-
PDF
- Split View
-
Views
-
Cite
Cite
Ranya Abo Khalaf, Mostafa Ibraheem, Hanin Shatrit, Moayad Nammourah, Orwa Alfallah, Qais Alnjoom, The quiet cyst: incidental diagnosis and conservative management of the first documented gallbladder ciliated foregut cyst in Palestine: a case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf899, https://doi.org/10.1093/jscr/rjaf899
Close - Share Icon Share
Abstract
Ciliated foregut cysts (CFCs) are rare congenital lesions derived from primitive foregut remnants, typically occurring above the diaphragm; involvement of the gallbladder is extremely uncommon, with only 17 cases reported previously. We present the 18th known case, and the first documented in Palestine, of gallbladder CFC in a 34-year-old female (G5 P4A1) who presented with sudden-onset left flank pain. Imaging revealed mild hydroureteronephrosis due to distal ureteric stones and incidentally identified a well-defined 7 mm cystic structure within the gallbladder fundus on computed tomography, confirmed by ultrasound. The patient had no biliary symptoms, and all other abdominal findings were normal. She was managed conservatively and discharged with outpatient surveillance. Although exceedingly rare, gallbladder CFCs should be considered in the differential diagnosis of incidental gallbladder cystic lesions. Recognition of their imaging features and embryologic origin is essential for accurate diagnosis and appropriate management.
Introduction
Ciliated foregut cysts (CFCs) are rare congenital lesions derived from remnants of the primitive foregut, which gives rise to the respiratory and upper gastrointestinal tracts. While typically found above the diaphragm, they can rarely appear in subdiaphragmatic organs like the liver and pancreas [1]. Their presence in the gallbladder is extremely rare due to its distinct embryologic origin [2]. To date, only 17 cases have been reported. We present the 18th case worldwide—the first in Palestine and the second in the Middle East [1, 3]. Given their rarity and non-specific imaging features, gallbladder CFCs are usually discovered incidentally. This report aims to improve recognition and support accurate diagnosis and documentation of this unusual lesion.
Case report
Presentation: A 34-year-old multiparous woman (G5 P4 A1) with no history of chronic illness or regular medication use presented to the emergency department with acute left flank pain of 3 h duration. She denied fever, chills, dysuria, hematuria, nausea, or vomiting. On examination, she was alert, oriented, and hemodynamically stable, with localized tenderness over the left flank. Cardiopulmonary, neurological, and musculoskeletal examinations were unremarkable. Laboratory investigations—including complete blood count, urinalysis, and serum creatinine—were within normal ranges.
Imaging findings: A non-contrast computed tomography (CT) scan of the abdomen revealed a mild left hydroureteronephrosis caused by a distal obstructive ureteric stone. Incidentally, the scan showed a focal thickening of the gallbladder fundus wall (Fig. 1). Correlation with abdominal ultrasound identified a well-defined 7 mm cystic lesion within the gallbladder wall (Fig. 2). The liver, spleen, and other abdominal organs appeared normal on CT.
Management: The patient was managed conservatively with intravenous fluids and analgesia during hospitalization.
Follow-up: She was discharged with advice for oral hydration and outpatient follow-up for both the ureteric stone and the incidental gallbladder lesion.
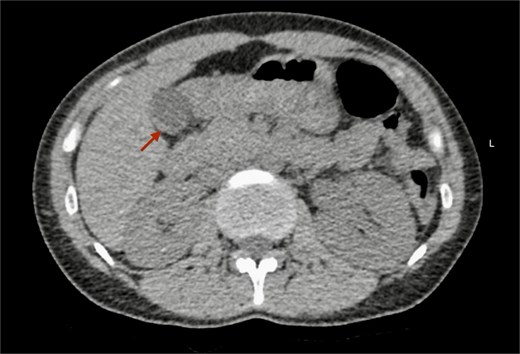
Non-contrast CT scan of the abdomen. The axial plane shows focal thickening of the gallbladder wall (arrow).
