-
PDF
- Split View
-
Views
-
Cite
Cite
Katherine L Szeliga, Jenny C McCloskey, Abdallah Elsabagh, Gawri Rajakaruna, Late human immunodeficiency virus presenting as necrotizing anal ulceration due to cytomegalovirus, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf763, https://doi.org/10.1093/jscr/rjaf763
Close - Share Icon Share
Abstract
The morbidity and mortality of severe disease secondary to cytomegalovirus (CMV) infection in immunocompromised patients has been well documented. We report an interesting case of CMV proctitis in a heterosexual adult male in his 50s who initially presented with an 8-month history of rectal pain, intermittent haematochezia, and weight loss. On examination, he was found to have perianal condyloma acuminata and ulceration up to the internal anal sphincter. The clinical suspicion of acquired immunodeficiency, such as human immunodeficiency virus, is of paramount importance in patients with severe, painful anorectal ulceration.
Introduction
The disease course of human immunodeficiency virus (HIV) is variable, with progression from infection to disease often occurring insidiously [1]. If untreated, individuals living with HIV may progress from having no symptoms to a severe, life-threatening disease that represents the late clinical stage of HIV—acquired immunodeficiency syndrome (AIDS). Late-stage HIV is defined as a CD4 count fewer than 200 cells/μl on presentation, or an AIDS-defining event, regardless of CD4 count [2]. Depending on the immunopathology of the disease, clinical presentation of late-stage HIV differs and may manifest across multiple organ systems [1].
We report an unusual case of a late diagnosis of HIV presenting with severe, atypical pain associated with necrotizing anal ulceration, in the presence of high-grade squamous intraepithelial lesions (HSIL) and cytomegalovirus (CMV) proctitis.
Case report
A 51-year-old male was referred to general surgery for further management of large haemorrhoids. The patient reported a progressively worsening 8-month history of severe anorectal pain, pruritis, rectal bleeding, intermittent mucoid discharge, and 15 kg unintentional weight loss. Medical history was remarkable for hypertension and sciatica. Prior to evaluation, history revealed no previous hospitalizations for infection.
At time of assessment, vitals were remarkable for a temperature of 38.2°C and heart rate of 110 beats per minute. Oral examination revealed mucocutaneous leukoplakia, suggestive of candidiasis. On rectal examination there were multiple condyloma acuminata and in the anal verge, there was evidence of ulceration. A fissure was noted at 12 o’clock.
Colonoscopy revealed extensive circumferential superficial ulcerations of the perianal skin (Fig. 1a) as well as a large mucosal ulcer just distal to the dentate line extending from the 3 o’clock position to the 9 o’clock position (Fig. 1b) with internal sphincter on view. Histopathology returned a positive result for HSIL with oncogenic human papilloma virus (HPV) genotypes 16 and 18 detected.
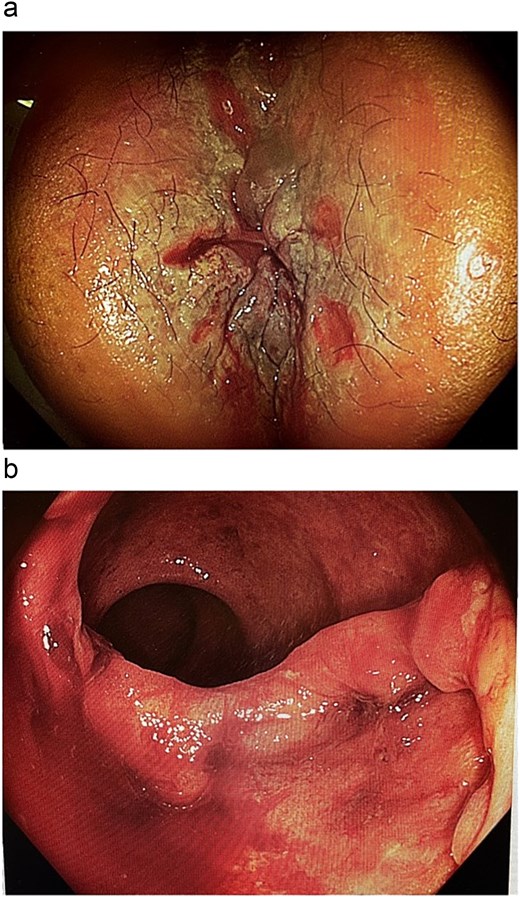
Colonoscopy images. (a) Superficial examination demonstrating circumferential perianal excoriation and ulceration. (b) Extensive colonic mucosal ulceration.
