-
PDF
- Split View
-
Views
-
Cite
Cite
Baijaeek Sain, Vishal Patel, Going solo: TightRope as the sole fixation method for lateral end clavicle fractures, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf728, https://doi.org/10.1093/jscr/rjaf728
Close - Share Icon Share
Abstract
Lateral end clavicle fractures, especially those that are displaced, have a high rate of delayed and non-union. This case series presents three patients with unstable lateral end clavicle fractures successfully treated with TightRope fixation as the sole method of stabilization, demonstrating excellent functional outcomes and minimal complications. The comprehensive literature review reveals mounting evidence with eight reported studies supporting TightRope as an effective standalone treatment option, with the largest published series showing 79% union rates and only 10% complication rates. These findings, combined with the theoretical advantages of avoiding routine hardware removal, lower costs, and compatibility with day-surgery protocols, suggest that TightRope fixation merits serious consideration as a primary treatment modality for appropriately selected patients with lateral end clavicle fractures.
Introduction
Unstable lateral end clavicle fractures, particularly Neer type II and IV, are associated with high non-union rates when managed non-operatively [1–3]. Traditional surgical options, such as hook plates and locking plates, while effective, are often complicated by hardware irritation, need for removal, and technical challenges in small or comminuted fragments. A simple, minimally invasive surgical technique using suture fixation can also be done; however, the literature is limited to this technique [4]. The TightRope system, which provides coracoclavicular stabilization through a minimally invasive approach, has emerged as an alternative that may address these limitations [5–8]. This report presents a case series of three patients treated with TightRope fixation as the sole method of stabilization, supplemented by a comprehensive review of the literature, to evaluate the efficacy, safety, and practical considerations of this technique.
Surgical technique
The patients were placed in beach chair position on a shoulder table with an image intensifier being used intra-operatively. An antero-superior horizontal incision approximately between 3–4 cm long was used, extending from the dorsal ridge of the clavicle and extending distally till the tip of the coracoid. Skin flaps were raised, and the fascia split longitudinally in line with the clavicle. The coracoid was adequately exposed. A 3.5 mm drill was used to drill separate holes in the clavicle and the coracoid, and the drill was wiggled to slightly increase the diameter of the hole to accommodate the 4 mm button passing through. It is recommended leaving a 2 cm gap between the drill hole medially in the clavicle shaft and the lateral fracture site on the clavicle. The coracoid drill position is usually near the base of the coracoid and centrally to reduce the risk of lateral blowout fracture. Arthrex endo-button system was used. A guide wire was used to pass the button through the clavicle and subsequently through the coracoid. It was retrieved and then pulled back to ensure it has flipped and is secure against the coracoid. The clavicle was reduced as best as possible, ensuring the optimal distance between the undersurface of the clavicle and the coracoid. The desired tension was finalized, and button secured further with knots. As a secondary measure, the threads that are attached to the coracoid button are then tied over with the threads from the tied clavicle button to reduce the bulkiness of the knot and to reinforce the repair.
Case series
Case 1
A 15-year-old male sustained a displaced Neer type IV lateral clavicle fracture during a rugby match, presenting with acute pain, deformity, and dorsal displacement without neurovascular compromise (Fig. 1). Imaging confirmed the diagnosis, and open reduction with TightRope and Fiber-wire reinforcement was performed. Early rehabilitation was initiated following short-term immobilization. At 6 weeks, the patient achieved pain-free shoulder function and radiographic stability. By four months, he regained full range of motion and returned to non-contact sports. Minor peri-scar numbness persisted, but imaging confirmed fracture union, and he was cleared for contact activities (Fig. 2A–B).
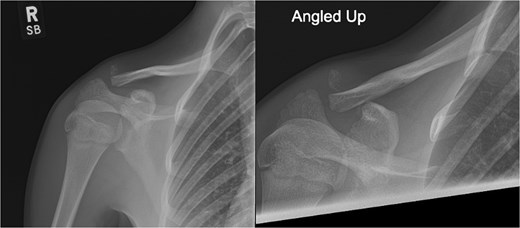
Radiographs of first case showing a displaced Neer type IV lateral clavicle fracture with deformity and displacement.
