TB. Characteristic histological features are submucosal and serosal caseating granuloma. Generally, it is recommended to interpret histopathologic findings in conjunction with culture or PCR results in order to enhance diagnostic accuracy. (8,9)
Surgical decision for patients with tubercular intestinal perforation depends upon general state of the patient, condition of the gastrointestinal tract and number of perforation. However, perforation may be fatal, even with surgical intervention. (6)
In conclusion, TB could be a potential cause of the acute abdomen in the HIV-infected patients. Surgeons should be aware of tubercular intestinal perforation and give close attention to immunocompromised patients.