The patient was appropriately referred to a sexual health physician who requested infectious aetiology be investigated given the significance of pain and extent of anal ulceration. Serology returned positive for HSV1 IgG and CMV viral load was 3.62 log10, 4180 IU/ml. HIV antibody returned positive, further confirmed by western blot. A CD4 count <7cells/μl demonstrated severe immunodeficiency. Immunochemistry for CMV and HSV was performed on rectal and perianal lesion biopsies that showed rare cells positive for CMV within endothelial vessels (Fig. 2a–c). There was no evidence of malignancy in any biopsy specimens but viral cytopathic affect and dysplasia consistent with HSIL was confirmed (Fig. 3a and b).
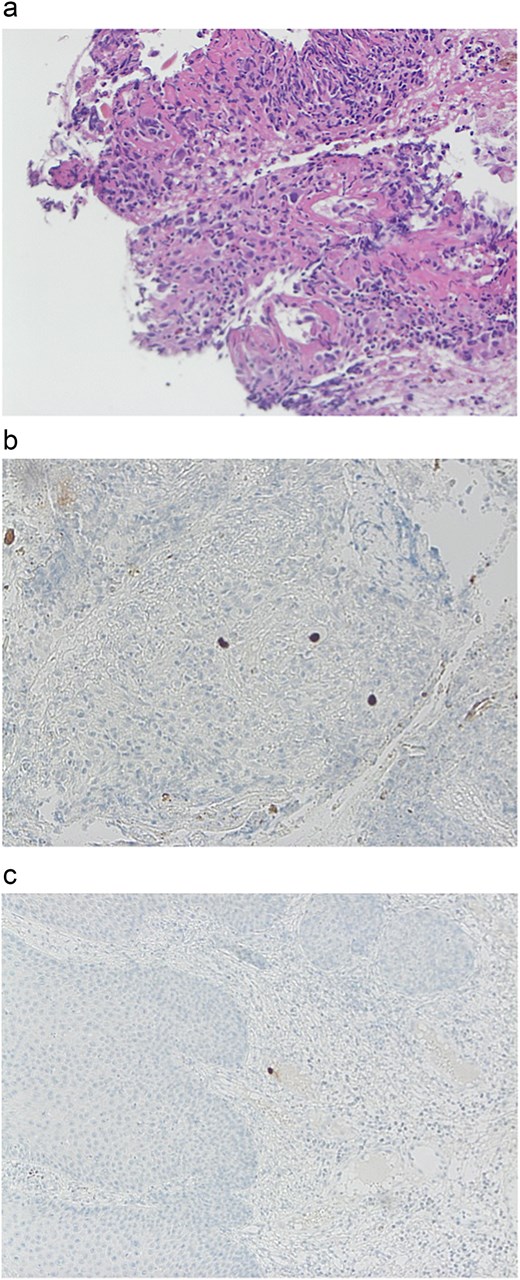
Immunohistochemistry. (a) Rectal biopsy: Large cells suggestive for CMV infection. (b) Rectal biopsy: Immunohistochemistry for CMV 10× high power. (c) Perianal biopsy: Immunohistochemistry for CMV high power.
