-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Ho, Christopher B Nahm, Phytobezoar mimicking superior mesenteric artery syndrome in acute duodenal obstruction: a case report and review of literature, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf358, https://doi.org/10.1093/jscr/rjaf358
Close - Share Icon Share
Abstract
Bezoars and superior mesenteric artery (SMA) syndrome are uncommon causes of duodenal obstruction. SMA syndrome is often suspected if radiological features such as reduced aortomesenteric angle and distance are observed. Other pathologies such as an obstructing bezoar should be investigated and treated first before a diagnosis of SMA syndrome is made. In this manuscript, we present a case of an obstructing duodenal bezoar initially misdiagnosed as SMA syndrome, and highlight the importance of thorough upper gastrointestinal endoscopy to the level of the third duodenal segment in all cases of suspected SMA syndrome.
Introduction
Duodenal obstruction is a life-threatening condition, most commonly due to malignant intra-luminal pathologies such as duodenal or periampullary adenocarcinoma. Less commonly, obstruction may arise from superior mesenteric artery (SMA) syndrome, in which the aorta and SMA extrinsically compress the third duodenal segment (D3), particularly in patients with low visceral adipose tissue [1]. Intraluminal bezoars are also an uncommon cause of D3 obstruction, formed by undigested vegetable matter (phytobezoars), hair (trichobezoars), or medications (pharmacobezoars). In this manuscript, we describe a case where thorough endoscopy revealed an obstructing phytobezoar causing duodenal obstruction despite radiological findings of SMA syndrome and review the literature on the coexistence of bezoars and SMA syndrome.
Case report
A 56-year-old male presented to the emergency department with 24 hours of sudden-onset epigastric cramping pain, not improving despite defecating and self-inducing emesis. He reported 15 kg intentional weight loss in the past 12 months with the change to a vegan diet. He had no history of inflammatory bowel disease, malignancy, or previous abdominal surgeries.
On examination, his abdomen was non-distended but tender to palpation in the epigastrium. Laboratory tests demonstrated a mild hypochloremic compensated metabolic alkalosis but no hypokalemia.
Abdominal computed tomography (CT) showed marked dilation of the stomach, first and second duodenal segments, with abrupt collapse at the retroperitoneal junction between the second and third duodenal segments. The aorto-mesenteric angle was reduced at 22° (Fig. 1), and no intraluminal cause of obstruction was visualized. The CT report subsequently concluded the duodenal obstruction was caused by SMA syndrome.

(a) Axial CT demonstrating a grossly distended stomach, first and second duodenal segments with collapse at the third segment between the abdominal aorta and SMA. (b) Sagittal CT with a measured aorto-mesenteric angle of 22°.
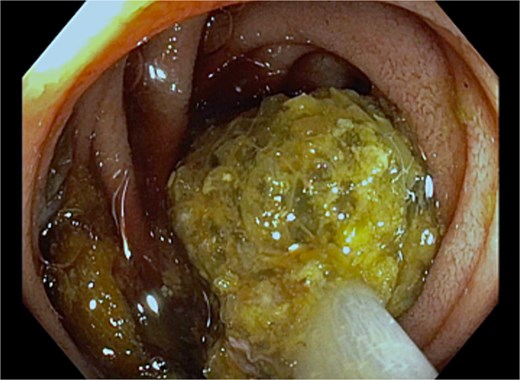
A nasogastric tube was inserted, which drained 2700 ml of green-brown fluid with symptomatic improvement. To assess for alternative causes of duodenal obstruction, upper gastrointestinal endoscopy was performed, which identified a large non-obstructing phytobezoar in the gastric body with associated erosive gastritis (Fig. 2). Upon entering the duodenum, a second phytobezoar causing luminal obstruction was found at the duodenojejunal flexure, which was removed with a Roth net (Fig. 3). Following this, no persistent extrinsic compression of the duodenum was noted endoscopically.
