-
PDF
- Split View
-
Views
-
Cite
Cite
Qudus Olajide Lawal, Ade Isenalumhe, Governor B O Okome, Mojeed Momoh, Joseph Ikheloa, Charles Igene, Sharon Emordi, Julius Arebun, Unseen scars: a case report on clitoral epidermal inclusion cyst and its influence on female body perception, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf672, https://doi.org/10.1093/jscr/rjaf672
Close - Share Icon Share
Abstract
Clitoral cyst is an epidermal inclusion cyst that results from invagination of the epidermis into the dermis or subcutaneous tissue. It commonly occurs following trauma from female genital mutilation (FGM), with presentation typically in childhood or the peripubertal period. Later, presentations often arise due to the asymptomatic nature of the condition and the associated stigma. Most previous reports have focused on cyst size, spontaneous aetiology, or its association with FGM. In this case report, we present an unusual case of a large clitoral cyst in a 38-year-old woman who had previously been denied treatment on three occasions at different healthcare facilities. She reported feeling like a ‘man’ all her life, reflecting a distressing negative body image. She subsequently had cyst excision and reported improved self-esteem.
Introduction
The clitoris and female genital tract play a central role in a woman’s sense of femininity and are key indicators of her genital health and well-being. Clitoral cysts, a form of clitoral disorder, can disrupt both the anatomy and function of the genital region, potentially affecting a woman’s physical and psychological health. These cysts are reported more frequently in African and Asian countries, where the prevalence of female genital mutilation (FGM) is high [1, 2].
Clitoral cysts arise when epidermal cells become embedded in the underlying dermis, leading to the formation of a cyst lined by stratified squamous epithelium [3]. Although trauma from FGM is the most common cause, spontaneous cases have also been documented [3]. These cysts typically appear as painless, slow-growing swellings of the clitoris during childhood or adolescence. However, diagnosis is often delayed due to the asymptomatic nature of the condition, the clitoris’s concealed anatomical position, and the stigma surrounding medical consultation for female genital concerns [2]. Treatment involves surgical excision (enucleation) of the cyst and reconstructive surgery to restore the normal anatomy and function of the external genitalia.
Although clitoral cysts can significantly alter genital anatomy, their psychological impact is rarely discussed in the literature. Genital appearance can affect both sexual and marital satisfaction [4, 5]. Beyond the visible enlargement of the clitoris, untreated clitoral cysts may cause psychological trauma. This case report presents the management of a 38-year-old woman who experienced profound body image distress due to a large clitoral cyst.
Case report
We report the case of a 38-year-old multiparous woman with a clitoral swelling first noticed in childhood. Initially, the size of a pea, the swelling gradually increased over the years to approximately the size of a small fist. She reported no associated pain, dyspareunia, bleeding, discharge, or similar swellings elsewhere on her body. There was no history of genital birth trauma or previous genital surgery; however, she did have a positive history of childhood FGM.
She had no significant past illnesses, chronic medical conditions, or systemic diseases. She reported no menstrual irregularities, urinary tract symptoms, previous genital lesions, or reproductive difficulties. Aside from the clitoral swelling, she had no history of genital trauma, surgery, or recurrent infections, and no evidence of other cystic lesions or chronic dermatologic conditions elsewhere on her body. While she had undergone FGM in childhood, she reported no long-term complications such as chronic pain, infections, or urinary dysfunction typically associated with FGM. There was also no prior surgical intervention related to the genital tract or pelvic region.
The patient expressed dissatisfaction with her genital appearance, describing a sense of masculine identity due to the cyst’s size and its resemblance to a penis. She felt shame and embarrassment, with a negative self-evaluation, and avoidance of sexual intimacy. The distress was profound, affecting her marital intimacy and emotional well-being.
On examination, she had a large, globular clitoral mass measuring 12 × 7 cm at its widest point. The mass was mobile, cystic in consistency, and non-tender (Figs 1 and 2). The overlying skin was intact with no ulceration or discharge. The urethral meatus was visible upon cephalad displacement of the mass, and the meatus appeared normal. Both labia minora and majora were healthy, with no signs of virilization. No other abnormalities were found on general examination. Adjacent genital structures, including the vaginal introitus, perineum, anus, mons pubis, and surrounding skin, appeared normal. There was no inguinal lymphadenopathy, and the lower abdomen was soft, non-tender, and without palpable masses. No signs of virilization or systemic illness were observed.


Diagnosis and surgical management
This absence of complicating medical, surgical, or systemic history supports the diagnosis of a solitary epidermal inclusion cyst on the clitoris (clitoral cyst), likely resulting from traumatic implantation of epidermal elements during the FGM procedure in early life. The patient was counselled on the diagnosis and the treatment options.
She underwent surgical excision under spinal anaesthesia. A vertical incision was made at the apex of the swelling, and careful dissection was carried out along the cyst wall plane (Fig. 3). Sharp dissection at the base ensured complete removal of the cyst (Fig. 4). The resulting dead space was closed, and the external genitalia were reconstructed to restore its normal anatomy, with minimal intra-operative blood loss (Fig. 5). The postoperative recovery was uneventful, and she was discharged on the second postoperative day.
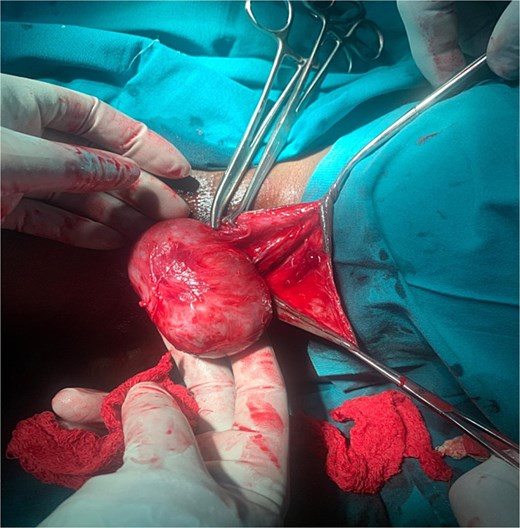
Enucleation of the clitoral cyst through midline incision made on the ventral surface.


