-
PDF
- Split View
-
Views
-
Cite
Cite
Primoz Potocnik, Luisa Lotter, Andreas Toepfer, Volker J Schmidt, Orthoplastic tarsal reconstruction using a chimeric vascularized bone graft in a heavy smoker: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf715, https://doi.org/10.1093/jscr/rjaf715
Close - Share Icon Share
Abstract
Vascularized reconstruction of bone defects in the foot after osteomyelitis is a complex procedure that requires an orthoplastic collaboration. This case demonstrates the successful use of a free osteocutaneous fibula flap with a perforator-based skin island to reconstruct the medial midfoot following a late-onset infection after fusion for osteonecrosis. A 63-year-old woman presented after osteonecrosis and failed surgeries, including talonavicular and naviculocuneiform arthrodesis complicated by infection. Given the patient’s smoking and infection history, revision using avascular bone grafts was not an option. A vascularized fibula graft and a perforator-based skin island were used to reconstruct the medial column and the soft tissue. The patient was free of pain and had full ankle mobility at 12 months. Reconstructing large postosteomyelitic foot defects is challenging. Vascularized bone and soft tissue flaps are essential to ensure healing and stability. Proper risk stratification and backup surgical strategies are critical for high-risk patients.
Introduction
Vascularized reconstruction of large-scale bone defects at the foot following osteomyelitis is a challenging task that requires an excellent interdisciplinary clinical setup between orthopaedic and plastic surgeons. This specific interdisciplinary field is usually referred to as ‘orthoplastics’. In this short report, we applied a free osteocutaneous fibula flap, including a perforator-based skin island, to reconstruct the medial column of the midfoot following a late-onset infection after talonavicular and naviculocuneiform fusion for osteonecrosis of the navicular bone in a smoking patient with low compliance as a last-resort treatment to avoid partial foot amputation. Our key learning was that applying sophisticated reconstructive techniques, which ensure proper vascularization, can resolve longstanding processes of chronic pain and repeated operations, even in multimorbid patients with low compliance. This underscores the importance of delivering vascularization to chronic wound environments.
Case presentation
A 63-year-old woman suffering from osteonecrosis and subsequent loss of the navicular bone was referred to our interdisciplinary orthoplastic outpatient clinic because of chronic pain in her right foot (Fig. 1). The patient was initially diagnosed with osteonecrosis of the navicular bone 2 years ago. Since then, we have performed multiple orthopaedic operations, including talonavicular as well as naviculocuneiform I and II arthrodesis, using an autogenous iliac bone graft. The patient required removal of the implant and thorough debridement of the bone due to an infection. This resulted in the patient being unable to walk on the affected foot. The patient had various comorbidities, including systemic sclerosis, chronic pain syndrome, polyarthritis, and nicotine addiction. It was clear from previous hospital stays that the patient struggled to comply with strict nicotine abstinence.
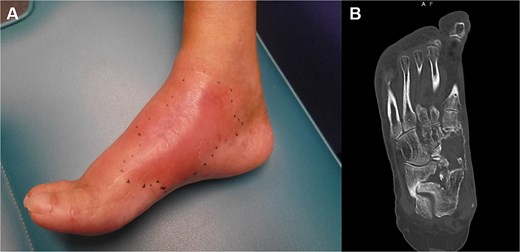
(A) The initial appearance of the affected right foot shows swelling and oedema at the dorsomedial aspect of the midfoot. The CT scan shows that the medial midfoot column has a bony defect following debridement for a late-onset infection. (B) This infection occurred after failed reconstructive attempts using avascular autologous bone grafts and arthrodesis.
Given the patient history and compliance, another attempt at revision surgery using avascular bone grafts was not an option. This left two possible therapeutic procedures: partial foot amputation or vascularized bone grafting with simultaneous soft tissue reconstruction due to the lack of soft tissue and scarring. After a thorough discussion, the patient opted for vascularized tarsal reconstruction.
The orthoplastic approach involved subtalar arthrodesis and the use of a 3.8 cm vascularized free fibula graft from the contralateral leg to reconstruct the medial metatarsus (Fig. 2). The vascularized bone was placed between the talus and the distal remains of the medial cuneiform bone and fixed with a low-profile medial column plate (3.5 mm medial column plate, Arthrex Inc., Naples, FL), spanning from the talus to the first metatarsal (Fig. 3). The remaining dead space was filled with additional autologous cancellous bone. The free fibula flap was harvested together with a perforator-based 10 × 1.5 cm skin island, which was used to reconstruct the subsequent soft tissue defect (Figs 2 and 3). The microanastomosis was performed end to end to the dorsalis pedis artery and to the great saphenous vein (GSV) using a 2 cm vein graft from the GSV. Initial healing went uneventfully, but the patient repeatedly left the ward to smoke and failed to follow our training requirements for lower extremity reconstruction—placing the leg in a horizontal position for 5 days. Three days after surgery, we performed a revision of the venous anastomosis due to immediate venous flap congestion. Further partial skin grafting was performed on the skin island to address the transient volume increase of the flap. The further postoperative follow-up was successful, and the flap healed well (Fig. 3). Furthermore, the bone healed successfully. At the 12-month follow-up, the patient was able to walk without pain and with a full range of motion in the ankle (Fig. 4).