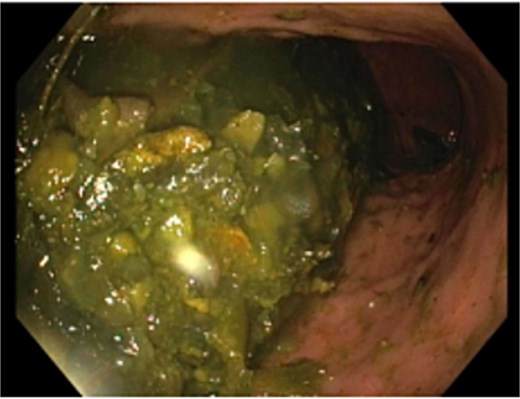
Bezoar material in the gastric body with associated erosive gastritis.
Progress CT showed interval improvement in gastric and small bowel dilatation, but persistent narrowing of the third duodenal segment beneath the SMA (Fig. 4). The patient tolerated reintroduction of oral feeding and was discharged after 2 days with no further nausea or vomiting. He remained well with no recurrence of obstructive symptoms four months later.
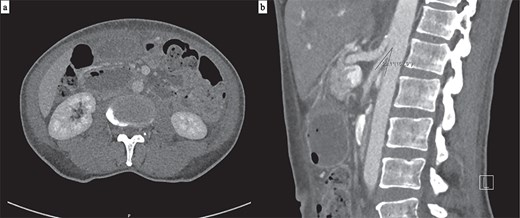
(a) Axial CT showing interval resolution of gastric dilatation with ongoing narrowing of the third duodenal segment between the aorta and SMA. (b) The aorto-mesenteric angle remains reduced at 22° on sagittal CT.
Discussion
SMA syndrome is an uncommon entity, characterized by extrinsic compression of D3 between the abdominal aorta and SMA, leading to duodenal obstruction. Its development is associated with loss of the aortomesenteric fat pad, which normally maintains the aortomesenteric angle between the two vessels at 38°–65° [1]. Rapid weight loss is a risk factor for acquired SMA syndrome, a symptom shared by more common causes of duodenal obstruction, such as malignancy. CT mesenteric angiogram is the most useful imaging modality for the diagnosis of SMA syndrome. Cut-off values for aortomesenteric distance and angle on CT consistent with SMA syndrome are distance <8 mm (100% sensitivity and specificity) and angle <22° (42.8% sensitivity, 100% specificity) [2]. Given the rarity of true SMA syndrome, alternate causes of duodenal obstruction must be excluded prior to surgical management, as bypass surgery can be avoided in many circumstances. The authors advocate for routine upper gastrointestinal endoscopy to the level of D3 in the evaluation of all patients with suspected SMA syndrome.
Bezoars are indigestible conglomerations within the gastrointestinal tract lumen. Phytobezoars are the most common type, consisting of undigested fiber, skin, and seeds of vegetables and fruits. The likelihood of bezoar formation increases with altered gastrointestinal anatomy and motility [3]. While CT is useful in detecting small gastric and intestinal bezoars, endoscopy is the preferred diagnostic modality, as it also allows fragmentation and removal [3]. In this instance, the obstructing phytobezoar was not visualized on CT, highlighting the importance of endoscopy.
In patients without prior gastric surgery or dysmotility, bezoar formation is postulated to develop from changes in dietary habits [4, 5]. In this case, change to vegan diet likely resulted in accumulation of undigested vegetable matter into a bezoar. True SMA syndrome was disproved here by the absence of persistent duodenal narrowing on endoscopy, resolution of the patient’s symptoms following removal of the duodenal bezoar, and absence of further obstructing symptoms.