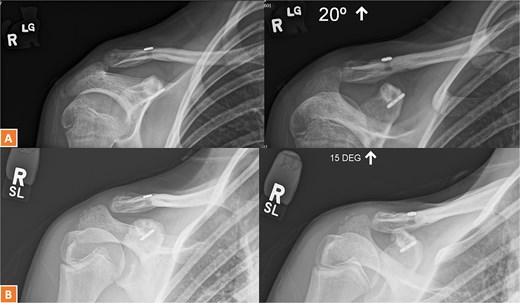
(A, B) Radiographs showing complete healing of the first case and union at 3 months and 12 months post-operatively.
Case 2
A 30-year-old male presented with an unstable lateral clavicle fracture and skin tenting after a rugby injury. Imaging revealed a Neer type IV equivalent fracture (Fig. 3). He underwent open reduction and internal fixation with coracoid exposure and TightRope placement, reinforced with fiber-wire. Postoperative recovery included sling immobilization followed by pendular exercises. Despite delayed radiological union, he achieved full range of motion and strength by three months, with only mild, asymptomatic clavicular prominence. He returned to physically demanding work without restrictions, and final imaging confirmed union (Fig. 4A–C).
Radiographs of second case showing a displaced lateral end clavicle fracture with deformity and dorsal displacement.
(A–C) Radiographs showing complete healing of the second case and union at 3, 6, and 12 months post-operatively.
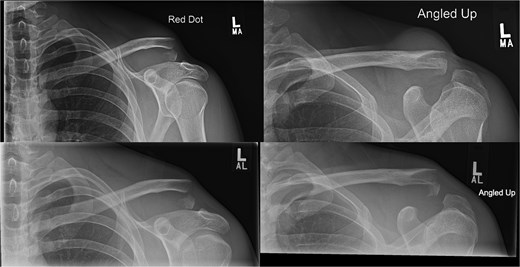
Case 3
A 27-year-old male suffered a right lateral clavicle fracture after a fall (Fig. 5). He underwent TightRope fixation with stabilization of the coracoclavicular ligament. Rehabilitation was initiated early, and by three months, he had full shoulder motion and returned to overhead sports. Radiographs confirmed union, and the patient reported minor scar sensitivity and transient keloid formation, with no functional limitations (Fig. 6A–D).

Radiographs of third case showing a displaced lateral clavicle fracture with deformity.
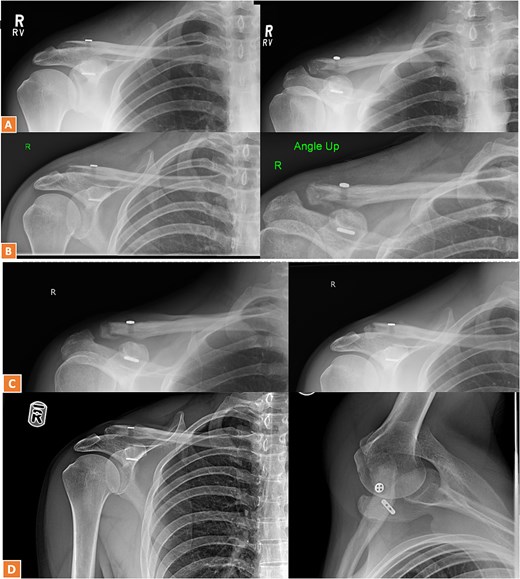
(A, B) Radiographs showing healing of the third case and radiological union at 6 weeks and 3 months post-operatively. (C–D) Radiographs showing complete healing of the third case and union at 6 months and 12 months post-operatively.
Discussion
Accurate fracture classification was critical, particularly in identifying coracoid involvement. All patients were young, active, and required robust fixation to allow early mobilization. The surgical approach involved open reduction, careful drill hole placement (at least 2 cm medial to the fracture on the clavicle and central in the coracoid), and reinforcement with fiber-wire if needed (Table 1).
