-
PDF
- Split View
-
Views
-
Cite
Cite
Roberto Cunha, Nuno Coelho, Andreia Coelho, Pedro Monteiro, Alexandra Canedo, Endovascular approach for acute-on-chronic mesenteric ischemia: the holy grail for old and frail patients, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf907, https://doi.org/10.1093/jscr/rjaf907
Close - Share Icon Share
Abstract
Acute mesenteric ischemia is a rare but potentially fatal condition, with an estimated mortality rate of 80%. Early diagnosis and intervention are crucial. While laparotomy and open revascularization have traditionally been the standard approach, endovascular techniques are emerging as viable alternatives. We report the case of a frail 76-year-old patient with an acute exacerbation of chronic mesenteric ischemia who underwent successful endovascular revascularization of the superior mesenteric artery with percutaneous thrombectomy, avoiding the need for laparotomy. This case illustrates that an endovascular-first approach can be a feasible option for selected patients, with close monitoring to ensure timely surgical revision if necessary.
Introduction
Acute mesenteric ischemia (AMI) is a rare condition, accounting for ~0.1% of all hospital admissions, yet it carries an overall mortality rate as high as 80% [1]. It can have a thrombotic, embolic, or non-occlusive etiology. Due to the widespread of oral anticoagulation and the population aging, the proportion of embolic AMI has been decreasing in comparison to the thrombotic etiology [2].
Early diagnosis and prompt treatment are necessary to prevent bowel ischemia. Conventional surgical approach allows bowel inspection but is associated to high morbimortality. Endovascular techniques have emerged as potential alternatives to the management of these patients [3].
We present a case of AMI due to superior mesenteric artery (SMA) thrombosis, associated with distal embolization, treated with aspiration thrombectomy, and SMA stenting.
Case report
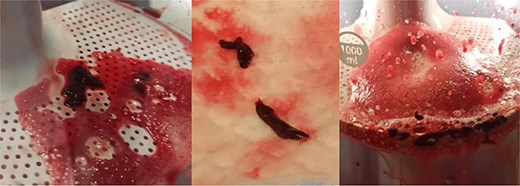
A 76-year-old female patient with a medical history of diabetes mellitus and cholecystectomy presented to the emergency department with a 7-month history of postprandial abdominal pain, food fear, and weight loss (25–30 kg). Over the past 3 days she referred symptom worsening to constant pain. On the physical examination, the abdomen was tender to palpation. Laboratory results revealed leukocytosis (13.700/μl), high C-reactive protein (23 mg/dl) and lactate 0.7 mmol/L. A previously performed computed tomography angiography (CTA) in context of a lithiasic cholecystitis revealed celiac trunk occlusion and pre-occlusive stenosis of the SMA ostium but the patient was not referred for a vascular surgery consultation. A CTA scan obtained in the emergency department revealed thrombotic occlusion of the SMA origin associated with distal embolization (Fig. 1A–C). In this context, the diagnosis of acute-on-chronic mesenteric ischemia was assumed, and the patient was proposed for urgent endovascular revascularization. A 7F (French) sheath was placed via percutaneous access in the left brachial artery, and SMA catheterization was performed using a triaxial system (sheath, MP catheter and Progreat® catheter). Diagnostic angiography confirmed the CT findings (Fig. 2A). Catheter-directed thrombolysis was first performed with a 5 ml bolus of alteplase, followed by percutaneous thrombectomy using the Penumbra® system (Fig. 2B), with retrieval of fresh thrombus (Fig. 3). Primary stenting of the SMA ostium was also performed using an Advanta® 6 × 39 mm stent with proximal flair, with an excellent imagological result (Fig. 4A and B). The postoperative course was uneventful, with significant improvement of symptoms and clinical status. A CTA prior to discharge revealed a patent stent with proper placement and no evidence of residual thrombus (Fig. 5A and B). The patient was discharged on the seventh postoperative day with apixaban 5 mg twice daily. Follow-up of the patient at 6 months revealed that the stent remained patent, with no reported abdominal complaints. The patient gained 15 kg at this point of follow-up.
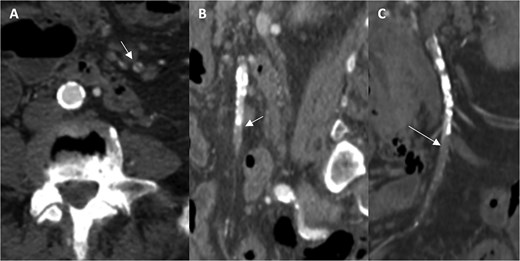
Computed tomography angiography images demonstrating occlusion of the superior mesenteric artery in the axial (A), sagittal (B), and coronal planes (C; arrows indicating the thrombus).