Clinical assessments, at 3 and 7 weeks postoperatively, showed complete wound closure without infection, dehiscence, or necrosis. The surgical site had good epithelialization, healed surrounding tissue, and restoration of normal genital anatomy. The patient experienced no significant pain or functional issues (Fig. 6). In addition, she reported an improved body image, relief from discomfort during intercourse, and improved marital intimacy.

The diagnosis of an epidermal inclusion cyst was confirmed through histopathological examination, which reveals a cyst wall lined by true stratified squamous epithelium containing all the typical skin layers, including a prominent stratum granulosum, filled with laminated keratinous material [6].
Discussion
Clitoral cysts frequently arise as long-term complications of FGM, particularly Type 1, and are more common in areas where FGM is practiced [7]. A prospective study in Benin City found that 41.2% of children experiencing FGM-related complications had clitoral cysts [8]. Most cases present in childhood or adolescence. However, due to their typical asymptomatic nature and the stigma surrounding female genital conditions, some clitoral cysts present late or go unreported [2]. In a retrospective study of 21 cases in Somalia, the mean age at presentation was 33 ± 14.89, which is similar to the age at presentation of our patient [1]. Cultural myths surrounding female genitalia, combined with misinformation about the impact of genital surgery on fertility, perpetuate fear, and cause a delay in seeking treatment [9].
The cyst comes in varying sizes, distorting the normal anatomy of the female genitalia with consequent impact on body image perception. These changes to the external genitalia can lead to identity conflicts, self-esteem issues, and impaired sexual relationships, as reported in FGM survivors. Dissatisfaction with genital appearance has been closely linked to poor sexual esteem and satisfaction, as observed in the patient [5].
Negative body image resulting from an enlarged clitoris due to clitoral cysts can significantly disrupt a woman’s sexual self-concept and intimate relationships, leading to reduced sexual desire, avoidance of sexual activity, and emotional distress during intimacy [5]. In parallel, FGM could impair sexual functioning and satisfaction through both physical alterations and the psychological trauma it induces [5]. For this patient, the coexistence of a large clitoral cyst and a history of FGM likely compounded the impact on her sexual well-being. The cyst not only physically altered her genital appearance but also symbolically reinforced the violation associated with FGM, deepening her sense of shame and loss of femininity. This layered experience of trauma, disfigurement, and dysfunction reflects how two related, but distinct conditions can interact synergistically, amplifying psychological distress and impairing quality of life. The patient’s perception of her genitalia as masculine further illustrates the gender identity conflict that can arise in such contexts.
Although the surgical intervention was primarily undertaken to excise the large clitoral cyst, it simultaneously addressed multiple, deeply intertwined consequences of the patient’s prior FGM. The procedure removed the cyst, enabled the reconstruction of the external genitalia, and in doing so, partially reversed some of the visible effects of the original cutting due to the FGM. Thus, the surgery not only offered relief from physical discomfort, particularly dyspareunia, but renewed the sexual function of the clitoris. In addition, the removal of a disfiguring mass and the restoration of a more typical genital appearance may have contributed to the patient’s improved body image and increased confidence in intimate settings, thereby addressing the marked psychosexual sequelae of FGM. Thus, the surgical excision and reconstruction went far beyond the management of a cyst; it represented a reparative intervention for the long-term consequences of FGM. It effectively addressed the compounded issues of disfigurement, chronic pain, and impaired self-image, illustrating the potential of focused surgical care to restore not only anatomy, but also dignity and quality of life in survivors.
Conclusion
Clitoral cysts can have a significant impact on both physical and psychological health of affected individuals. Timely surgical intervention can restore the anatomy, relieve symptoms, and improve self-perception and sexual function. Raising awareness, providing appropriate counselling, and ensuring access to surgical care are essential to improving outcomes for women affected by this condition.
Acknowledgements
We acknowledge the roles of Dr Andrew Okoh, Dr Aituma Lewis, Dr Kadiri Haliru, Dr Oarhe Friday, Dr Best Izuyon, Dr Esther Yomere Ayeomeretse, and Dr Gladys Ibrahim in the management of the patient.
Author contributions
Qudus Olajide Lawal conceptualize and wrote original draft, Julius Arebun was part of the conceptualization, Joseph Ikheloa, Ade Isenalumhe, Sharon Emordi, and Charles Igene reviewed and edited the manuscript, and Governor B.O. Okome and Mojeed Momoh reviewed and edited the manuscript and also provided supervision. All authors read and approved the final manuscript.
Conflict of interest statement
None declared.
Funding
None declared.
Ethics approval and consent to participate
Ethics approval was obtained from Irrua Specialist teaching hospital, Human research ethics committees, Approval number ISTH/HREC/20250904/703.
Consent for publication
Informed consent obtained.