Table showing patient demographic details of patients fixed with TightRope only for lateral end clavicle fractures
| Timeline and events . | Case 1 (15-year-old) . | Case 2 (30-year-old) . | Case 3 (27-year-old) . |
|---|---|---|---|
| Injury | Rugby injury with displaced Neer IV fracture | Rugby collision with unstable lateral fracture | Fall resulting in lateral clavicle fracture |
| Presentation | Dorsal displacement, intact neurovascular status | Skin tenting, stable neurovascular examination | Localized tenderness, stable examination |
| Surgery | ORIF with titanium TightRope and Fibrewire reinforcement | ACJ stabilization via TightRope | ORIF using TightRope (Arthrex) |
| 6 weeks | Pain-free function (90° elevation, full ER, 10° IR) | Pendular exercises, acceptable alignment | Progressive rehabilitation, wound healing |
| 3 months | Radiographic stability, progressive rehabilitation | Full ROM and strength, transient prominence | Maintained alignment, full motion, mild aching |
| 6 months | Full ROM, symmetrical strength, sports clearance | Return to demanding employment | Return to tennis and overhead activities |
| Final follow-up at 12 months | Non-contact sports resumption, transient numbness | Discharge with asymptomatic elevation | Oxford Score 46/48, minor scar sensitivity |
| Timeline and events . | Case 1 (15-year-old) . | Case 2 (30-year-old) . | Case 3 (27-year-old) . |
|---|---|---|---|
| Injury | Rugby injury with displaced Neer IV fracture | Rugby collision with unstable lateral fracture | Fall resulting in lateral clavicle fracture |
| Presentation | Dorsal displacement, intact neurovascular status | Skin tenting, stable neurovascular examination | Localized tenderness, stable examination |
| Surgery | ORIF with titanium TightRope and Fibrewire reinforcement | ACJ stabilization via TightRope | ORIF using TightRope (Arthrex) |
| 6 weeks | Pain-free function (90° elevation, full ER, 10° IR) | Pendular exercises, acceptable alignment | Progressive rehabilitation, wound healing |
| 3 months | Radiographic stability, progressive rehabilitation | Full ROM and strength, transient prominence | Maintained alignment, full motion, mild aching |
| 6 months | Full ROM, symmetrical strength, sports clearance | Return to demanding employment | Return to tennis and overhead activities |
| Final follow-up at 12 months | Non-contact sports resumption, transient numbness | Discharge with asymptomatic elevation | Oxford Score 46/48, minor scar sensitivity |
Table showing patient demographic details of patients fixed with TightRope only for lateral end clavicle fractures
| Timeline and events . | Case 1 (15-year-old) . | Case 2 (30-year-old) . | Case 3 (27-year-old) . |
|---|---|---|---|
| Injury | Rugby injury with displaced Neer IV fracture | Rugby collision with unstable lateral fracture | Fall resulting in lateral clavicle fracture |
| Presentation | Dorsal displacement, intact neurovascular status | Skin tenting, stable neurovascular examination | Localized tenderness, stable examination |
| Surgery | ORIF with titanium TightRope and Fibrewire reinforcement | ACJ stabilization via TightRope | ORIF using TightRope (Arthrex) |
| 6 weeks | Pain-free function (90° elevation, full ER, 10° IR) | Pendular exercises, acceptable alignment | Progressive rehabilitation, wound healing |
| 3 months | Radiographic stability, progressive rehabilitation | Full ROM and strength, transient prominence | Maintained alignment, full motion, mild aching |
| 6 months | Full ROM, symmetrical strength, sports clearance | Return to demanding employment | Return to tennis and overhead activities |
| Final follow-up at 12 months | Non-contact sports resumption, transient numbness | Discharge with asymptomatic elevation | Oxford Score 46/48, minor scar sensitivity |
| Timeline and events . | Case 1 (15-year-old) . | Case 2 (30-year-old) . | Case 3 (27-year-old) . |
|---|---|---|---|
| Injury | Rugby injury with displaced Neer IV fracture | Rugby collision with unstable lateral fracture | Fall resulting in lateral clavicle fracture |
| Presentation | Dorsal displacement, intact neurovascular status | Skin tenting, stable neurovascular examination | Localized tenderness, stable examination |
| Surgery | ORIF with titanium TightRope and Fibrewire reinforcement | ACJ stabilization via TightRope | ORIF using TightRope (Arthrex) |
| 6 weeks | Pain-free function (90° elevation, full ER, 10° IR) | Pendular exercises, acceptable alignment | Progressive rehabilitation, wound healing |
| 3 months | Radiographic stability, progressive rehabilitation | Full ROM and strength, transient prominence | Maintained alignment, full motion, mild aching |
| 6 months | Full ROM, symmetrical strength, sports clearance | Return to demanding employment | Return to tennis and overhead activities |
| Final follow-up at 12 months | Non-contact sports resumption, transient numbness | Discharge with asymptomatic elevation | Oxford Score 46/48, minor scar sensitivity |
Strengths and limitations
This series demonstrates TightRope fixation’s versatility across age groups and fracture patterns, with all patients achieving union and excellent function. Limitations include the small sample size, lack of a comparative control group, and one case with adjunctive lateral plating.
