-
PDF
- Split View
-
Views
-
Cite
Cite
Zia Ur Rehman, Rabia Chang, Anam Ghauri, Cutaneous mucormycosis in a young immunocompetent host – a case report, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf374, https://doi.org/10.1093/jscr/rjaf374
Close - Share Icon Share
Abstract
Cutaneous mucormycosis is a rare disease, which commonly affects immunocompromised individuals. It is highly invasive with devastating outcomes. Prompt actions such as surgical debridement and early initiation of antifungals are necessary to prevent the infection's rapid progression. Unfortunately, due to its rarity and frequent negative fungal cultures, diagnosis, and treatment are often delayed. Here, we have described a case of a young immunocompetent individual with cutaneous mucormycosis of the arm. Her diagnosis was made on clinical suspicion, later confirmed with tissue histopathology. She underwent surgical debridement and was started on antifungals. Unfortunately, due to the rapid spread of the infection, an amputation became necessary to prevent further complications.
Introduction
Mucormycosis is a rare and devastating fungal infection caused by fungi belonging to the order Mucorales [1]. The commonly affected systems are pulmonary and rhino-orbital [2]. Cutaneous mucormycosis (CM) is a rare presentation of the disease, frequently seen in immunocompromised patients or individuals with diabetes mellitus. CM has two forms, the superficial CM, which usually occurs in immunocompetent hosts and the disseminated form commonly occurring in immunocompromised patients [3]. Limbs are the most commonly affected areas by CM [2]. Diagnosis of mucormycosis, especially in immunocompetent individuals, is usually delayed due to its rarity. Timely diagnosis and appropriate interventions are necessary to prevent its devastating complications. Here, we present a case of a young immunocompetent female with mucormycosis of the upper limb.
Case presentation
A young girl in her early 20s, with no known comorbidities, presented to the vascular surgery clinic with a painful, large, and non-healing wound on her right arm. There was no previous history of any trauma to the arm. According to the patient, she initially had an abscess, which was treated at an outside hospital facility with incision and drainage. Later, due to the worsening condition of the wound, she underwent wound debridement, with no clinical improvement in her condition. Her outside histopathology report was negative for malignancy, and tissue cultures showed heavy growth of Pseudomonas aeruginosa sensitive to Meropenem.
At the time of her presentation, she was conscious, alert, and awake. She was afebrile and vitally stable and was not taking any medications. Her wound was tender and large, covering the entire anterior aspect of her right arm, with overlying necrotic tissue. Her C-reactive protien count was elevated. She was admitted for further workup and surgical management.
Upon admission, she was started on relevant antibiotics according to the available tissue cultures and underwent wound debridement under general anesthesia. Samples were sent for biopsy; tissue, fungal, acid fast bacillus (AFB) cultures, and GeneXpert. Post-operatively, she was continued with broad-spectrum antibiotics and daily dressings of the wound with acetic acid.
Her pain was managed, and she underwent daily limb physiotherapy as well. Her tissue cultures again reported heavy growth of P. aeruginosa sensitive to meropenem and ciprofloxacin. Fungal, AFB cultures, and gene Xpert were reported negative. Biopsy reports were still pending. She remained afebrile during her hospital admission, and the wound seemed to be improving. Therefore, she was discharged on IV antibiotics and daily dressings with acetic acid.
On follow-up to the clinic on postoperative day 6, she was doing well. Her wound was improving, had some necrotic tissue for which bedside debridement was done and antibiotics were continued. She was advised to return to the clinic with final histopathology reports after a week.
However, on the second follow-up visit to the clinic, she had worsening pain and limited range of motion at her elbow joint, despite being regular with her medications and dressings. She also reported a new fever spike 2 days ago. On examination, the wound had worsened with increasing necrotic tissue and surrounding erythema (Fig. 1).

The whole arm was edematous, with evident flexion contracture at the elbow joint. The median nerve was intact. Ulnar and radial could not be assessed due to excessive edema. Her histopathology reports showed chronic granulomatous inflammation and invasive fungal infection, likely mucormycosis, and were negative for malignancy (Figs 2 and 3).