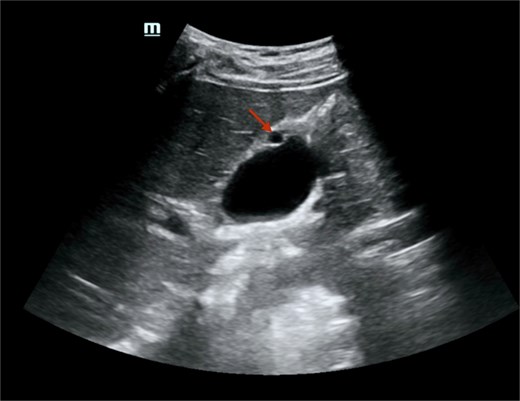
Abdominal ultrasound showed a well-defined, round, anechoic lesion within the gallbladder wall, measuring about 7 mm, likely representing a foregut cyst of the gallbladder. There was no peri-cholecystic edema, obvious shadowing stones, or increased wall thickness.
Discussion
Cystic lesions of the gallbladder are uncommon and may be congenital, acquired, or neoplastic. Among congenital types, ciliated cysts are benign lesions believed to originate from the anterior primitive gut [4]. During early embryogenesis, the primitive foregut forms in the third–fourth week of gestation and subsequently gives rise to a diverse set of endodermal derivatives. The ventral foregut develops into the pharynx, esophagus, stomach, proximal duodenum, as well as the hepatobiliary system (including the liver, intra/extrahepatic bile ducts, and gallbladder) and the ventral pancreatic bud. In contrast, the dorsal foregut contributes to the development of the respiratory tract and thyroid gland. Aberrant sequestration of epithelial rests from this developmental process is thought to underlie the formation of foregut cysts. The characteristic lining of ciliated pseudostratified columnar epithelium with underlying smooth muscle in these cysts reflects their embryonic origin and distinguishes them from true biliary epithelium [5].
These cysts are typically unilocular, lined by pseudostratified, ciliated, mucin-secreting columnar epithelium [6]. While they most commonly occur above the diaphragm, such as in the bronchial tree, esophagus, or mediastinum [3], they have also been reported below the diaphragm, particularly in the liver as ciliated hepatic foregut cysts, with over 100 documented cases. In contrast, gallbladder CFCs are extremely rare [7] and are thought to result from aberrant embryologic differentiation, leading to ectopic ciliated epithelium in sites like the liver, gallbladder, or pancreas [8].
According to Table 1, from 1995 to 2025, 18 cases of gallbladder CFCs were reported, and 1 case was excluded in our review table and analysis because it was different from the rest, as it was in the liver with some gallbladder involvement. So, our review showed a strong female predominance (78%). Most patients (14 cases) were symptomatic, predominantly with right upper quadrant pain, while 4 cases were detected incidentally. The neck of the gallbladder was the most frequent location (61%), followed by the body, fundus, and Calot’s triangle [9], possibly reflecting an embryologic tendency related to nearby biliary structures.