Literature review
The largest published series by Al-Tawil et al. evaluated 29 patients with displaced lateral clavicle fractures treated exclusively with TightRope [9]. Union was achieved in 79% of cases, with a low complication rate (10%), and functional outcomes were consistently good (mean Oxford Shoulder Score 41). Complications were minor, including adhesive capsulitis, hardware prominence, and coracoid button migration. Other reports and small series corroborate these findings, with most patients achieving full union and rapid return to activities.
Minimally invasive and arthroscopic techniques are evolving, offering further reduction in soft tissue trauma and improved cosmesis. However, not all patients are candidates for these approaches due to risk of coracoid fracture, particularly if the entire load is borne by a single implant.
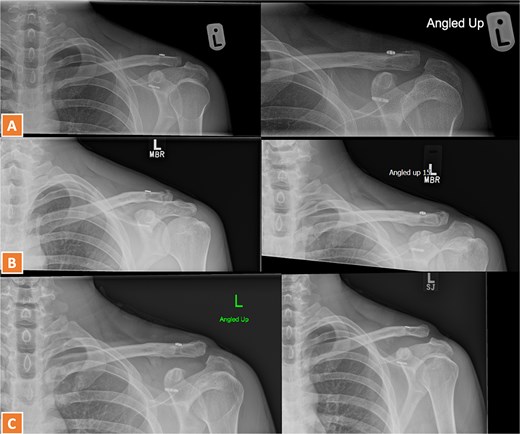
Biomechanical and technical considerations
The acromioclavicular joint is where most of the rotational movement happens mechanically. This rotation occurs through the fracture site following a fracture. Since the clavicle fracture is very lateral and the intact coracoclavicular ligaments hold the distal fragment of the clavicle in place, the clavicle, once released from its lateral attachments, is left to rotate through the fracture in the simplest manner possible, resulting in delayed union [2–4].
TightRope fixation provides flexible stabilization, more closely mimicking natural ligament function than rigid plates, and allows early mobilization. The technique distributes load across button interfaces, reducing stress concentration compared to screw-based systems. Key technical points include maintaining adequate bone stock by placing the clavicular drill hole at least 2 cm medial to the fracture and central placement of the coracoid drill hole to minimize risk of cortical blow-out. The open approach remains standard, though arthroscopic and percutaneous methods are emerging (Fig. 7).
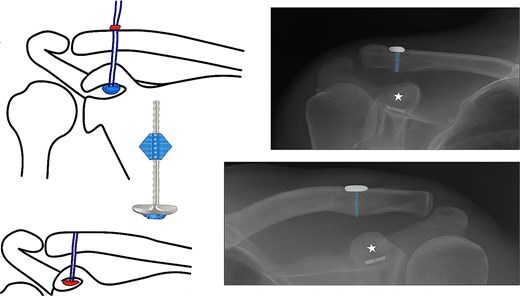
Schematic diagram of fixation of lateral end clavicle with TightRope alongside corresponding radiographic reference points for the surgical technique.
Complications
The overall complication rate is low, with most issues being minor and manageable, such as hardware irritation or migration. The risk of coracoid fracture is minimized by careful surgical technique and patient selection. Compared to hook plates, which require routine hardware removal and are associated with higher rates of stiffness and infection, TightRope offers significant advantages in both safety and patient satisfaction.
Comparative outcomes
The comparative analysis of surgical outcomes reveals several findings (Table 2). Union rates demonstrated significant variability across studies, with Al-Tawil et al. (2020) reporting the lowest rate at 79% and five investigations achieving perfect union rates [9]. This 21% disparity likely reflects differences in surgical techniques, with Motta et al. utilizing arthroscopic TightRope stabilization, while Zheng et al. (2019) employed a minimally invasive closed-loop approach [10, 11]. Patient demographics may also contribute, as Al-Tawil's cohort included older patients (mean age 36, range 14–73) compared to Meena et al.'s younger population (mean 29.5 years).
