-
PDF
- Split View
-
Views
-
Cite
Cite
Evelyne Wassef, Maher Al-Khaldi, François Dagbert, Éric De Broux, Marianne Gagnon-Konamna, Rasmy Loungnarath, Richard Ratelle, Carole Richard, Frank Schwenter, Ramses Wassef, Herawaty Sebajang, Left paraduodenal hernia, a diagnostic challenge, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf669, https://doi.org/10.1093/jscr/rjaf669
Close - Share Icon Share
Abstract
Left paraduodenal hernias, an abnormal protrusion of abdominal organs through a peritoneal defect into the fossa of Landzert, are a rare cause of small bowel obstruction. We present the case of a 21-year-old man with intermittent abdominal pain over several months. Diagnostic laparoscopy confirmed a left paraduodenal hernia. The hernia was reduced, and the fossa of Landzert was left widely open. This condition presents a diagnostic challenge, as symptoms are non-specific and imaging may appear unremarkable. Prompt diagnosis is essential to avoid complications such as strangulation and ischemia. Unlike conventional approaches, our surgical strategy involved enlarging and intentionally leaving the hernial defect open—justified by anatomical and pathophysiological reasoning. At 21-month follow-up, the patient remained symptom-free. This case highlights the importance of maintaining a high index of suspicion in similar clinical presentations and proposes an alternative surgical technique for managing this rare internal hernia.
Introduction
Internal hernias are defined as an abnormal protrusion of an abdominal organ or viscera through a peritoneal or mesentery defect and can be a rare cause of small bowel obstruction [1–7]. Multiple types of internal hernias exist (paracecal, transmesenteric, and transcolic), but by far the most common type, representing ⁓30%–53% of internal hernias, is the paraduodenal hernia [5, 6, 8, 9] first described in the 18th century [10], and found in 2% of the population during autopsies [3, 4, 8, 10–12]. It was later classified into left and right paraduodenal hernias, both caused by a malrotation of the midgut during the embryological period. In the left paraduodenal hernia (LPDH), most commonly found in men in their 4th or 5th decade of life [3, 11], this malrotation creates a peritoneal fossa, the fossa of Landzert, situated behind the descending mesocolon, bordered anteromedially by the left colic artery and the inferior mesenteric vein, and through which the small bowel can herniate [1, 4, 5, 8, 10]. As it is a rare cause of small bowel obstruction, accounting for ˂1% of cases [3, 8], and its clinical presentation is often non-specific with paroxysmal episodes of abdominal pain or acute abdominal pain, its preoperative diagnosis is challenging [1–6, 8–14]. Early treatment is required as it can lead to ischemia of the herniated bowels and mortality rates as high as 20%–50% have been reported [1, 5, 6, 10, 11].
Case presentation
A 21-year-old man, with no medical or surgical history, presented to a community emergency department with a history of intermittent abdominal pain, accompanied by nausea and vomiting, worsened by meals. Initial blood tests and computed tomographic (CT) scan were deemed normal. However, given the discrepancy between the patient’s presentation and the normal paraclinical findings, he underwent a diagnostic laparoscopy. The small bowel was explored in its entirety and was found to be almost entirely located in a retroperitoneal fossa, on the left side of the ligament of Treitz, establishing the diagnosis of a left paraduodenal hernia. The hernia was reduced, and the defect left unrepaired. In the early post-operative period, the patient returned to the emergency department of a tertiary center with recurrent obstructive symptoms. A second CT scan (Figs 1–3) was performed and, on this occasion, a left paraduodenal hernia was identified. Retrospectively, this finding was also visible on the first imaging.