| Author . | Year . | Sex . | Age . | Symptoms . | Location . | Size . | Locularity . | Content . | Imaging . | Therapy . |
|---|---|---|---|---|---|---|---|---|---|---|
| Kakisubata | 1995 | M | 71 | Asymptomatic | Body | Unspecified | Unilocular | Unspecified | Ultrasound | Open |
| Nam | 2000 | F | 36 | Asymptomatic | Fundus | 15 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Hirono | 2002 | F | 43 | Asymptomatic | Neck | 25 mm | Unilocular | Mucus | US, CT, MRI | Open |
| Muraoka | 2003 | F | 37 | Asymptomatic | Body | 24 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Bulut | 2010 | F | 41 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | Unspecified | Laparoscopy |
| Tunçyürek S | 2013 | F | 42 | RUQ pain | Body | 7 mm | Unilocular | Mucus | US | Laparoscopy |
| Giakoumidis | 2014 | F | 29 | Epigastric pain | Neck | 30 mm | Unilocular | Mucus | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Hwang | 2015 | F | 39 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Lee | 2015 | M | 61 | RUQ pain | Body | 27 mm | Unilocular | Gelatinous | US, CT | Laparoscopy |
| Han | 2016 | F | 20 | RUQ pain | Neck | 16 mm | Unilocular | Mucus | US/CT (not described) | Unspecified |
| Agarwal | 2016 | M | 9 | RUQ pain, vomiting | Neck | 30 mm | Unilocular | Unspecified | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Farrugia | 2017 | M | 72 | RUQ pain, nausea | Neck | 45 mm | Unilocular | Unspecified | CT (adjacent to gallbladder) | Open |
| Wissem | 2017 | F | 34 | RUQ pain | Neck | 30 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Chikanori | 2021 | F | 50 | Asymptomatic | Neck | 17 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Baig and Priya | 2022 | F | 20 | RUQ pain | Calot’s Triangle | 50 mm | Unilocular | Mucus | US, CT with contrast | Laparoscopy |
| Ghanghoria et al. | 2023 | F | 30 | RUQ pain, vomiting | Neck | 25 mm | Unilocular | Mucus | US, MRCP | Laparoscopy |
| Present case | 2025 | F | 34 | Asymptomatic | Fundus | 7 mm | Unilocular | Unspecified | US, CT scan | Conservative |
| Author . | Year . | Sex . | Age . | Symptoms . | Location . | Size . | Locularity . | Content . | Imaging . | Therapy . |
|---|---|---|---|---|---|---|---|---|---|---|
| Kakisubata | 1995 | M | 71 | Asymptomatic | Body | Unspecified | Unilocular | Unspecified | Ultrasound | Open |
| Nam | 2000 | F | 36 | Asymptomatic | Fundus | 15 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Hirono | 2002 | F | 43 | Asymptomatic | Neck | 25 mm | Unilocular | Mucus | US, CT, MRI | Open |
| Muraoka | 2003 | F | 37 | Asymptomatic | Body | 24 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Bulut | 2010 | F | 41 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | Unspecified | Laparoscopy |
| Tunçyürek S | 2013 | F | 42 | RUQ pain | Body | 7 mm | Unilocular | Mucus | US | Laparoscopy |
| Giakoumidis | 2014 | F | 29 | Epigastric pain | Neck | 30 mm | Unilocular | Mucus | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Hwang | 2015 | F | 39 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Lee | 2015 | M | 61 | RUQ pain | Body | 27 mm | Unilocular | Gelatinous | US, CT | Laparoscopy |
| Han | 2016 | F | 20 | RUQ pain | Neck | 16 mm | Unilocular | Mucus | US/CT (not described) | Unspecified |
| Agarwal | 2016 | M | 9 | RUQ pain, vomiting | Neck | 30 mm | Unilocular | Unspecified | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Farrugia | 2017 | M | 72 | RUQ pain, nausea | Neck | 45 mm | Unilocular | Unspecified | CT (adjacent to gallbladder) | Open |
| Wissem | 2017 | F | 34 | RUQ pain | Neck | 30 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Chikanori | 2021 | F | 50 | Asymptomatic | Neck | 17 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Baig and Priya | 2022 | F | 20 | RUQ pain | Calot’s Triangle | 50 mm | Unilocular | Mucus | US, CT with contrast | Laparoscopy |
| Ghanghoria et al. | 2023 | F | 30 | RUQ pain, vomiting | Neck | 25 mm | Unilocular | Mucus | US, MRCP | Laparoscopy |
| Present case | 2025 | F | 34 | Asymptomatic | Fundus | 7 mm | Unilocular | Unspecified | US, CT scan | Conservative |
| Author . | Year . | Sex . | Age . | Symptoms . | Location . | Size . | Locularity . | Content . | Imaging . | Therapy . |
|---|---|---|---|---|---|---|---|---|---|---|
