-
PDF
- Split View
-
Views
-
Cite
Cite
Mohsin Yahya Murshid, Abdulmalik AlShamrani, Fatimah Hayash, Farrukh Alim Ansari, Left-sided acute appendicitis in a patient with situs inversus totalis: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf653, https://doi.org/10.1093/jscr/rjaf653
Close - Share Icon Share
Abstract
Situs inversus totalis (SIT) is a rare congenital anomaly involving mirror-image reversal of thoracic and abdominal organs, which may complicate the diagnosis and management of acute abdominal conditions due to atypical symptom localization. This report describes a 23-year-old male who presented with lower abdominal pain and vomiting. Clinical examination revealed tenderness in the left iliac fossa and laboratory findings showed leukocytosis. A chest X-ray revealed dextrocardia, raising suspicion for situs inversus totalis, which was confirmed by contrast-enhanced CT demonstrating an inflamed appendix in the left iliac fossa. The patient underwent laparoscopic appendectomy with modifications to port placement and operative positioning to accommodate the reversed anatomy. The procedure was completed without complication, and the patient recovered uneventfully. This case highlights the importance of early recognition of anatomical anomalies in patients with atypical abdominal pain and supports the use of laparoscopy as both a diagnostic and therapeutic approach in SIT.
Introduction
Situs inversus totalis (SIT) is a rare congenital condition characterized by the mirror-image transposition of thoracic and abdominal organs, with an estimated incidence of 1 in 10 000 to 25 000 live births [1]. Although often asymptomatic and discovered incidentally, SIT presents unique diagnostic challenges when patients present with acute abdominal pain. In such scenarios, conventional symptom localization may mislead clinicians and delay appropriate treatment. Acute appendicitis typically presents with right lower quadrant pain, nausea, and anorexia, but in patients with SIT, the inflamed appendix is in the left iliac fossa. This may mimic other conditions such as diverticulitis or gynecologic pathology, potentially complicating clinical evaluation [2, 3]. Moreover, certain SIT patients paradoxically experience right-sided abdominal pain, believed to result from non-mirrored visceral innervation, where afferent pathways follow typical central nervous system (CNS) projections despite reversed anatomy [4].
This case is noteworthy not only for its rarity but also for illustrating the diagnostic ambiguity posed by discordant pain localization, and the operative considerations in adapting laparoscopic technique to reversed anatomy. It underscores the need for heightened clinical suspicion, appropriate imaging, and intraoperative preparedness in patients with known or suspected SIT. Broader awareness of such anatomical variants in emergency settings may facilitate timely diagnosis and reduce the risk of complications in similar presentations.
Case report
A 23-year-old male presented with a 24-hour history of lower abdominal pain that began peri-umbilically and migrated to the left iliac fossa, accompanied by two episodes of non-bilious vomiting. He denied fever, urinary symptoms, bowel changes, or similar prior episodes. He had no comorbidities or surgical history. On examination, he was alert, afebrile, and hemodynamically stable. Abdominal exam revealed left iliac fossa and suprapubic tenderness, with rebound and guarding. Given the atypical location, differential diagnoses included diverticulitis, urinary tract infection, and renal colic, with appendicitis considered less likely.
Laboratory tests showed white blood cell count 13.2 × 109/L; LFTs and renal profile were normal. Inflammatory markers C-reactive protein, erythrocyte sedimentation rate were not requested. A chest X-ray revealed dextrocardia, raising suspicion for SIT. Abdominal X-ray was unremarkable. Contrast-enhanced computed tomography (CT) confirmed SIT with the appendix in the left iliac fossa, measuring 11 mm with mural thickening, intraluminal appendicolith, and peri-appendiceal fat stranding—consistent with early acute appendicitis (Fig. 1).

Coronal (left) and axial (right) CT images of the abdomen demonstrating situs inversus totalis with the liver located on the left side and spleen on the right. The inflamed appendix is seen in the left iliac fossa, with mural thickening and a visible appendicolith (arrow), consistent with acute appendicitis.
The patient underwent laparoscopic appendectomy using a mirror-image three-port configuration (Fig. 2). The monitor was positioned on the left, with the surgical team on the right. Intraoperatively, the inflamed appendix was found in the expected reversed location (Fig. 3). Despite being right-handed, the surgeon encountered only minor ergonomic adjustments, particularly during mesoappendix dissection and ligation, thanks to preoperative planning. The appendix was removed without complication. No other anomalies were noted. The patient recovered uneventfully, resumed oral intake early, and was discharged on postoperative Day 2. At 2 and 4 week follow-ups, he remained symptom-free. Histopathology confirmed acute suppurative appendicitis without perforation or malignancy.
