-
PDF
- Split View
-
Views
-
Cite
Cite
Yangjun Gu, Zhitao Chen, Qingqing Fang, Qiyong Li, Endoscopic-assisted duodenal decompression tube placement during the operation ensures and accelerates the recovery of duodenal trauma: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf925, https://doi.org/10.1093/jscr/rjaf925
Close - Share Icon Share
Abstract
We present the case of a 42-year-old man who sustained a traumatic perforation of the horizontal (third) portion of the duodenum. The injury was diagnosed within 24 hours of the trauma. During the operative repair, intraoperative endoscopy was used to guide placement of a duodenal decompression tube to optimize postoperative drainage. Two weeks later, endoscopic re-evaluation confirmed complete healing, and the patient was discharged in good condition. Finally, we review current strategies for managing traumatic duodenal injuries, with special emphasis on the role of endoscopic techniques.
Introduction
Traumatic duodenal injuries (TDIs) account for only 3.7%–5% of all abdominal trauma, but associated with substantial morbidity and mortality [1]. According to causes, TDI could be divided into penetrating (77%) and blunt (23%) trauma, the latter most frequently resulting from motor-vehicle collisions (85%). These injuries predominantly affect young male patients, with reported mortality rates ranging from 5% to 30%, depending on the injury grade and time to diagnosis [1, 2]. The American Association for the Surgery of Trauma, in agreement with the Organ Injury Scale Committee (AAST-OIS), categorizes TDIs into five grades, aiming to estimate mortality. Key predictors of outcome include time to diagnosis, presence of associated injury, need for transfusion, physiologic derangement, and injury severity score on arrival. A diagnostic delay exceeding 24 hours increases mortality fourfold (from 11% to 40%) and is associated with a 5-fold rise in mortality following blunt trauma [3].
Case report
At approximately midnight on a rainy night, a 42-year-old man presented to our emergency department around half an hour after falling from his electric bicycle on a slippery road. The handlebars struck his left lower chest and left upper quadrant, and he complained of persistent pain in the left upper abdomen. On examination, there were small contusions over the left costal margin, marked tenderness in the left upper quadrant with mild rebound, and no signs of hemodynamic instability. Initial laboratory studies revealed a mild anemia (hemoglobin 11.6 g/dl), and contrast-enhanced computed tomography (CT) demonstrated multiple left-sided rib fractures, slight peripancreatic fluid collection, and subtle edema of the proximal jejunum (Fig. 1a). The patient was admitted for observation by the surgical team. Eight hours later, repeat contrast CT revealed extraluminal air and contrast leakage at the junction of the ascending duodenum and proximal jejunum, consistent with perforation (Fig. 1b), and he was taken for emergent laparotomy. Intraoperatively, injuries to the stomach, transverse colon, ascending duodenum, and proximal jejunum were confirmed (Fig. 1c).
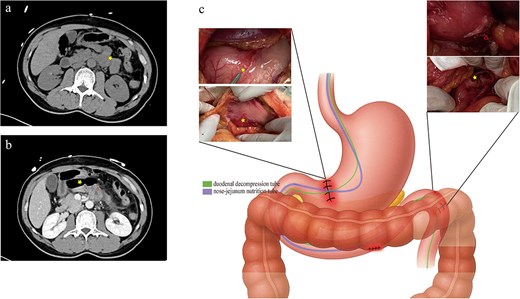
(a) Initial non–contrast abdominal CT on presentation demonstrating slight peripancreatic fluid collection, mild wall thickening, and edema of the proximal jejunum (yellow star). (b) Contrast-enhanced CT performed 8 hours later, showing extraluminal air (yellow star) and contrast leakage (red triangle) at the junction of the ascending duodenum and proximal jejunum. (c) Intraoperative view showing serosal lacerations of the stomach and transverse colon, with perforations of the ascending duodenum and proximal jejunum (yellow star denotes the main defect; red triangle indicates a smaller perforation identified endoscopically), and the positions of the duodenal decompression tube (purple) and nasojejunal feeding tube (green).
Serosal repair was performed on the stomach and transverse colon, and the duodenal and jejunal perforations were closed primarily. Intraoperative endoscopy facilitated placement of a nasojejunal feeding tube and a duodenal decompression tube. The feeding tube tip was positioned 20 cm distal to the repair site, while the decompression tube tip was advanced to the horizontal portion of the duodenum (Fig. 1c). The patient resumed oral intake 1 week postoperatively. A follow-up endoscopic examination prior to discharge confirmed complete mucosal healing (Fig. 2).
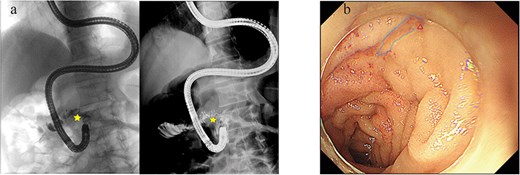
(a) Contrast radiograph of the ascending duodenum and proximal jejunum demonstrating luminal continuity without perforation. (b) Follow-up enteroscope illustrating localized mucosal scarring at the site of duodenal perforation repair.
Discussion
Although rare, duodenal trauma is associated with significant morbidity and mortality, outcomes that are largely determined by injury severity, concurrent injuries, and promptness of intervention. When technically feasible, primary repair supplemented by adequate drainage and early enteral nutrition offers the most favorable prognosis; more complex reconstructive procedures are reserved for cases with extensive tissue loss or failed primary repair. Though studies demonstrate that there was no difference in mortality based on causes of injury [4], blunt duodenal trauma is more frequently complicated by intra-abdominal injuries that may be overlooked at initial surgery.
According to the AAST-OIS, this patient’s duodenal laceration involved nearly 50% of the circumference, classifying it as a grade II injury with an associated mortality of ~18.7%. Duodenal contents contain active pancreatic enzymes capable of causing extensive tissue autodigestion when leaked. Postoperative morbidity and mortality are often driven by enzyme-mediated corrosion. Consequently, generous drainage of the repair site is essential. Compared with external drains, intraluminal decompression tubes can be removed earlier, are easier to manage, and carry a lower risk of drain-related complications. Early nutrition, especially intestinal support, was an important security of enhanced recovery. Intestinal nutrition tube was commonly recommended for gastrointestinal surgery, especially for those with undesirable healing factors.
Endoscopy has been confirmed to play an important role in upper gastrointestinal perforations, especially for small perforations [5]. Intraoperative endoscopic visualization enables accurate identification of subtle perforations and areas of gastrointestinal wall fragility that might otherwise be overlooked. Furthermore, blind placement of enteral tubes during open surgery can be technically challenging; endoscopic guidance allows precise intraoperative positioning of nasojejunal feeding and duodenal decompression tubes, thereby avoiding a separate postoperative endoscopic procedure, minimizing patient discomfort, and facilitating accelerated recovery.
Conclusion
We presented a case of traumatic duodenal perforation managed with intraoperative gastroscopic guidance for placement of nasojejunal feeding and duodenal decompression tubes. The patient’s uncomplicated, rapid recovery highlights that intraoperative endoscopic assistance can minimize surgical trauma and optimize postoperative outcomes in complex upper gastrointestinal injuries.
Author contributions
Gu Yangjun wrote the paper; Chen Zhitao, Fang Qingqing, and Li Qiyong performed the edit and review.
Conflict of interest statement
None declared.
Funding
None declared.