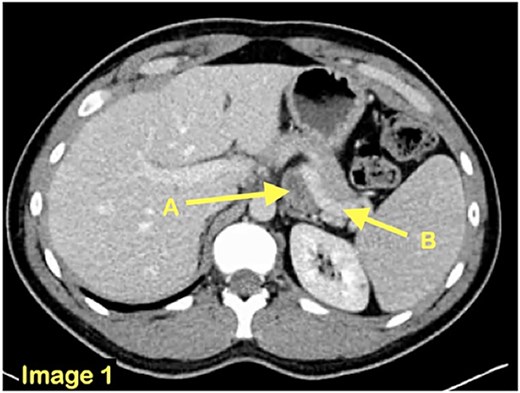
An axial CT scan view revealing the presence of a small bowel loop (A) behind the splenic vein (B).
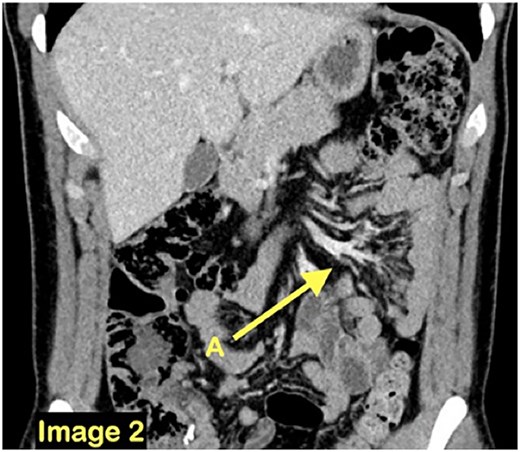
A coronal CT scan view demonstrating a cluster of small bowel loops (A) in the left abdomen.
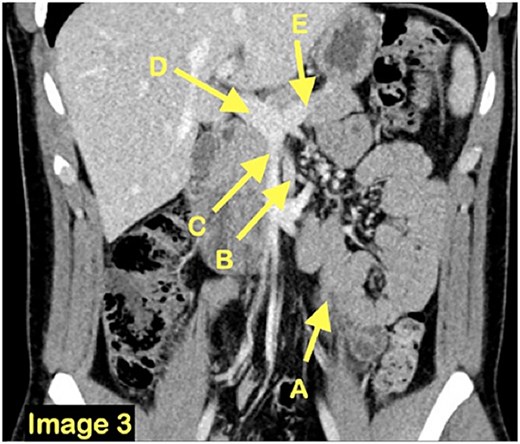
A coronal CT scan view demonstrating once again the clustered small bowel loops (A) and the surrounding vasculature inferior mesenteric vein (B), superior mesenteric vein (C), portal vein (D) and splenic vein (E).
Prompt management was undertaken by the surgical team and the patient underwent a second diagnostic laparoscopy. The hernia was once again reduced (Fig. 4), and a fibrous membrane was identified, seemingly preventing a full reduction of the small bowel loops found in the fossa of Landzert (Fig. 5).
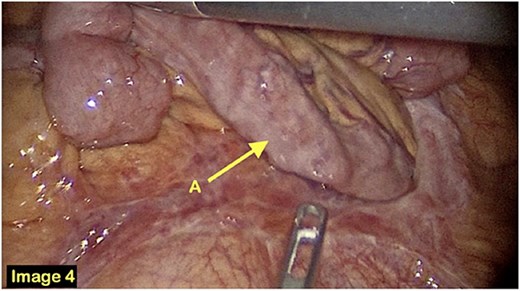
A laparoscopic view of the small bowel protruding through the hernia defect.
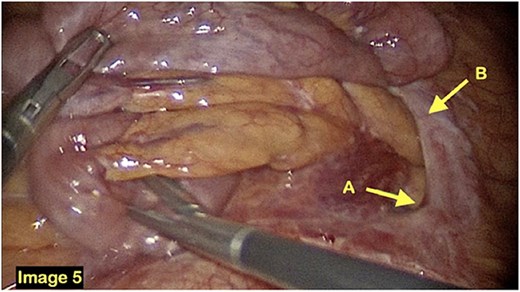
The fossa of Landzert is identified (A) alongside a fibrous band of tissue preventing the small bowel from moving freely through the fossa (B).