Table showing detailed review of literature of previously reported eight-studies on the usage of TightRope for fixation of lateral end clavicular fracture with their outcomes
| Study (year) . | Design . | Sample size . | Mean age (range) . | Gender (M/F) . | Fracture type (Neer) . | Follow-up . | Union rate . | Complications . | Key findings . |
|---|---|---|---|---|---|---|---|---|---|
| Al-Tawil et al. (2020) [9] | Retrospective | 29 | 36 (14–73) | 72% M, 28% F | Type II | 21 months | 79% (22/28) | 10% (3/29): Adhesive capsulitis (1), Hardware removal (1) | Tightrope achieved OSS 41, EQ5D 0.78. 93% return to pre-injury activity level. |
| Motta et al. (2014) [10] | Case Series | 14 | Not Reported | 100% M | IIA (2), IIB (10), V (2) | 2 years | 100% | 14% (2/14): Delayed healing (1), Coracoid tunnel breach (1) | Arthroscopic TightRope stabilization allowed full return to activities (Constant score: 95). |
| Soh et al. (2011) [12] | Case Report | 1 | 24 | 0% M, 100% F | Type IIB | 12 weeks | 100% | None reported | Pain-free ROM at 12 weeks using TightRope. |
| Mičeta et al. (2022) [13] | Case Report | 1 | 48 | 0% M, 100% F | Type IIB | 3 months | 100% | None reported | Full ROM and return to daily activities post-TightRope fixation. |
| Meena et al. (2023) [14] | Retrospective | 37 | 29.5 (19–46) | 81% M, 19% F | IIA (12), IIB (19), V (6) | 6.1 years | 95% (35/37) | 13.5% (5/37): Non-union (2), AC arthritis (3) | Long-term Constant score 93.38. 89% maintained reduction at 6-year follow-up. |
| Yang et al. (2021) [15] | Case Report | 1 | 34 | Not reported | Type IIA | 12 weeks | 100% | None reported | Minimally invasive approach with fluoroscopic guidance. |
| Robinson et al. (2010) [16] | Case Series | 16 | <60 years | 81% M, 19% F | Lateral clavicle fractures | 1 year | 94% (15/16) | 6% (1/16): Asymptomatic fibrous union | Twin Endobutton technique achieved mean Constant score 87.1. No reoperations. |
| Zheng et al. (2019) [11] | Retrospective | 15 | 36.5 (18–65) | 73% M, 27% F | Neer II | 9 months | 100% | None reported | ASES 92.4, Constant 93.7. Return to function at 3.8 months. |
| Study (year) . | Design . | Sample size . | Mean age (range) . | Gender (M/F) . | Fracture type (Neer) . | Follow-up . | Union rate . | Complications . | Key findings . |
|---|---|---|---|---|---|---|---|---|---|
| Al-Tawil et al. (2020) [9] | Retrospective | 29 | 36 (14–73) | 72% M, 28% F | Type II | 21 months | 79% (22/28) | 10% (3/29): Adhesive capsulitis (1), Hardware removal (1) | Tightrope achieved OSS 41, EQ5D 0.78. 93% return to pre-injury activity level. |
| Motta et al. (2014) [10] | Case Series | 14 | Not Reported | 100% M | IIA (2), IIB (10), V (2) | 2 years | 100% | 14% (2/14): Delayed healing (1), Coracoid tunnel breach (1) | Arthroscopic TightRope stabilization allowed full return to activities (Constant score: 95). |
| Soh et al. (2011) [12] | Case Report | 1 | 24 | 0% M, 100% F | Type IIB | 12 weeks | 100% | None reported | Pain-free ROM at 12 weeks using TightRope. |
| Mičeta et al. (2022) [13] | Case Report | 1 | 48 | 0% M, 100% F | Type IIB | 3 months | 100% | None reported | Full ROM and return to daily activities post-TightRope fixation. |
| Meena et al. (2023) [14] | Retrospective | 37 | 29.5 (19–46) | 81% M, 19% F | IIA (12), IIB (19), V (6) | 6.1 years | 95% (35/37) | 13.5% (5/37): Non-union (2), AC arthritis (3) | Long-term Constant score 93.38. 89% maintained reduction at 6-year follow-up. |
| Yang et al. (2021) [15] | Case Report | 1 | 34 | Not reported | Type IIA | 12 weeks | 100% | None reported | Minimally invasive approach with fluoroscopic guidance. |
| Robinson et al. (2010) [16] | Case Series | 16 | <60 years | 81% M, 19% F | Lateral clavicle fractures | 1 year | 94% (15/16) | 6% (1/16): Asymptomatic fibrous union | Twin Endobutton technique achieved mean Constant score 87.1. No reoperations. |