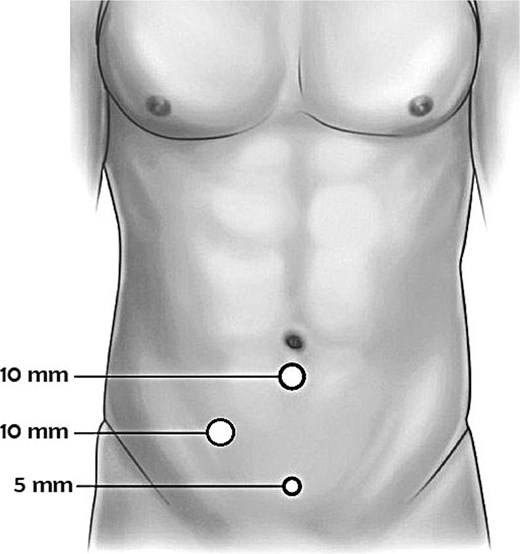
Schematic illustration of mirror-image port placement for laparoscopic appendectomy in a patient with situs inversus totalis. Three ports were used: a 10 mm camera port at the umbilicus, a 10 mm working port in the right lower quadrant (mirror of standard left-sided placement), and a 5 mm assistant port in the supra-pubic area. The operating surgeon and assistant stood on the patient's right side, with the monitor positioned to the left.
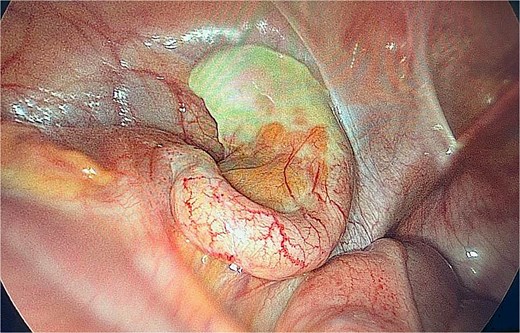
Intraoperative image of inflamed appendix in the left iliac fossa.
Discussion
SIT is a rare congenital condition involving complete mirror-image reversal of thoracic and abdominal organs, typically inherited in an autosomal recessive pattern. Although most individuals remain asymptomatic, the reversed anatomy can complicate clinical assessment, particularly in emergency presentations involving abdominal pain. Additionally, SIT presents distinct intraoperative challenges that may necessitate modifications in standard surgical approaches, particularly in laparoscopic procedures such as cholecystectomy and appendectomy [1–3]. Timely identification of anatomical variations is critical in the evaluation of patients presenting with atypical abdominal pain. In the current case, dextrocardia detected on chest X-ray raised early suspicion of SIT, prompting further imaging and leading to an accurate diagnosis. Cross-sectional imaging, particularly contrast-enhanced CT, remains the most reliable modality for confirming SIT and localizing pathology, especially when clinical findings are non-classical [1].
Standard clinical scoring systems such as the Alvarado score may have limited reliability in SIT, as they are designed around typical symptom patterns involving the right iliac fossa. In SIT, pain may occur in the left iliac fossa or, paradoxically, on the right, due to persistence of standard visceral afferent nerve pathways despite reversed organ placement [2, 3]. This mismatch between organ position and neural mapping can obscure the diagnosis unless clinicians maintain a high index of suspicion. In patients with SIT presenting with left iliac fossa pain, the differential diagnosis is broad and includes conditions such as diverticulitis, urinary tract infection, and, in females, gynecologic disorders. In such cases, the diagnostic workup should include CT to clarify organ orientation and pathology. For women of reproductive age, pelvic ultrasound remains a valuable adjunct to exclude adnexal causes [4, 5].
Laparoscopy offers significant advantages in managing abdominal pathology in SIT due to its capacity for full intra-abdominal visualization and flexible port placement. In this case, a mirrored three-port configuration was employed with the monitor positioned to the left and the surgical team on the right. The operating surgeon, though right-handed, encountered only minor ergonomic adjustments during the procedure. Careful preoperative planning played a key role in ensuring a smooth surgical experience. Previous studies have noted that left-handed surgeons may find it ergonomically more favorable to operate in mirror-image anatomy; however, overall familiarity with reversed orientation and thoughtful intraoperative positioning appear to be more important factors influencing technical ease [6, 7]. In the present case, standard laparoscopic principles were successfully applied with minimal modification.
No additional anomalies were observed intraoperatively. The appendix was readily visualized and removed without complication. Similar outcomes have been reported in other cases of appendicitis in SIT, where tailored laparoscopic techniques have led to favorable clinical courses [8–10]. The growing body of case reports on SIT-associated appendicitis emphasizes the importance of anatomical awareness and surgical adaptability. This case contributes to that literature by reinforcing the role of imaging in diagnosis and the feasibility of laparoscopy when approached with an understanding of mirror-image anatomy [11–15].
Conclusion
This case highlights the diagnostic and operative challenges of managing acute appendicitis in a patient SIT. The patient’s presentation with left iliac fossa pain initially suggested common differentials such as diverticulitis or urinary tract infection. However, early contrast-enhanced CT was crucial in confirming the diagnosis of appendicitis and mapping the reversed anatomy, allowing for prompt and appropriate intervention.
Conflict of interest statement
None declared.
Funding
None declared.