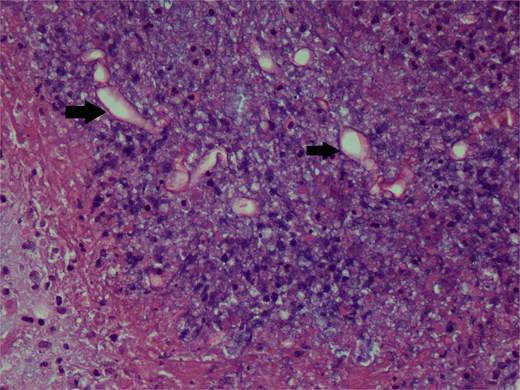
Hematoxylin and eosin stain photomicrograph showing fungal hyphae.
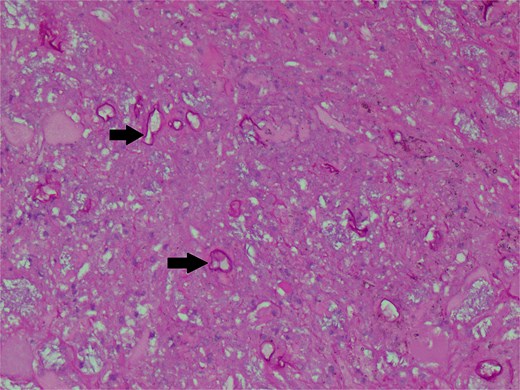
Periodic Acid Schiff stain photomicrograph showing broad-based aseptate fungal hyphae and spores (arrows).
She was advised admission; Infectious Diseases team was taken on board and was started on IV amphotericin B with pre-hydration.
She again underwent wound debridement under general anesthesia. Intraoperatively, it was found that all underlying muscles were necrotic. After discussion with Infectious Diseases and the patient, it was decided that the infection was spreading rapidly, and source control was necessary for the patient's improvement. Therefore, the patient was counselled and referred to orthopedics for assessment of shoulder disarticulation. Magnetic resonance imaging of the right arm was done, which showed necrotic muscles in the anterior and posterior compartments of the arm extending up to the axilla. The neurovascular bundle was encased by the necrotic tissue with a narrow caliber of the brachial artery. The patient was counselled regarding the need for shoulder disarticulation. They agreed and opted for another facility for the procedure due to financial reasons.
Discussion
Mucormycosis is an invasive fungal infection caused by the order Mucorales; Rhizopus, Mucor, and Lichtheimia being the most common genera [1]. It can lead to severe outcomes such as multiorgan failure and sepsis, especially in vulnerable populations such as those with immunosuppression or diabetes, emphasizing the need for early recognition and intervention.
It has various presentations in human beings, rhinocerebral and pulmonary being the most common, followed by cutaneous [2]. According to one study, a prevalence of 0.14/1000 population and 38% mortality of CM was reported in Pakistan [4]. It is commonly found in patients with an immune deficiency. However, some cases have been reported in immunocompetent patients, usually associated with trauma [5]. Due to its rarity, especially in immunocompetent patients, its diagnosis is often delayed. Fungal cultures are often reported as negative [6], as was in our case, further complicating the diagnostic process. Some studies have advocated early initiation of antifungal therapy even before the definitive histopathology confirmation, to improve outcomes [7, 8]. Early surgical intervention also plays a crucial role in controlling the source and to avoid the spread of the infection to underlying fascia, muscles, and bones [9]. In our case, surgical debridement was done timely, but unfortunately, due to the rapid spread of the infection, amputation became necessary.
Owing to the high mortality rates, devastating complications, and difficult diagnostic process, having a high index of suspicion is critical. Increasing awareness among clinicians is important for improving prognosis and mitigating the burden of mucormycosis on the healthcare system.
Conflict of interest statement
None declared.
Funding
None declared.