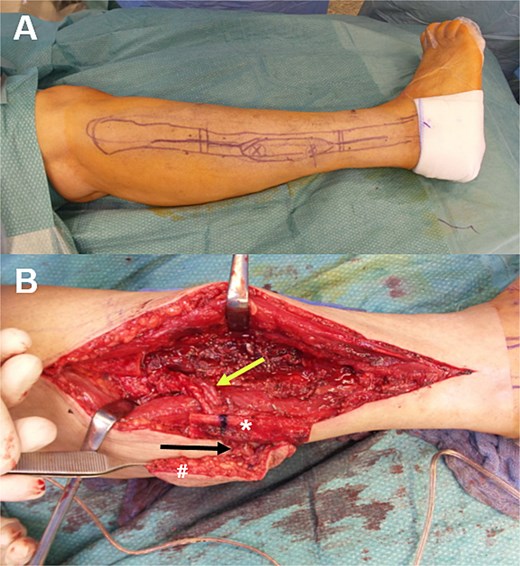
(A) The fibula bone graft resection sites and the perforator-based skin flap are marked. Perforator mapping was performed using colour-coded duplex ultrasound. The intraoperative situation (B) clearly shows the main pedicle containing the fibular artery (top arrow), the vascularized fibula bone graft (*), and the perforator-based (bottom arrow) soft-tissue island (#).
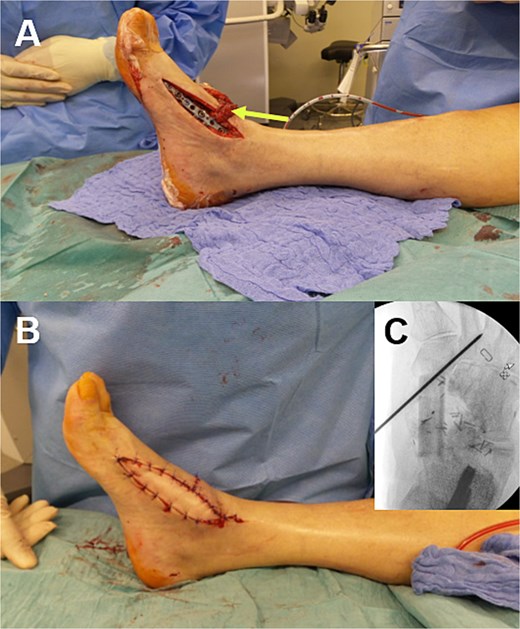
(A) The vascularized bone graft is fixed using a low-profile medial column plate. We ensure that the perforator to the skin island (arrow) and the main pedicle of the chimeric flap are carefully preserved during plate fixation. (B) The final intraoperative result. It demonstrates proper coverage of the soft tissue defect and plate by means of the perforator-based skin island. (C) An intraoperative X-ray scan of the temporarily fixed bone graft with a K-wire.

Six months after surgery, the final result shows a stable coverage with an adequate range of active motion regarding (A) dorsal extension and (B) plantar flexion. (C, D) The bone graft is fully integrated.
Discussion and conclusion
Reconstruction of large bony defects of the foot is challenging, particularly after multiple operations following osteomyelitis, where thorough debridement is often necessary. In rare cases, these clinical situations require the use of vascularized bone transplants and a vascularized soft tissue flap. This is the only way to address both the healing and stability of the bone as well as adequate coverage of the applied osteosynthesis material. In patients who have suffered loss of bone, painful midfoot instability and lack of mobility after several attempts of nonvascularized bone grafting, the only alternatives to these demanding interdisciplinary orthoplastic reconstructions are partial foot amputations or other below-knee amputations [1]. Furthermore, in patients with a low level of compliance and major risk factors, such as heavy smoking, the use of high-end microsurgical procedures, such as chimeric free flaps, should be considered [2, 3].
In this case, we did not fully anticipate the lack of compliance during the early postoperative period. Otherwise, we would not have agreed to the complex therapy plan.
These complex cases must be addressed in an interdisciplinary orthoplastic team approach, including multistage preoperative discussion, to obtain informed consent from the patient. Secondary lifeboat procedures (e.g. partial foot amputation) must be outlined in detail to the patient prior to the reconstructive microsurgical approach [4]. In summary, complex high-end reconstructions are suitable for high-risk patients if proper risk stratification, multistage informed consent, and a reliable alternative surgical backup strategy are present.
Conflict of interest statement
None declared.
Funding
None declared.