This band was transected (Fig. 6), thus widening the orifice, and endoloops used prophylactically on both sides of the band to prevent bleeding. This allowed a full reduction of the hernia (Fig. 7). A conscious decision was made to leave the fossa open and the defect unrepaired, allowing the bowels to move in and out easily from the fossa, while preventing further incarceration and bowel obstruction.
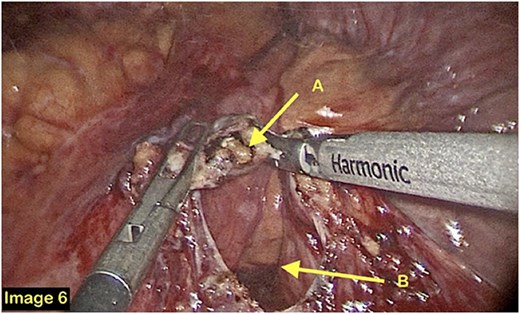
A laparoscopic view of the fibrous band being transected (A) and the fossa of Landzert (B).
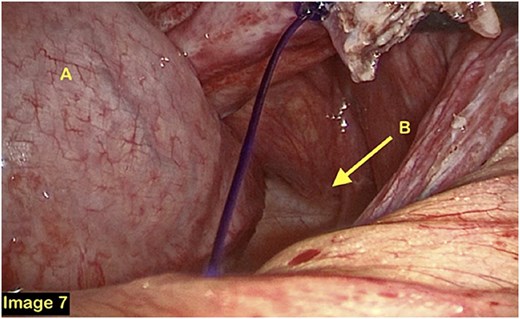
The patient was discharged on the second post-operative day. Latest follow-up was at 21 months post-operatively and no recurrence of symptoms was noted.
Discussion
LPDH are an uncommon cause of small bowel obstruction, where a portion of the small bowel enters a congenital peritoneal defect, the fossa of Landzert, situated behind the descending mesocolon [1–14]. The clinical presentation is notoriously non-specific, some patients being asymptomatic and others presenting with a history of paroxysmal abdominal pain or acute symptoms of obstruction [1–14]. The diagnosis is made difficult by the rarity of this finding [1–10], (some citing a correct pre-operative diagnosis in only 43% of cases [1]), and by the possible spontaneous reduction of the hernia, leading to symptom resolution and a normal CT scan [4, 12, 14]. Nonetheless, a CT scan is the main diagnostic tool, and a cluster of small bowel loops between the stomach and the pancreas, near the ligament of Treitz, and a displacement of normally adjacent structures are suspicious of a LPDH [1–12, 14]. As incarceration and obstruction may occur in ⁓50% of cases [1, 2, 8, 10, 11], special attention should be given to signs of strangulation and ischemia, such as engorged vessels or free fluid [1–12]. Prompt surgical treatment should be attempted to reduce risks of ischemia and death [1–3, 5–14].
As for the surgical procedure, no official guideline exists to this day. Most case studies published to date have attempted a repair of the peritoneal defect, therefore closing the fossa of Landzert altogether [3, 6, 8, 9, 13]. Some discuss the possibility of either closing or opening the defect but opt to close it in most of their reported cases [2, 5], often using a running suture between the jejunum the colon and the mesocolon [5]. This should prevent recurrent herniation of the small bowel in this space, but the risk is not eliminated. While unreported in the literature, herniation through a smaller defect due to technical error or inadequate healing remains a potential concern, as are the risks of strangulation and ischemia. To avoid these risks in our case, the defect was enlarged and left wide open, allowing the small bowel to move freely between the fossa of Landzert and the peritoneal cavity. While the hernia itself is not eliminated, the risks of incarceration and strangulation become very low.
Conclusion
LPDH being a rare but potentially lethal cause of small bowel obstruction, a high level of suspicion should be maintained in cases with a vague history of abdominal pain and no prior abdominal surgeries. It is critical not to delay prompt treatment with laparoscopic exploration, although initial CT scan may at first appear unremarkable. The hernia defect may be either closed primarily or widened to prevent future incarceration.
Conflict of interest statement
None declared.
Funding
None declared.