Summary of 10 case reports describing the coexistence of bezoars and SMA syndrome
| Reference . | Patient . | Bezoar . | Duodenal appearance . | Predisposing factors . | Outcome and follow-up . |
|---|---|---|---|---|---|
| Chung et al. [6] | 44 M | Obstructing phytobezoar at third duodenal segment | Hold up of barium contrast at third duodenal segment on barium swallow study | Vagotomy and pyloroplasty 2 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with no further duodenal narrowing on repeat barium swallow study on 1-year follow-up |
| Doski et al. [7] | 6 F | Trichobezoar extending from duodenal bulb to third segment | Obstruction of the third duodenal segment on barium swallow study | Trichotillomania weight loss | Duodenotomy for removal of bezoar Ladd procedure to relieve duodenal obstruction by SMA Asymptomatic on 3-month follow-up |
| Fuhrman et al. [8] | 46 M | Obstructing bezoar at third duodenal segment | Prominent pulsations extrinsic to duodenal wall | Vagotomy and pyloroplasty 14 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic on 4-month follow-up |
| Lim et al. [9] | 20 F | Gastric bezoars | Intraoperative visualization of the SMA constricting the third duodenal segment Unable to pass gastroscope beyond second duodenal segment | 7 kg weight loss in 6 months prior | Anterior gastrostomy for removal of bezoar Retrocolic duodenojejunostomy for SMA syndrome Asymptomatic on 3-year follow-up |
| Kang et al. [10] | 58 M | Gastric bezoar | Vascular impression of third duodenal segment on duodenography, aortomesenteric distance 8 mm, angle 38.5° on CT | 5 kg weight loss prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with ongoing pulsatile extrinsic compression of duodenum on endoscopy on 6-month follow-up |
| Hernández-Gea et al. [11] | 50 M | Phytobezoar at third duodenal segment | Abrupt vascular compression of third duodenal segment by SMA on CT | Vegetarian diet Weight loss | Endoscopic fragmentation and removal of bezoar Ongoing extrinsic compression on repeat endoscopy noted with no clinical obstruction 5 days later |
| Sato et al. [12] | 71 F | Large mass of undigested food in duodenal lumen | Visualization of SMA narrowing third duodenal segment on autopsy | Patient found dead at home Cause of death: acute gastric dilatation and duodenal obstruction due to intraduodenal bezoar and extrinsic narrowing of third duodenal segment by SMA | |
| Yamagata et al. [13] | 73 M | Obstructing diospyrobezoar at third part of duodenum | Dilatation of the third duodenal segment on stomach on CT No abnormal duodenal findings intraoperatively | Laparoscopic distal gastrectomy with Billroth I reconstruction for gastric cancer 15 months ago | Failed endoscopic fragmentation and removal, proceeded to enterotomy and removal No duodenal abnormalities on endoscopy 4 weeks later |
| Mehdi et al. [14] | 34 F | Phytobezoar in stomach with severe diffuse gastric ulceration | Extrinsic pulsatile compression of third duodenal segment on endoscopy | Acute pancreatitis | Multiple endoscopies to remove bezoar Roux-en-Y gastrojejunostomy with feeding jejunostomy Outcome not discussed |
| Gologorsky et al. [15] | 16 M | Popcorn bezoar impacted at third part of duodenum | Aortomesenteric angle 20.5°, aortomesenteric distance 3.3 mm on CT | Laparotomy, milking of kernels into jejunum and removal with jejunotomy Asymptomatic on 6-month follow-up |
| Reference . | Patient . | Bezoar . | Duodenal appearance . | Predisposing factors . | Outcome and follow-up . |
|---|---|---|---|---|---|
| Chung et al. [6] | 44 M | Obstructing phytobezoar at third duodenal segment | Hold up of barium contrast at third duodenal segment on barium swallow study | Vagotomy and pyloroplasty 2 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with no further duodenal narrowing on repeat barium swallow study on 1-year follow-up |