| Kakisubata | 1995 | M | 71 | Asymptomatic | Body | Unspecified | Unilocular | Unspecified | Ultrasound | Open |
| Nam | 2000 | F | 36 | Asymptomatic | Fundus | 15 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Hirono | 2002 | F | 43 | Asymptomatic | Neck | 25 mm | Unilocular | Mucus | US, CT, MRI | Open |
| Muraoka | 2003 | F | 37 | Asymptomatic | Body | 24 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Bulut | 2010 | F | 41 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | Unspecified | Laparoscopy |
| Tunçyürek S | 2013 | F | 42 | RUQ pain | Body | 7 mm | Unilocular | Mucus | US | Laparoscopy |
| Giakoumidis | 2014 | F | 29 | Epigastric pain | Neck | 30 mm | Unilocular | Mucus | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Hwang | 2015 | F | 39 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Lee | 2015 | M | 61 | RUQ pain | Body | 27 mm | Unilocular | Gelatinous | US, CT | Laparoscopy |
| Han | 2016 | F | 20 | RUQ pain | Neck | 16 mm | Unilocular | Mucus | US/CT (not described) | Unspecified |
| Agarwal | 2016 | M | 9 | RUQ pain, vomiting | Neck | 30 mm | Unilocular | Unspecified | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Farrugia | 2017 | M | 72 | RUQ pain, nausea | Neck | 45 mm | Unilocular | Unspecified | CT (adjacent to gallbladder) | Open |
| Wissem | 2017 | F | 34 | RUQ pain | Neck | 30 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Chikanori | 2021 | F | 50 | Asymptomatic | Neck | 17 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Baig and Priya | 2022 | F | 20 | RUQ pain | Calot’s Triangle | 50 mm | Unilocular | Mucus | US, CT with contrast | Laparoscopy |
| Ghanghoria et al. | 2023 | F | 30 | RUQ pain, vomiting | Neck | 25 mm | Unilocular | Mucus | US, MRCP | Laparoscopy |
| Present case | 2025 | F | 34 | Asymptomatic | Fundus | 7 mm | Unilocular | Unspecified | US, CT scan | Conservative |
| Author . | Year . | Sex . | Age . | Symptoms . | Location . | Size . | Locularity . | Content . | Imaging . | Therapy . |
|---|---|---|---|---|---|---|---|---|---|---|
| Kakisubata | 1995 | M | 71 | Asymptomatic | Body | Unspecified | Unilocular | Unspecified | Ultrasound | Open |
| Nam | 2000 | F | 36 | Asymptomatic | Fundus | 15 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Hirono | 2002 | F | 43 | Asymptomatic | Neck | 25 mm | Unilocular | Mucus | US, CT, MRI | Open |
| Muraoka | 2003 | F | 37 | Asymptomatic | Body | 24 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Bulut | 2010 | F | 41 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | Unspecified | Laparoscopy |
| Tunçyürek S | 2013 | F | 42 | RUQ pain | Body | 7 mm | Unilocular | Mucus | US | Laparoscopy |
| Giakoumidis | 2014 | F | 29 | Epigastric pain | Neck | 30 mm | Unilocular | Mucus | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Hwang | 2015 | F | 39 | RUQ pain | Neck | 35 mm | Unilocular | Mucus | US, CT | Laparoscopy |
| Lee | 2015 | M | 61 | RUQ pain | Body | 27 mm | Unilocular | Gelatinous | US, CT | Laparoscopy |
| Han | 2016 | F | 20 | RUQ pain | Neck | 16 mm | Unilocular | Mucus | US/CT (not described) | Unspecified |
| Agarwal | 2016 | M | 9 | RUQ pain, vomiting | Neck | 30 mm | Unilocular | Unspecified | US, MRI (adjacent to gallbladder) | Laparoscopy |
| Farrugia | 2017 | M | 72 | RUQ pain, nausea | Neck | 45 mm | Unilocular | Unspecified | CT (adjacent to gallbladder) | Open |
| Wissem | 2017 | F | 34 | RUQ pain | Neck | 30 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Chikanori | 2021 | F | 50 | Asymptomatic | Neck | 17 mm | Unilocular | Mucus | US, CT with contrast | Open |
| Baig and Priya | 2022 | F | 20 | RUQ pain | Calot’s Triangle | 50 mm | Unilocular | Mucus | US, CT with contrast | Laparoscopy |
| Ghanghoria et al. | 2023 | F | 30 | RUQ pain, vomiting | Neck | 25 mm | Unilocular | Mucus | US, MRCP | Laparoscopy |
| Present case | 2025 | F | 34 | Asymptomatic | Fundus | 7 mm | Unilocular | Unspecified | US, CT scan | Conservative |
Lesion sizes ranged from 7 to 50 mm. The smallest (7 mm) appeared in both the current 2025 case (fundus) and a 2013 report (body). The largest, a 50 mm cyst in Calot’s triangle, was documented in 2022. Patient ages were from 9 to 72 years, with a median of 36.5 years. Over half of the cases occurred in individuals aged 30–45, indicating a diagnostic concentration in mid-adulthood.
