-
PDF
- Split View
-
Views
-
Cite
Cite
Jaejun Jeong, Min Kyun Kang, Ji Yeon Kim, Lucky case of pinch-off syndrome combined with colloid adenocarcinoma of the lung, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf503, https://doi.org/10.1093/jscr/rjaf503
Close - Share Icon Share
Abstract
We report a case of a colloid adenocarcinoma in the left lower lobe in a 59-year-old female. The fractured chemoport catheter fragment, which was inserted 10 years ago for gastric cancer chemotherapy, was embedded in left superior segmental pulmonary artery. The patient underwent left lower lobectomy with resection margins and all lymph nodes free of tumor through uniportal video assisted thoracic surgery. The patient was lucky because the malignancy and fractured chemoport catheter fragment could be removed concomitantly without additional lung resection due to the location of catheter fragment. A port access via the internal jugular vein should be considered to prevent pinch-off syndrome and the chemoport catheter needs to be removed as soon as possible after the completion of chemotherpy.
Introduction
The colloid adenocarcinoma is a rare subtype of the lung adenocarcinoma in the World Health Organization (WHO) classification, presenting in just 0.24% of all primary lung carcinomas [1]. A total of 39 cases, which has been followed-up more than 1 year after surgery, have been reported in the literature till now [2]. There is insufficient understanding of the colloid adenocarcinoma because of its paucity. A pinch-off syndrome, a compression of subclavian vein catheter between the clavicle and first rib, which was reported by Hinke et al. [3]. This complication could be life-threatening due to embolization into pulmonary vessels. To date, there has been no report of a case in which colloid adenocarcinoma and pinch-off syndrome were diagnosed to co-exist and were simultaneously removed surgically. This case presents a case of colloid adenocarcinoma with pinch-off syndrome, which was treated by surgical resection concomitantly.
Case report
A 59-year-old female presented to our clinic for evaluation of left lung nodule. She underwent surgery for gastric cancer (Stage IIIA) and chemoport was inserted in the right subclavian vein for adjuvant chemotherapy 10 years ago. A chest computed tomography (CT) scan revealed a 1.8 × 1.5 × 1.5 cm lobulating mass with slightly irregular margins in the superior segment of left lower lobe (LLL) (Fig. 1A and B). A CT-guided percutaneous needle biopsy was performed and colloid adenocarcinoma was diagnosed. At the same time, fractured chemoport fragment, which was embedded in left superior segmental pulmonary artery, was also confirmed (Fig. 1A and B). Fortunately, the catheter fragment did not cause any symptoms such as dyspnea or arrhythmia. An F-18-fluoro-positron emission tomography (FDG-PET) showed no evidence of lymph node involvement or distant metastasis. Surgical resection was planned and LLL resection with mediastinal lymph node dissection was performed through uniportal video assisted thoracic surgery. Histopathological findings were consistent with the diagnosis of colloid adenocarcinoma without visceral pleural invasion, lymphovascular invasion, or regional lymph node metastasis, T1bN0M0 (Fig. 2). The chemoport fragment was also removed clearly (Fig. 1C). After lobectomy was completed, the port chamber with proximal catheter segment was removed. The patient had an uneventful postoperative course and was discharged on postoperative Day 5. He has been free of recurrence for 1-year follow-up.
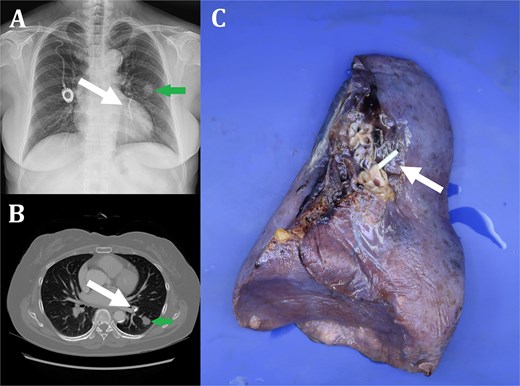
Fractured chemoport fragment embedded in left superior segmental pulmonary artery (white arrow) (A: Chest X-ray, B: Chest CT, C: Specimen of left lower lobe). Colloid adenocarcinoma in superior segment of left lower lobe (green arrow) (A: Chest X-ray, B: Chest CT).
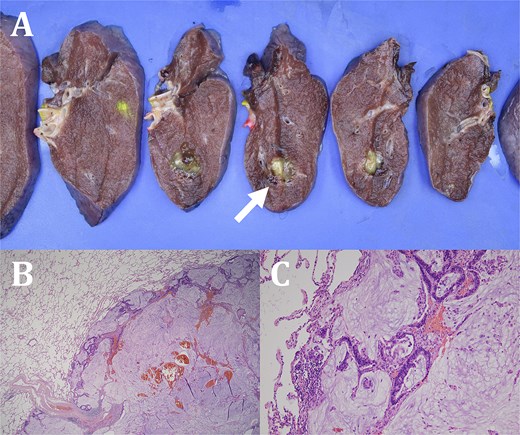
Serial sections of the lung reveal a circumscribed gelatinous tumor (white arrow) (A). The tumor shows prominent extracellular mucin pools with effacement of underlying lung parenchyma (B). The mucin pool is focally surrounded by tumor cells, which are columnar, pseudostratified epithelial cells exhibiting nuclear atypia (hematoxylin and eosin stain, ×100) (C).
Discussion
Colloid adenocarcinoma is classified as a variant of invasive adenocarcinoma. Radiologic findings are insufficient for a definitive diagnosis. A tumor shows poor enhancement on CT and FDG-PET because of the abundant amount of mucus and few malignant cells [4, 5]. The histologic diagnosis is based on the findings of neoplastic cells floating in large pools of mucus and focally lining the alveolar spaces with positive immunostaining for CDX2, MUC2, CK20, and CK7. Surgical resection may be the treatment choice when colloid adenocarcinoma is localized [6]. The pinch off syndrome could be explained by the narrowing of the costoclavicular space. The clinical symptoms might range from asymptomatic to cardiovascular symptoms such as dyspnea, chest pain, and arrhythmia [7]. The diagnosis could be clinched by a simple chest X-ray. A fractured catheter fragment should be extracted promptly because its complications could be disastrous. In this report, we report a lucky case of colloid adenocarcinoma with pinch-off syndrome that was treated concomitantly by LLL resection without any complications. Our report could serve as a reminder that the chemoport catheter needs to be removed as soon as possible after the completion of chemotherpy and a port catheter access through internal jugular vein could be helpful for prevention of pinch-off syndrome.
Conflict of interest statement
No conflicts of interest.
Funding
None declared.
Consent
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Guarantor
The corresponding author will be the guarantor for this paper.