| Zheng et al. (2019) [11] | Retrospective | 15 | 36.5 (18–65) | 73% M, 27% F | Neer II | 9 months | 100% | None reported | ASES 92.4, Constant 93.7. Return to function at 3.8 months. |
Table showing detailed review of literature of previously reported eight-studies on the usage of TightRope for fixation of lateral end clavicular fracture with their outcomes
| Study (year) . | Design . | Sample size . | Mean age (range) . | Gender (M/F) . | Fracture type (Neer) . | Follow-up . | Union rate . | Complications . | Key findings . |
|---|---|---|---|---|---|---|---|---|---|
| Al-Tawil et al. (2020) [9] | Retrospective | 29 | 36 (14–73) | 72% M, 28% F | Type II | 21 months | 79% (22/28) | 10% (3/29): Adhesive capsulitis (1), Hardware removal (1) | Tightrope achieved OSS 41, EQ5D 0.78. 93% return to pre-injury activity level. |
| Motta et al. (2014) [10] | Case Series | 14 | Not Reported | 100% M | IIA (2), IIB (10), V (2) | 2 years | 100% | 14% (2/14): Delayed healing (1), Coracoid tunnel breach (1) | Arthroscopic TightRope stabilization allowed full return to activities (Constant score: 95). |
| Soh et al. (2011) [12] | Case Report | 1 | 24 | 0% M, 100% F | Type IIB | 12 weeks | 100% | None reported | Pain-free ROM at 12 weeks using TightRope. |
| Mičeta et al. (2022) [13] | Case Report | 1 | 48 | 0% M, 100% F | Type IIB | 3 months | 100% | None reported | Full ROM and return to daily activities post-TightRope fixation. |
| Meena et al. (2023) [14] | Retrospective | 37 | 29.5 (19–46) | 81% M, 19% F | IIA (12), IIB (19), V (6) | 6.1 years | 95% (35/37) | 13.5% (5/37): Non-union (2), AC arthritis (3) | Long-term Constant score 93.38. 89% maintained reduction at 6-year follow-up. |
| Yang et al. (2021) [15] | Case Report | 1 | 34 | Not reported | Type IIA | 12 weeks | 100% | None reported | Minimally invasive approach with fluoroscopic guidance. |
| Robinson et al. (2010) [16] | Case Series | 16 | <60 years | 81% M, 19% F | Lateral clavicle fractures | 1 year | 94% (15/16) | 6% (1/16): Asymptomatic fibrous union | Twin Endobutton technique achieved mean Constant score 87.1. No reoperations. |
| Zheng et al. (2019) [11] | Retrospective | 15 | 36.5 (18–65) | 73% M, 27% F | Neer II | 9 months | 100% | None reported | ASES 92.4, Constant 93.7. Return to function at 3.8 months. |
| Study (year) . | Design . | Sample size . | Mean age (range) . | Gender (M/F) . | Fracture type (Neer) . | Follow-up . | Union rate . | Complications . | Key findings . |
|---|---|---|---|---|---|---|---|---|---|
| Al-Tawil et al. (2020) [9] | Retrospective | 29 | 36 (14–73) | 72% M, 28% F | Type II | 21 months | 79% (22/28) | 10% (3/29): Adhesive capsulitis (1), Hardware removal (1) | Tightrope achieved OSS 41, EQ5D 0.78. 93% return to pre-injury activity level. |
| Motta et al. (2014) [10] | Case Series | 14 | Not Reported | 100% M | IIA (2), IIB (10), V (2) | 2 years | 100% | 14% (2/14): Delayed healing (1), Coracoid tunnel breach (1) | Arthroscopic TightRope stabilization allowed full return to activities (Constant score: 95). |
| Soh et al. (2011) [12] | Case Report | 1 | 24 | 0% M, 100% F | Type IIB | 12 weeks | 100% | None reported | Pain-free ROM at 12 weeks using TightRope. |
| Mičeta et al. (2022) [13] | Case Report | 1 | 48 | 0% M, 100% F | Type IIB | 3 months | 100% | None reported | Full ROM and return to daily activities post-TightRope fixation. |
| Meena et al. (2023) [14] | Retrospective | 37 | 29.5 (19–46) | 81% M, 19% F | IIA (12), IIB (19), V (6) | 6.1 years | 95% (35/37) | 13.5% (5/37): Non-union (2), AC arthritis (3) | Long-term Constant score 93.38. 89% maintained reduction at 6-year follow-up. |
| Yang et al. (2021) [15] | Case Report | 1 | 34 | Not reported | Type IIA | 12 weeks | 100% | None reported | Minimally invasive approach with fluoroscopic guidance. |
