-
PDF
- Split View
-
Views
-
Cite
Cite
Isra W Ayasa, Rahaf Muhtaseb, Ansam Herbawe, Raneen W Atatrah, Taha Z Makhlouf, Mohammed A Maraqa, Rami D Almarasha, Baker Nairoukh, Laparoscopic resection of an ileocecal duplication cyst in a 7-year-old female: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf506, https://doi.org/10.1093/jscr/rjaf506
Close - Share Icon Share
Abstract
Alimentary tract duplication cysts are rare congenital anomalies that can occur anywhere along the gastrointestinal tract. Ileocecal duplication cysts, a subset of enteric duplication cysts (EDCs), are particularly uncommon and often present with nonspecific symptoms, making preoperative diagnosis difficult. We report a case of a 7-year-old female who presented with intermittent abdominal pain and vomiting for 1 month. Physical examination revealed right iliac fossa tenderness and mild abdominal distension, with imaging suggesting a mesenteric cyst. Laparoscopic exploration identified a mass attached to the ileocecal region, necessitating right hemicolectomy. Histopathology confirmed an ileocecal duplication cyst. Most EDCs are diagnosed within the first two years of life, making this a rare late presentation. This case underscores the importance of considering EDCs in older children with vague abdominal symptoms. Although imaging aids evaluation, surgical exploration remains essential for definitive diagnosis and treatment. Laparoscopic resection effectively prevents complications such as obstruction or perforation.
Introduction
Alimentary tract duplication is a rare congenital anomaly that can occur at any point along the alimentary tract, including enteric duplication cysts (EDCs), which occur in ~1 in 4500 births and have a slight male predominance [1, 2].
These cysts are characterized by an epithelial lining containing the mucosa of the alimentary tract, an envelope of smooth muscle, and a cyst closely attached to the gastrointestinal tract (GT) by sharing a common wall. Although the mucosal lining may not always correspond to the adjacent gastrointestinal tissue, duplications are named based on the part of the GT to which they are closely attached. Ectopic gastric mucosa is found in 20%–30% of these cysts, more frequently in esophageal and small bowel duplications, while ectopic pancreatic mucosa is most commonly observed in gastric duplications [3].
Clinical manifestations vary widely, ranging from asymptomatic cases to severe complications such as intestinal obstruction, bleeding, and perforation [4]. Preoperative diagnosis is often challenging due to nonspecific symptoms and overlapping imaging features with other abdominal pathologies, and most EDCs appear as cystic lesions on CT, with alternating echogenic and hypoechoic layers visible on transabdominal ultrasound [2, 5]. The primary treatment approach for symptomatic EDCs involves complete surgical removal [4].
Case presentation
A 7-year-old female patient with no prior medical history presented with intermittent abdominal pain lasting for ~1 month. The pain had a gradual onset and was localized to the right iliac fossa. Each episode lasted ~2 hours and occurred two to three times per week. It was described as cramping, non-radiating, and of low intensity, typically worsening after meals. The episodes were occasionally associated with vomiting and abdominal distension. There was no associated fever. The patient reported normal bowel habits, with no changes in the frequency, consistency, or appearance of her stools.
On physical examination, she exhibited tenderness in the right iliac fossa with mild to moderate abdominal distension. Baseline laboratory investigations revealed a complete blood count (haemoglobin [Hb] = 12.2 g/dl, white blood cells = 12.5 × 103/μl), and serum electrolytes were within normal range (Na: 141 mmol/L, K: 3.5 mmol/L, Cl: 105 mmol/L).
An abdominal ultrasound revealed a cystic mass in the right iliac fossa. Subsequent computed tomography (CT) confirmed the presence of a right abdominal cyst, with the most likely diagnosis being a mesenteric cyst (Fig. 1).
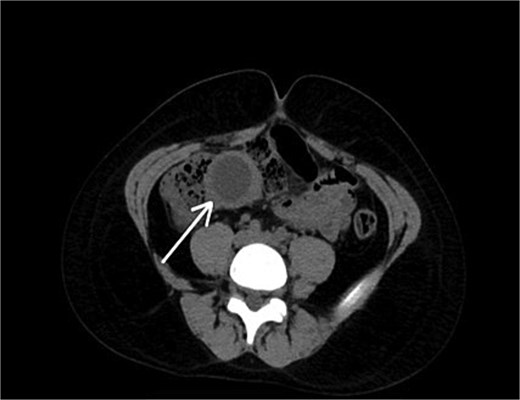
A preoperative axial CT scan of the abdomen and pelvis demonstrates a well-defined, fluid-filled cystic structure adjacent to the bowel.