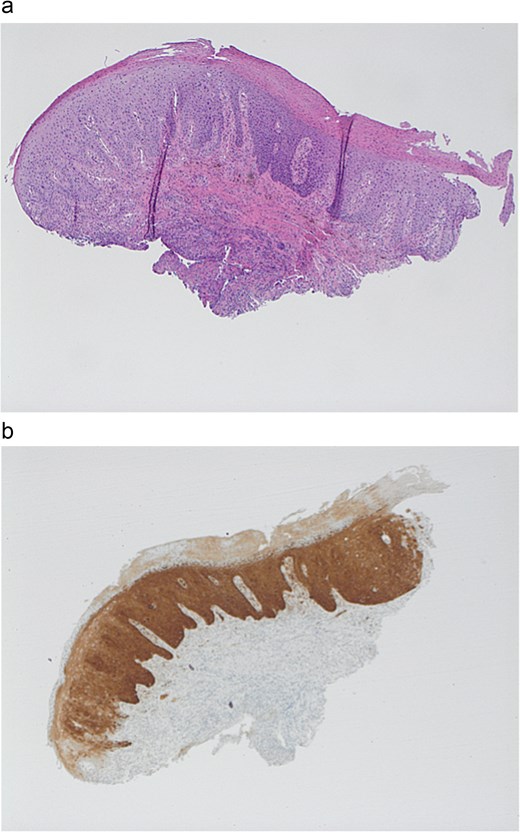
Immunohistochemistry. (a) Perianal biopsy with HISL 4× low power. (b) Perianal biopsy: p16 immunohistochemisty.
Multiplanar T1 and T2 weighted magnetic resonance imaging (MRI) of the rectum showed abnormal signals, mainly mucosal, based at the anal sphincter complex with extension into the inferior rectal mucosa. There was associated induration and ulceration at the level of the sphincter muscle in the 7 o’clock position (Fig. 4a–c).
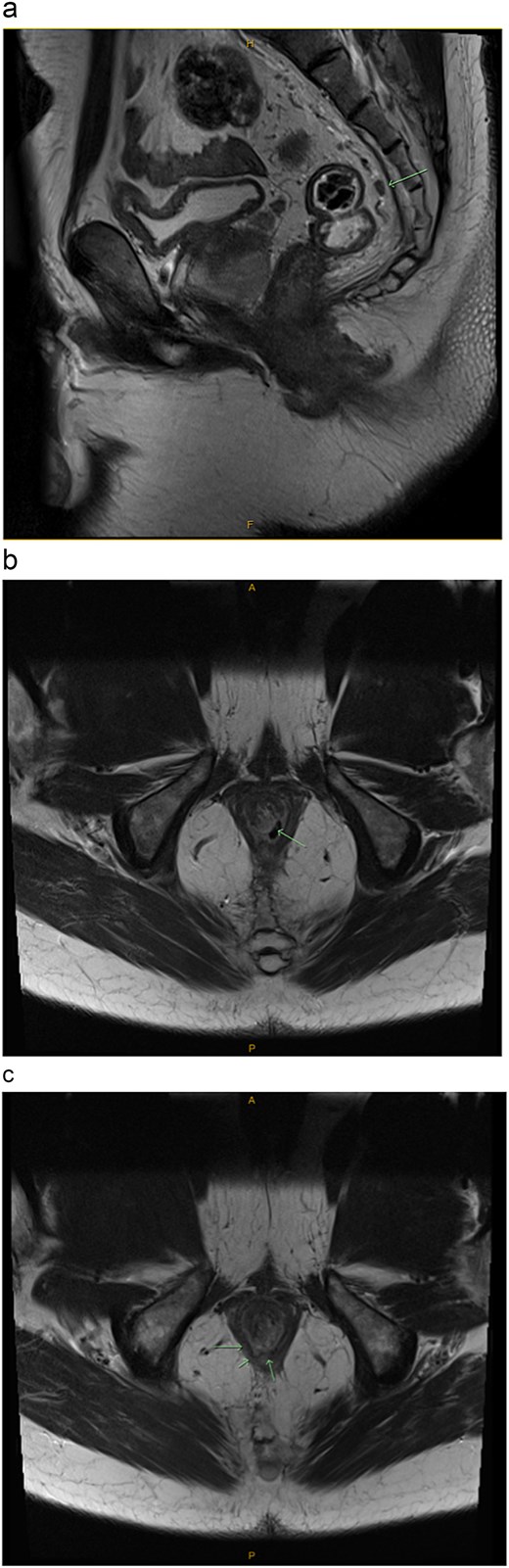
Pelvic MRI with contrast enhancement (T1 and T2 weighted imaging including DWI). (a) Sagittal view: Evidence of a single, small mesorectal lymph node (arrow), but no suspicious mesorectal lymphadenopathy. (b) Transverse view: Evidence of a single, small mesorectal lymph node (arrow), but no suspicious mesorectal lymphadenopathy. (c) Transverse view: Mucosal based high T2 signal involving the anal sphincter complex with focal induration/ulceration noted at the level of the sphincter muscle at 7 o’clock (arrows). Extension into the inferior rectus mucosa.