| Robinson et al. (2010) [16] | Case Series | 16 | <60 years | 81% M, 19% F | Lateral clavicle fractures | 1 year | 94% (15/16) | 6% (1/16): Asymptomatic fibrous union | Twin Endobutton technique achieved mean Constant score 87.1. No reoperations. |
| Zheng et al. (2019) [11] | Retrospective | 15 | 36.5 (18–65) | 73% M, 27% F | Neer II | 9 months | 100% | None reported | ASES 92.4, Constant 93.7. Return to function at 3.8 months. |
Complication profiles showed patterns, with hardware-related issues predominating in studies using traditional fixation methods. Al-Tawil et al. (2020) documented a 10% complication rate, including one hardware removal, while Meena et al. (2023) reported 13.5% complications with two non-unions [9, 14].
Surgical approach comparisons revealed equivalent efficacy across modalities when performed appropriately. Motta et al. achieved 100% union arthroscopically, while Robinson et al. attained 94% success with open reduction [10, 16]. Percutaneous techniques described by Yang et al. produced comparable outcomes to more invasive methods, though longer-term data remain limited [15]. Functional scores showed remarkable consistency, with Constant scores ranging 87.1–95 across approaches, indicating technique selection should consider surgeon expertise and patient factors rather than presumed superiority of any single method.
Union rates range from 79% to 100%, with non-union being rare. The fibrous union in Robinson et al. occurred in an open approach cohort, contrasting with the infection-free outcomes in arthroscopic series [16]. In our series, complete fibrous union took place at the fracture site. Complications are infrequent and mostly minor, such as transient stiffness.
The lower profile implants in this technique seem to have better functional and radiological results in the short and medium term. They also cause less irritation than hook plates or pins, which lowers the re-operation rate. Additionally, they do not require bony purchase on small, potentially comminuted lateral fragments like locking plates do. Because it eliminates the need for a second removal process, this method has a major advantage over hook plates. It helps with lateral end clavicle plates, which can be noticeable and need to be removed again, or they can fail to keep the coracoclavicular ligaments reduced. We are confident in maintaining reduction by securing the reduction of the medial clavicle segment directly, without the assistance of the lateral fragment or acromion. The TightRope device also has the advantage of being substantially less expensive than hook or locking plates.
Patient perspective
All patients reported satisfaction with outcomes, rapid return to activity, and minimal discomfort. Minor complaints included transient numbness and scar sensitivity, but no patient required further intervention or expressed dissatisfaction.
Conclusion
TightRope fixation as the sole method for unstable lateral end clavicle fractures yields consistently favorable outcomes, including high union rates, excellent functional recovery, and a low complication profile. The technique offers practical advantages over traditional fixation, such as avoidance of routine hardware removal, lower cost, and compatibility with outpatient protocols. Current evidence, though limited to small series and case reports, strongly supports TightRope as a primary treatment option for appropriately selected patients. Larger prospective comparative studies are warranted to further define its role and long-term outcomes in orthopedic practice.
Conflict of interest statement
None declared.
Funding
None declared.
Ethical approval
Not required given study design.
References
Zheng YR, Lu YC, Liu CT. Treatment of unstable distal-third clavicule fractures using minimal invasive closed-loop double endobutton technique. J Orthop Surg Res 2019;14:37.