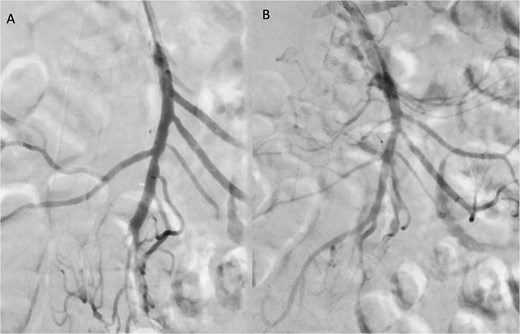
Angiographic images before (A) and after (B) thrombectomy of the superior mesenteric artery (SMA).
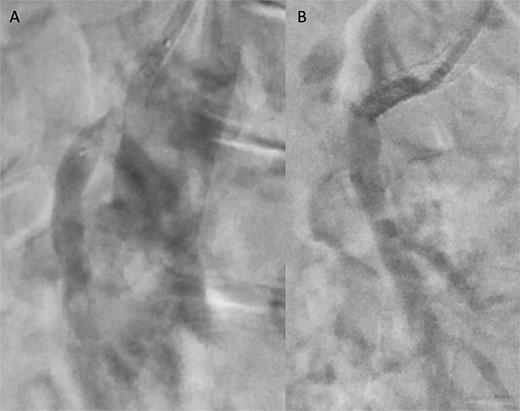
Angiographic images before (A) and after (B) primary stenting of SMA ostium using a 6 × 39 mm Advanta® stent with proximal flare.
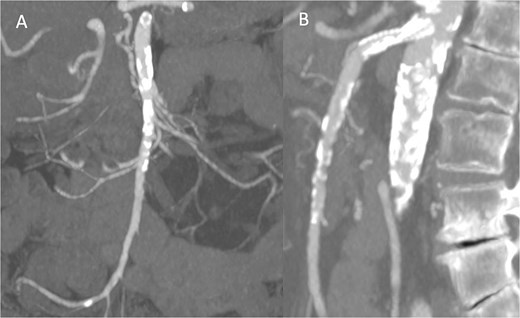
Pre-discharge follow-up CTA showing patent SMA and no complications, with coronal (A) and sagittal (B) images.
Discussion
The clinical diagnosis of acute-on-chronic mesenteric ischemia in its early phase is challenging due to the lack of a specific signs/symptoms in the clinical presentation. The most characteristic presentation is the sudden-onset abdominal pain disproportionate to physical examination findings, in a patient with previous chronic mesenteric ischemia symptoms. CTA has high sensitivity (93.3%) and specificity (95.9%) for the diagnosis of AMI, supporting the use of this technique as the first-line imaging method [3].
Endovascular therapy has been increasingly used as a revascularization strategy in AMI, however, it may not be applicable to all patients. The management of bowel infarction involves open bowel resection hence patients with signs of bowel necrosis or perforation on imaging, such as pneumatosis intestinalis or free intraperitoneal fluid, must undergo conventional surgery [4]. Also, CTA imaging has a low sensitivity for bowel suffering signs at an early stage.
Studies demonstrate improved 30-day mortality and decreased length of stay with endovascular strategies in the management of AMI. A study from the National Surgery Quality Improvement Program showed a 2.5-fold decrease in the risk of death associated with endovascular-first therapy [1]. Concerns regarding the endovascular strategy relate to the possibility of increasing the time to effective revascularization (in the event of failure) potentially delaying revascularization and exacerbating outcomes.
This case report is an example of a prompt and successful percutaneous intervention for an acute-on-chronic mesenteric ischemia event. The choice of endovascular treatment was based on the patient's fragility, low lactate levels, the absence of clinical signs of a board-like abdomen, and the lack of evidence of intestinal perforation or necrosis on the CTA. During the procedure, it was decided that percutaneous aspiration should be complemented by stenting of the SMA ostium to ensure greater durability of the treatment and to prevent similar phenomena in the future. Despite the success of the endovascular intervention, close monitoring of the patient’s abdominal evolution was maintained.
In conclusion, a minimally invasive strategy with a prompt endovascular-first approach is a good option for appropriately selected patients, if close monitoring is maintained and the need for bowel surgical assessment through laparoscopy or laparotomy is not excluded.
Acknowledgements
The authors would like to thank Dr. Luís Fernandes, Dr. Francisco Basílio, Dr. Marta Machado, Dr. Patrícia Carvalho, and Dr. Beatriz Guimarães for their valuable support and collaboration throughout the development of this study.
Conflict of interest statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical considerations
Our institution does not require ethical approval for reporting individual cases or case series.
Consent to participate and for publication
Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
This case report was conducted at Unidade Local de Saúde de Gaia e Espinho. The author has since moved to Hospital do Divino Espírito Santo.
References
- stents
- gastrointestinal tract vascular insufficiency
- thromboembolism
- vascular insufficiency of intestine, acute
- vascular insufficiency of intestine, chronic
- frail elderly
- laparotomy
- superior mesenteric artery
- repeat surgery
- second look surgery
- thrombectomy
- mortality
- revascularization
- early diagnosis
- exacerbation, acute
- aspiration thrombectomy