A diagnosis of CMV proctitis, confirmed by histopathology, HSIL and severe immunodeficiency secondary to previously undiagnosed HIV was made. The patient was referred to a private infectious disease’s physician for further assessment and management.
At the 3-month colorectal follow-up, the patient reported reduced perianal itch, no bleeding per rectum, and regular bowel motions. On examination, perianal ulceration had mostly healed. Once anorectal ulceration has completely resolved the patient will be followed up and reassessed for management of HSIL disease.
Discussion
CMV infection in immunocompetent hosts is commonly assumed to cause undifferentiated mononucleosis-like viral symptoms that are self-limiting; however, a systematic meta-analysis of 290 cases [3] reports that immunocompetent individuals may to experience multi-system clinical manifestations of CMV infection. Among these reports, the most common primary site of involvement was the gastrointestinal tract with 31.4% (n = 91/290) of patients presenting clinically with fever, diffuse abdominal pain, or localizing lower quadrant abdominal pain, nausea and vomiting, anorexia, weight loss, watery or bloody diarrhoea, melaena, and haematochezia [3].
Immunocompromised individuals, particularly those with HIV who have impaired CD4+ T lymphocyte function or low cell number are susceptible to exponential replication of the Herpesviridae virus, leading to viremia and profound multiple organ involvement [4–7]. Gastrointestinal CMV disease in immunocompromised patients is an ulcerative and erosive process that can occur anywhere along the gastrointestinal tract [8]. Cytomegalovirus is an AIDS defining condition [9] and while the diagnosis if often considered in patients with HIV, it is essential that it is not overlooked in patients with even a low degree of immune dysfunction.
HPV is the most common sexually transmitted disease with more than 130 types, 40 of which affect the lower genital tract. HPV is characterized as low risk (predominantly associated with genital warts) or high-risk (classified histologically as low grade (LSIL) and HSIL and invasive cancer). Infection with multiple HPV types carries increased risk of transformation to anal intraepithelial neoplasia (AIN) or HSIL over time [10]. Anogenital manifestations of HPV, such as anogenital warts (condylomata acuminata) and AIN comprise a high burden of disease among immunocompromised HIV-positive patients, but usually the presentation is not of severe pain or ulceration unless there is evidence of neoplasia [11].
Anal condylomata form pink/white cauliflower-like lesions on the perianal skin or within the anal canal to lower rectum. Although condylomatous disease can cause pain, bleeding, and itch, warts are generally considered to be asymptomatic [12]. Similarly, LSIL or HSIL rarely causes deep ulceration or significant pain within the anal canal [11]. If HSIL undergoes malignant transformation into ulcerated in situ carcinoma, approximately one third of patients may experience pain, generally when the sphincter complex is involved [12–14].
Squamous intraepithelial lesions are a rare cause of severe anal pain or anorectal ulceration. Despite what is already known about HPV related lesions, further research is needed to improve screening tools for the identification of HSIL. In addition, education regarding the use of high resolution endoscopy to detect HSIL would be advantageous. This case demonstrates the importance of further investigation into alternative aetiology and pathology in patients with atypical presentations. CMV disease of the gastrointestinal tract characteristically produces mucosal ulceration that can manifest as anorectal pain, diarrhoea, and bleeding. Particularly in patients who are immunocompromised, CMV as a potential infectious agent should be included in the differential diagnosis for severe gastrointestinal disease [15]. It is essential for physicians suspecting CMV or other AIDS-defining conditions to maintain a high index of suspicion for underlying immunocompromise among presumably immunocompetent patients to ensure timely diagnostics, referral, and management.
Conflict of interest statement
None declared.
Funding
None declared.