| Doski et al. [7] | 6 F | Trichobezoar extending from duodenal bulb to third segment | Obstruction of the third duodenal segment on barium swallow study | Trichotillomania weight loss | Duodenotomy for removal of bezoar Ladd procedure to relieve duodenal obstruction by SMA Asymptomatic on 3-month follow-up |
| Fuhrman et al. [8] | 46 M | Obstructing bezoar at third duodenal segment | Prominent pulsations extrinsic to duodenal wall | Vagotomy and pyloroplasty 14 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic on 4-month follow-up |
| Lim et al. [9] | 20 F | Gastric bezoars | Intraoperative visualization of the SMA constricting the third duodenal segment Unable to pass gastroscope beyond second duodenal segment | 7 kg weight loss in 6 months prior | Anterior gastrostomy for removal of bezoar Retrocolic duodenojejunostomy for SMA syndrome Asymptomatic on 3-year follow-up |
| Kang et al. [10] | 58 M | Gastric bezoar | Vascular impression of third duodenal segment on duodenography, aortomesenteric distance 8 mm, angle 38.5° on CT | 5 kg weight loss prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with ongoing pulsatile extrinsic compression of duodenum on endoscopy on 6-month follow-up |
| Hernández-Gea et al. [11] | 50 M | Phytobezoar at third duodenal segment | Abrupt vascular compression of third duodenal segment by SMA on CT | Vegetarian diet Weight loss | Endoscopic fragmentation and removal of bezoar Ongoing extrinsic compression on repeat endoscopy noted with no clinical obstruction 5 days later |
| Sato et al. [12] | 71 F | Large mass of undigested food in duodenal lumen | Visualization of SMA narrowing third duodenal segment on autopsy | Patient found dead at home Cause of death: acute gastric dilatation and duodenal obstruction due to intraduodenal bezoar and extrinsic narrowing of third duodenal segment by SMA | |
| Yamagata et al. [13] | 73 M | Obstructing diospyrobezoar at third part of duodenum | Dilatation of the third duodenal segment on stomach on CT No abnormal duodenal findings intraoperatively | Laparoscopic distal gastrectomy with Billroth I reconstruction for gastric cancer 15 months ago | Failed endoscopic fragmentation and removal, proceeded to enterotomy and removal No duodenal abnormalities on endoscopy 4 weeks later |
| Mehdi et al. [14] | 34 F | Phytobezoar in stomach with severe diffuse gastric ulceration | Extrinsic pulsatile compression of third duodenal segment on endoscopy | Acute pancreatitis | Multiple endoscopies to remove bezoar Roux-en-Y gastrojejunostomy with feeding jejunostomy Outcome not discussed |
| Gologorsky et al. [15] | 16 M | Popcorn bezoar impacted at third part of duodenum | Aortomesenteric angle 20.5°, aortomesenteric distance 3.3 mm on CT | Laparotomy, milking of kernels into jejunum and removal with jejunotomy Asymptomatic on 6-month follow-up |
Summary of 10 case reports describing the coexistence of bezoars and SMA syndrome
| Reference . | Patient . | Bezoar . | Duodenal appearance . | Predisposing factors . | Outcome and follow-up . |
|---|---|---|---|---|---|
| Chung et al. [6] | 44 M | Obstructing phytobezoar at third duodenal segment | Hold up of barium contrast at third duodenal segment on barium swallow study | Vagotomy and pyloroplasty 2 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with no further duodenal narrowing on repeat barium swallow study on 1-year follow-up |
| Doski et al. [7] | 6 F | Trichobezoar extending from duodenal bulb to third segment | Obstruction of the third duodenal segment on barium swallow study | Trichotillomania weight loss | Duodenotomy for removal of bezoar Ladd procedure to relieve duodenal obstruction by SMA Asymptomatic on 3-month follow-up |
| Fuhrman et al. [8] | 46 M | Obstructing bezoar at third duodenal segment | Prominent pulsations extrinsic to duodenal wall | Vagotomy and pyloroplasty 14 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic on 4-month follow-up |
| Lim et al. [9] | 20 F | Gastric bezoars | Intraoperative visualization of the SMA constricting the third duodenal segment Unable to pass gastroscope beyond second duodenal segment | 7 kg weight loss in 6 months prior | Anterior gastrostomy for removal of bezoar Retrocolic duodenojejunostomy for SMA syndrome Asymptomatic on 3-year follow-up |