The imaging characteristics of our case a small-sized cystic lesion with clearly defined margins, and fundic location which suggest a CFC, a rare congenital lesion originating from embryonic foregut remnants. Although asymptomatic, its rarity and developmental origin justify ongoing monitoring, especially given the few cases reported globally.
The differential diagnosis of gallbladder cystic lesions is broad and includes congenital, acquired, and neoplastic entities. Congenital lesions encompass simple epithelial cysts, duplication cysts, mesothelial cysts, dermoid cysts, and CFCs, all of which are rare and often discovered incidentally [10]. Acquired cystic changes may result from dilated Rokitansky–Aschoff sinuses in adenomyomatosis, retention cysts secondary to obstruction, or inflammatory pseudocysts related to chronic cholecystitis [10]. Neoplastic cystic lesions include cystadenomas and cystadenocarcinomas, which may mimic benign cysts radiologically but carry malignant potential [11]. Other tumor-like conditions such as cholesterol polyps, xanthogranulomatous cholecystitis, and heterotopic tissue (gastric or pancreatic) should also be considered [12]. Distinguishing CFCs from these entities relies on careful correlation of imaging with histopathology, as the presence of pseudostratified ciliated columnar epithelium with smooth muscle wall is pathognomonic. Recognition of these features is crucial to avoid misdiagnosis and unnecessary surgical intervention, particularly in asymptomatic patients.
As a conclusion, CFCs of the gallbladder represent infrequent congenital anomalies, with limited cases described in the literature. This report presents the smallest documented lesion to date and the first case reported in Palestine. Its incidental discovery highlights the importance of considering such cysts in the differential diagnosis of gallbladder lesions. Thorough documentation contributes to improved recognition, enhances clinical awareness, and supports better-informed management of these uncommon entities.
Acknowledgements
The authors express their gratitude to the patient and their family for their significant contribution.
Author contributions
Qais Alnjoom and Ranya Abo Khalaf were the main contributors to the manuscript. Qais Alnjoom finalized the document, prepared it for submission, and is the corresponding author. Ranya Abo Khalaf contributed equally to writing the manuscript and was responsible for data collection. Mostafa Ibraheem wrote the introduction section, assisted in data collection, compiled the references, and prepared the abstract after the manuscript was completed. Hanin Shatrit and Moayad Nammourah, from the Diagnostic Radiology department, identified the case, initiated collaboration for the report, contributed to the literature review, and provided essential diagnostic data. Orwa Alfallah supervised all aspects of the work and approved each step prior to execution. All authors read and approved the final manuscript.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
The authors decline to receive any funding to make this work, and the authors did not have any funding supply.
Data availability
All data supporting the findings of this case report are included within the article. Other details or clarifications are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
The case was ethically approved to be published by the scientific research committee of Al-Ahli Hospital – Hebron; the approval is available for review upon the editor’s request. Informed consent was taken from the patient for taking information from her. The patient and their family were informed clearly that no added benefits would be given to them when they agree to participate in this research. Also, no harm will be caused to them in case of refusing participation.
A copy of the written consent is available for review upon the editor’s request.
Consent for publication
Informed consent was taken from the patient for the publication of this case report. A copy of the written consent is available for review upon the editor’s request.
References
Faure S, de Santa Barbara P. Molecular embryology of the foregut.