Given the limitations of imaging in definitively distinguishing among potential diagnoses, including mesenteric cyst, EDC, lymphangioma, and omental cyst, laparoscopic exploration was selected for its minimally invasive nature, diagnostic accuracy, and therapeutic potential. Intraoperatively, a well-localized mass was identified, entirely contained within the cecum, with no involvement of adjacent structures. A duplication cyst was suspected based on its appearance. The mass was firmly attached to the ileocecal region, necessitating a right hemicolectomy, which involved resecting an intestinal segment with peri-intestinal fat, composed of a part of small bowel measuring 9.0 cm in length, a cecum with colon measuring 8.0 cm in length and 4.0 cm in diameter, and an attached appendix measuring 6.0 cm in length and 0.3 cm in diameter. An end-to-end anastomosis was performed without intraoperative complications (Fig. 2).

Histopathological examination revealed a cystic structure at the level of the ileocecal valve measuring 4.0 × 2.5 × 2.5 cm, showing a smooth and thin wall, confirming the diagnosis of an ileocecal duplication cyst. The mucosa of both the small and large bowel, as well as the appendix, appeared unremarkable. Seventeen reactive lymph nodes were identified, with no evidence of malignancy.
Postoperatively, the patient remained nil per os (NPO) for 24 hours, after which clear fluids were introduced and gradually advanced to a normal diet. The patient was discharged in good general condition on postoperative day 3. Upon discharge, she was encouraged to eat small, frequent meals to aid digestion and to maintain adequate hydration to compensate for potential fluid loss. Long-term follow-up includes monitoring for possible nutritional deficiencies, particularly vitamin B12, iron, and folate. Supplementation will be considered if any deficiency is detected. The patient has been followed in the outpatient clinic for 4 months. Follow-up has been uneventful, with the patient remaining in good general condition, reporting no current complaints, and maintaining normal bowel habits.
Discussion
EDCs are rare congenital anomalies that represent a small percentage of abdominal cysts in children [6]. These cysts typically form along the GT, and while they may present as either tubular or cystic structures, the cystic form is more common [7]. The cysts are characterized by muscular layers and a mucosal lining similar to the GT [8]. The first recorded case of an EDC dates back to 1733, though much of the current understanding of these lesions has developed more recently [6]. The exact cause of EDCs remains unclear, but several theories have been proposed, including partial or abortive twinning, the split notochord theory, canalization defects, and potential environmental factors such as trauma or hypoxia [9]. Of these, the split notochord theory is the most widely accepted. EDCs are thought to form during the 4th to 8th weeks of embryonic development, a critical period for GT differentiation [10].
While EDCs can occur anywhere along the GT, from the mouth to the rectum, they are most commonly found in the ileum (33%), followed by the esophagus (20%), colon (13%), jejunum (10%), stomach (7%), and duodenum (5%) [3].
The clinical presentation and severity of symptoms depend largely on the cyst’s size, location, and any complications that may arise. In general, most EDCs present within the first 2 years of life, with ~70% presenting in the first year and 85% by the second year [10]. This case is unique, however, as the patient was 7 years old at the time of presentation. Such an age is uncommon, as the typical diagnosis occurs much earlier in life. This underscores the importance of considering EDCs even in older children, especially when nonspecific symptoms such as intermittent abdominal pain and vomiting are present.
Diagnosing EDCs can be particularly challenging due to the nonspecific nature of their symptoms, which often overlap with those of other abdominal pathologies. In this case, imaging studies initially raised the possibility of a mesenteric cyst, which shares many characteristics with EDCs. However, laparoscopic exploration revealed a mass located at the ileocecal region, confirming the presence of a duplication cyst rather than a mesenteric cyst. This case illustrates how EDCs can sometimes be misdiagnosed based on imaging alone, as their characteristics overlap with other cystic abdominal lesions such as mesenteric cysts, omental cysts, and even meconium pseudocysts. As a result, clinical suspicion and surgical exploration remain crucial for a definitive diagnosis, especially when imaging results are inconclusive.