| Kang et al. [10] | 58 M | Gastric bezoar | Vascular impression of third duodenal segment on duodenography, aortomesenteric distance 8 mm, angle 38.5° on CT | 5 kg weight loss prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with ongoing pulsatile extrinsic compression of duodenum on endoscopy on 6-month follow-up |
| Hernández-Gea et al. [11] | 50 M | Phytobezoar at third duodenal segment | Abrupt vascular compression of third duodenal segment by SMA on CT | Vegetarian diet Weight loss | Endoscopic fragmentation and removal of bezoar Ongoing extrinsic compression on repeat endoscopy noted with no clinical obstruction 5 days later |
| Sato et al. [12] | 71 F | Large mass of undigested food in duodenal lumen | Visualization of SMA narrowing third duodenal segment on autopsy | Patient found dead at home Cause of death: acute gastric dilatation and duodenal obstruction due to intraduodenal bezoar and extrinsic narrowing of third duodenal segment by SMA | |
| Yamagata et al. [13] | 73 M | Obstructing diospyrobezoar at third part of duodenum | Dilatation of the third duodenal segment on stomach on CT No abnormal duodenal findings intraoperatively | Laparoscopic distal gastrectomy with Billroth I reconstruction for gastric cancer 15 months ago | Failed endoscopic fragmentation and removal, proceeded to enterotomy and removal No duodenal abnormalities on endoscopy 4 weeks later |
| Mehdi et al. [14] | 34 F | Phytobezoar in stomach with severe diffuse gastric ulceration | Extrinsic pulsatile compression of third duodenal segment on endoscopy | Acute pancreatitis | Multiple endoscopies to remove bezoar Roux-en-Y gastrojejunostomy with feeding jejunostomy Outcome not discussed |
| Gologorsky et al. [15] | 16 M | Popcorn bezoar impacted at third part of duodenum | Aortomesenteric angle 20.5°, aortomesenteric distance 3.3 mm on CT | Laparotomy, milking of kernels into jejunum and removal with jejunotomy Asymptomatic on 6-month follow-up |
| Reference . | Patient . | Bezoar . | Duodenal appearance . | Predisposing factors . | Outcome and follow-up . |
|---|---|---|---|---|---|
| Chung et al. [6] | 44 M | Obstructing phytobezoar at third duodenal segment | Hold up of barium contrast at third duodenal segment on barium swallow study | Vagotomy and pyloroplasty 2 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with no further duodenal narrowing on repeat barium swallow study on 1-year follow-up |
| Doski et al. [7] | 6 F | Trichobezoar extending from duodenal bulb to third segment | Obstruction of the third duodenal segment on barium swallow study | Trichotillomania weight loss | Duodenotomy for removal of bezoar Ladd procedure to relieve duodenal obstruction by SMA Asymptomatic on 3-month follow-up |
| Fuhrman et al. [8] | 46 M | Obstructing bezoar at third duodenal segment | Prominent pulsations extrinsic to duodenal wall | Vagotomy and pyloroplasty 14 years prior | Endoscopic fragmentation and removal of bezoar Asymptomatic on 4-month follow-up |
| Lim et al. [9] | 20 F | Gastric bezoars | Intraoperative visualization of the SMA constricting the third duodenal segment Unable to pass gastroscope beyond second duodenal segment | 7 kg weight loss in 6 months prior | Anterior gastrostomy for removal of bezoar Retrocolic duodenojejunostomy for SMA syndrome Asymptomatic on 3-year follow-up |
| Kang et al. [10] | 58 M | Gastric bezoar | Vascular impression of third duodenal segment on duodenography, aortomesenteric distance 8 mm, angle 38.5° on CT | 5 kg weight loss prior | Endoscopic fragmentation and removal of bezoar Asymptomatic with ongoing pulsatile extrinsic compression of duodenum on endoscopy on 6-month follow-up |
| Hernández-Gea et al. [11] | 50 M | Phytobezoar at third duodenal segment | Abrupt vascular compression of third duodenal segment by SMA on CT | Vegetarian diet Weight loss | Endoscopic fragmentation and removal of bezoar Ongoing extrinsic compression on repeat endoscopy noted with no clinical obstruction 5 days later |
