-
PDF
- Split View
-
Views
-
Cite
Cite
Mohsin Yahya Murshid, Mohammed Ghandourah, Abdulmalik AlShamrani, Saeed Ahmed AlZahrani, Infected urachal cyst presenting as acute abdomen – a case report, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf359, https://doi.org/10.1093/jscr/rjaf359
Close - Share Icon Share
Abstract
Urachal cysts are rare congenital anomalies arising from incomplete obliteration of the urachus, an embryological connection between the bladder and umbilicus. This report describes a 33-year-old man who presented with acute abdominal pain, constipation, and umbilical discharge. Diagnostic imaging, particularly computed tomography scans, revealed a thick-walled, fluid-filled cystic lesion adjacent to the umbilicus, indicative of an infected urachal cyst without evidence of bowel involvement. Diagnosing urachal anomalies in adults remains challenging due to their rarity and nonspecific clinical presentation, emphasizing the importance of imaging for accurate identification and targeted surgical intervention. The patient underwent successful surgical excision with drainage of the associated umbilical sinus and abscess, achieving satisfactory postoperative recovery. This case highlights the necessity of clinician awareness and prompt management of urachal cysts to prevent serious complications, such as persistent infection, abscess formation, or malignant transformation.
Introduction
Urachal anomalies are rare congenital disorders resulting from the incomplete obliteration of the urachus, a vestigial tract connecting the fetal bladder to the allantois [1]. Normally degenerating post-birth into the medial umbilical ligament, these conditions can lead to significant clinical complications, such as infections or malignant transformations, particularly when diagnosis is delayed into adulthood. Urachal anomalies are rare in adults and often present with non-specific symptoms like abdominal pain, which are challenging to diagnose in emergency settings where they might be overlooked [1, 2]. Urachal cysts, a specific type of urachal anomaly, arise from the disruption of the urachal remnant and are typically identified in children, though they can also occur in adults. The incidence is about 1 in 5000 live births, with ~35% of cases presenting symptoms such as lower abdominal pain, urinary tract infections, or palpable masses. These cysts are usually diagnosed incidentally during imaging for unrelated symptoms or when they present with acute abdominal issues [3, 4]. Diagnostic tools include ultrasound, cystography, and computed tomography (CT). This case report focuses on an adult male with acute abdominal pain due to an infected urachal cyst, highlighting the importance of considering such rare diagnoses.
Case report
A 33-year-old male patient with no significant medical and surgical history presented to the emergency room with complaints of abdominal pain, distension, and a 6-month history of watery, foul-smelling discharge from the umbilicus, associated with absolute constipation for 5 days. He also reported a burning sensation during urination without any change in urine color. There was associated fever, nausea, or vomiting. His appetite was diminished. Physical examination revealed the abdomen was soft and lax with mild distension and localized tenderness in the sub-umbilical area.
Lab tests showed an elevated white blood cell count of 14 000/mm3. A CT scan of the abdomen was requested, which scan revealed a dilated cecum filled with fecal matter, mildly dilated small bowel loops, and a fluid-filled, thick-walled cystic lesion measuring approximately 3.6 × 3 × 4.6 cm at the level of the umbilicus (Fig. 1a). The lesion, which contained a few tiny air locules and appeared to communicate with the umbilicus, did not show a clear connection to underlying bowel loops. A retrograde cystourethrogram was performed, showing an intact urinary bladder wall with no communication with the cystic lesion (Fig. 1b). The urinary bladder was mildly thickened, and no other significant abnormalities were noted in the abdominal and pelvic organs.