Laparoscopy has become increasingly valuable in the management of EDCs, especially in pediatric patients. It enables direct visualization for diagnostic confirmation, accurate localization of the lesion, and safe, minimally invasive resection. This is particularly relevant for ileal and ileocecal duplications, where laparoscopic or laparoscopy-assisted excision without bowel resection has been shown to be both feasible and effective in selected cases [11]. In our case, the laparoscopic approach allowed clear identification of the cyst’s anatomical relation to the ileocecal region, facilitated complete excision, and minimized postoperative morbidity. These benefits are consistent with existing literature, which highlights reduced postoperative pain, shorter recovery times, and excellent cosmetic outcomes associated with laparoscopic procedures in children [12]. Thus, laparoscopy not only provides diagnostic clarity in ambiguous cases but also offers a therapeutic advantage, making it a preferred surgical approach when anatomically and technically appropriate.
Complications arising from EDCs include bowel obstruction, intussusception, gastrointestinal bleeding, perforation, and, in rare cases, volvulus or malignancy [3].
In this case, the patient’s symptoms—intermittent abdominal pain and vomiting—were likely caused by local pressure from the cyst, which was located near the ileocecal region. The decision to proceed with laparoscopic resection was made to prevent further complications, such as bowel obstruction, cyst rupture, or peritonitis, all of which can be life-threatening. Surgical resection is the preferred treatment for EDCs, as it alleviates symptoms and reduces the risk of severe complications [9]. Histopathological examination of the resected tissue confirmed the diagnosis of an ileocecal duplication cyst, without evidence of malignancy or ectopic gastric mucosa, which can occasionally be present in these lesions.
Postoperatively, the patient’s recovery was uneventful, and she was discharged in good condition on the third day after surgery. This case emphasizes the importance of considering EDCs in the differential diagnosis of abdominal cystic lesions, even in older children. The typical presentation may be subtler or more atypical than what is commonly seen in infancy. The successful laparoscopic resection and the absence of complications reinforce the value of early diagnosis and appropriate surgical management, ensuring favorable outcomes for children with EDCs.
Conclusion
The study concludes that ileocecal duplication cysts, though uncommon, should be considered in the differential diagnosis of chronic abdominal pain in children. Given the potential for misdiagnosis based on imaging alone, early recognition and surgical intervention are essential to prevent complications. Laparoscopic-assisted resection is a safe and effective treatment, offering favorable outcomes when performed in a timely manner. This case underscores the challenges in diagnosis and highlights the success of laparoscopic-assisted management in treating an ileocecal duplication cyst.
Acknowledgements
The authors express their profound gratitude to the Polytechnic Medical Students’ Research Association (PMRA) for their invaluable contributions and unwavering support that significantly enriched every stage of the research journey.
Author contributions
Concept and design: Isra W. Ayasa, Rahaf Muhtaseb, Ansam Herbawe, Raneen W. Atatrah, and Taha Z. Makhlouf. Drafting of the manuscript: Isra W. Ayasa, Rahaf Muhtaseb, Ansam Herbawe, Raneen W. Atatrah, and Taha Z. Makhlouf. Critical review of the manuscript for important intellectual content: Mohammed A. Maraqa, Rami D. Almarasha, and Taha Z. Makhlouf. Acquisition, analysis, or interpretation of data: Mohammed A. Maraqa, Rami D. Almarasha, and Taha Z. Makhlouf. Supervision: Baker Nairoukh. All authors, Isra W. Ayasa, Rahaf Muhtaseb, Ansam Herbawe, Raneen W. Atatrah, Taha Z. Makhlouf, Mohammed A. Maraqa, Rami D. Almarasha, and Baker Nairoukh, have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Conflict of interest statement
We declare that no conflict of interest could be perceived as prejudicing the impartiality of the research reported.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not for-profit sectors.
Data availability
The data used to support the findings of this study are included in the article.
Informed consent
Written informed consent was obtained from the patient’s family for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal if requested.
Ethical approval
Ethical approval was not applicable for this study, as our institution’s IRB committee at Palestine Polytechnic University does not mandate approval for reporting individual cases or case series.