| Sato et al. [12] | 71 F | Large mass of undigested food in duodenal lumen | Visualization of SMA narrowing third duodenal segment on autopsy | Patient found dead at home Cause of death: acute gastric dilatation and duodenal obstruction due to intraduodenal bezoar and extrinsic narrowing of third duodenal segment by SMA | |
| Yamagata et al. [13] | 73 M | Obstructing diospyrobezoar at third part of duodenum | Dilatation of the third duodenal segment on stomach on CT No abnormal duodenal findings intraoperatively | Laparoscopic distal gastrectomy with Billroth I reconstruction for gastric cancer 15 months ago | Failed endoscopic fragmentation and removal, proceeded to enterotomy and removal No duodenal abnormalities on endoscopy 4 weeks later |
| Mehdi et al. [14] | 34 F | Phytobezoar in stomach with severe diffuse gastric ulceration | Extrinsic pulsatile compression of third duodenal segment on endoscopy | Acute pancreatitis | Multiple endoscopies to remove bezoar Roux-en-Y gastrojejunostomy with feeding jejunostomy Outcome not discussed |
| Gologorsky et al. [15] | 16 M | Popcorn bezoar impacted at third part of duodenum | Aortomesenteric angle 20.5°, aortomesenteric distance 3.3 mm on CT | Laparotomy, milking of kernels into jejunum and removal with jejunotomy Asymptomatic on 6-month follow-up |
A literature search identified 10 case reports where bezoars were found in patients described to have features of SMA syndrome (see Table 1). In seven patients, predisposing factors such as previous gastric surgery and rapid weight loss were identified [6–11, 13]. In seven patients, obstructing bezoars were found at D3 [6–8, 11–13, 15] and gastric bezoars were seen in the remaining three patients [9, 10, 14]. We hypothesize that some patients have a sub-clinical level of extrinsic D3 compression by the SMA, predisposing them to the development of fulminant duodenal obstruction by a bezoar that would otherwise have passed through in patients with normal anatomy. In two patients, persistent extrinsic pulsatile compression was noted endoscopically on follow-up with no symptomatic obstruction, supporting this hypothesis [10, 11]. Importantly, bezoars were removed by endoscopic fragmentation or with enterotomy in nine patients [6–11, 13–15]. Of these nine patients, six patients required no further surgical bypass following bezoar removal [6, 8, 10, 11, 13, 15]. Two patients underwent bypass surgery (retrocolic duodenojejunostomy, Roux-en-Y gastrojejunostomy with feeding jejunostomy) [9, 14] and one underwent a Ladd procedure for definitive management of SMA syndrome [7]. Eight patients were asymptomatic on follow up ranging from 5 days to 1 year later [6–11, 13, 15]. The outcome was undescribed for one patient [14], and for another patient diagnosis was made on autopsy [12].
Conclusion
Clinicians should be cognisant of the existence of obstructing bezoars in patients with acute duodenal obstruction who have radiological features suggestive of SMA syndrome. A preceding history of rapid weight loss and major diet change should increase suspicion for bezoar formation. Thorough upper gastrointestinal endoscopy through the entire duodenum should be performed to assess for intraluminal pathology, as the most likely site for an impacted bezoar would be in the narrowed third duodenal segment. A review of the literature indicates removal of the bezoar often cures duodenal obstruction even when radiological features of SMA syndrome are present.
Author contributions
DH obtained patient information and wrote the manuscript. CN provided administrative and editorial input for the manuscript.
Conflict of interest statement
The authors report no conflict of interest.
Funding
No funding was received for this study.
Consent
The patient provided informed consent for his details to be included in this case report.