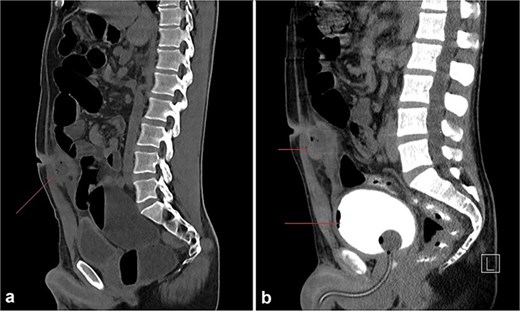
(a) A round to oval shaped, thick walled, fluid filled cystic lesion (34 HU) measuring ~3.6 × 3 × 4.6 cm is noted at the level of the umbilicus, subjacent to the rectus abdominus muscles; it appears to be in communication with the umbilicus. Few tiny air locules are noted within. (b) Retrograde cystourethrogram showing an intact urinary bladder with mild diffuse thickening of the wall. No communication can be seen between the abscess cavity and the bladder.
The patient underwent surgery for excision and drainage of the cystic lesion. An infraumbilical incision revealed a sinus connected to underlying layers with intact fascia. A large cavity containing gray material with a foul smell was identified and excised, followed by irrigation and packing. The patient tolerated the procedure well and was discharged on postoperative day 2 in stable condition. Patient recovery was satisfactory on subsequent out-patient clinic visits.
Discussion
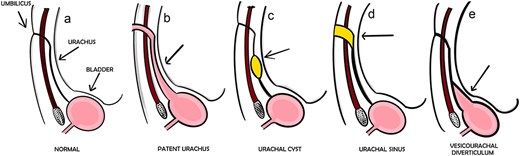
Urachal anomalies are rare congenital conditions resulting from incomplete obliteration of the embryonic connection between the bladder and umbilicus. Four main types are recognized: patent urachus, urachal cyst, urachal sinus, and vesicourachal diverticulum (Fig. 2) [5, 6]. Urachal cysts are the most common type, followed by urachal sinus and patent urachus [5]. The most frequent presenting symptom is umbilical discharge, followed by abdominal pain and mass [5, 6]. Ultrasonography (US) is the preferred initial diagnostic tool, with high accuracy for all anomaly types [6]. Surgical excision is the standard treatment, sometimes requiring partial cystectomy [5]. Early diagnosis and management are crucial to prevent complications such as infections and malignancies [6].
Urachal anomalies can present with various clinical manifestations and imaging features [7, 8]. CT and US are primary imaging modalities, with CT typically showing midline masses extending from the umbilicus to the bladder dome [7, 8]. Magnetic resonance imaging (MRI) provides additional information, particularly for assessing associated spinal cord abnormalities [9]. While symptomatic cases may require surgical intervention, asymptomatic lesions can often be managed conservatively with imaging surveillance [10]. Distinguishing between infected urachal cysts and urachal carcinomas based solely on imaging remains challenging, necessitating further diagnostic procedures [8].
Recent studies suggest a shift toward conservative management of urachal anomalies in children, especially for asymptomatic or minimally symptomatic cases. Initial conservative approaches, including watchful waiting and antibiotic use, have shown promising results [11]. Infected urachal cysts may present with abdominal pain, fever, nausea, and urinary complications. Conservative management is often recommended for newborns due to the possibility of spontaneous involution. For adults, surgical resection of the urachal remnant up to the bladder dome is advised to prevent recurrence and reduce the risk of malignant transformation. Most tumors associated with the urachus manifest as adenocarcinomas at the bladder apex [12]. Management approaches vary depending on the size and complexity of the lesion. Small abscesses (<1.2 cm) may be treated with antibiotics or drainage, while larger ones often require surgical excision [13]. A two-stage approach involving initial drainage followed by complete excision is recommended for complicated cases [14, 15]. However, some cases may be managed with a single-stage approach using preoperative antibiotics and definitive excision. Surgical excision is generally recommended in adults to prevent recurrent infections and potential malignant transformation [14].
Conclusion
This case highlights the clinical importance of considering urachal anomalies, such as infected urachal cysts, in the differential diagnosis of acute abdominal pain in adults. Early recognition, accurate imaging, and timely surgical management are essential to minimize complications, including infection recurrence and malignancy risk. Further awareness and research into standardized diagnostic and management protocols will aid clinicians in effectively addressing these rare congenital conditions.
Conflict of interest statement
None declared.
Funding
None declared.



