-
PDF
- Split View
-
Views
-
Cite
Cite
Hao Chen, Chuanzheng Yin, Zifang Song, Palliative cholangiojejunostomy for refractory biliary obstruction in mucinous cholangiocarcinoma: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf718, https://doi.org/10.1093/jscr/rjaf718
Close - Share Icon Share
Abstract
Mucinous cholangiocarcinoma is a rare, aggressive biliary tract malignancy. Excessive mucin secretion causes diagnostic and therapeutic challenges. A 76-year-old male presented with painless progressive jaundice. Imaging showed cystic lesions with calcification in the right liver/hilum, intrahepatic bile duct dilation, and stones. Radical resection was deemed unfeasible due to insufficient predicted residual liver volume. Given the high risk of mucin-induced obstruction with conventional biliary drainage, palliative choledochojejunostomy was performed. Intraoperative findings revealed mucin and stones; frozen section pathology confirmed biliary mucinous adenocarcinoma. Postoperatively, bilirubin decreased significantly and biliary dilation improved. Mucinous cholangiocarcinoma management requires a multidisciplinary approach. When radical resection is contraindicated, palliative choledochojejunostomy effectively relieves mucin-related obstruction. Long-term outcomes depend on adjuvant therapy and surveillance; further, molecular research is needed to develop targeted therapies.
Introduction
Cholangiocarcinoma is a malignant tumor originating from the epithelial cells of the bile ducts [1, 2]. While mucin production is frequently observed in cholangiocarcinoma, the significant accumulation of mucin within the hepatic parenchyma and biliary tract is uncommon [3–5]. Mucinous cholangiocarcinoma (MC) is a rare variant of biliary malignancy characterized by the abundant secretion of mucin by tumor cells [6]. It was first described by Sugihara and Kojiro. Its exact incidence remains incompletely defined; however, among 102 cases of intrahepatic cholangiocarcinoma reported by Nakajima et al., only one was identified as MC [7]. The disease typically presents with non-specific symptoms such as biliary obstruction, jaundice, abdominal pain, and weight loss, posing significant diagnostic and therapeutic challenges.
Despite its low incidence, MC exhibits distinct biological behavior and response to treatment compared to other cholangiocarcinoma subtypes. Therefore, in-depth research into this entity holds significant clinical importance. This case report aims to elucidate the clinical characteristics and therapeutic strategies for MC through a detailed analysis of a patient’s clinical presentation, diagnostic process, treatment regimen, and prognostic outcome, thereby providing valuable insights for clinical practice.
Case presentation
A 76-year-old elderly male was admitted to our hospital due to jaundice (icterus of the skin and sclera) persisting for over one month. One month prior, he presented to a local hospital with jaundice. An upper abdominal contrast-enhanced magnetic resonance imaging (MRI) scan plus magnetic resonance cholangiopancreatography revealed a space-occupying lesion in the right hepatic lobe and hepatic hilum, suggestive of cystadenoma, with cholangiocarcinoma not excluded. Intra- and extrahepatic bile duct stones were noted with concomitant biliary duct dilation. The gallbladder was slightly enlarged, with an abnormal signal focus within its lumen; possible sludge stones, or inflammatory sediment (Fig. 1)? Tumor markers, including CA125, CA199, AFP, and PIVKA-II, were all within normal ranges. During his hospitalization there, supportive treatment including jaundice reduction, liver protection, and nutritional support was administered, but his symptoms showed no significant improvement.
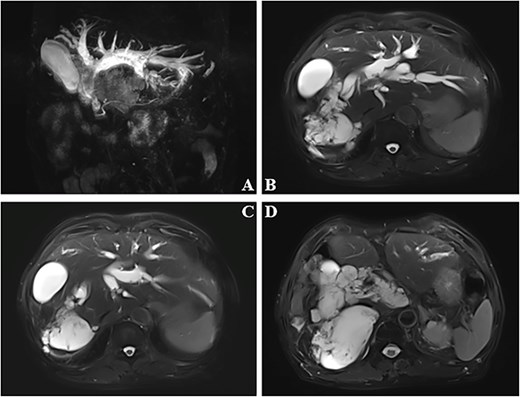
Dilated bile ducts (A). The mass shows high signal intensity on MRI T2-weighted images (B–D).
He was subsequently transferred to our hospital for further evaluation and management. Upon admission, the patient complained of dark urine and pruritus, but denied abdominal discomfort. Physical examination revealed an alert and cooperative patient with icteric skin and sclera. Cardiopulmonary examination was unremarkable. The abdomen was flat and soft, displaying an approximately 10-cm long old surgical scar (from a previous laparotomy for small bowel rupture due to a traffic accident). There was no tenderness or rebound tenderness. The liver and spleen were not palpable below the costal margin. Murphy’s sign was negative. Shifting dullness was absent. No lower extremity edema was noted. Laboratory investigations showed: total bilirubin: 59.9 μmol/l, direct bilirubin: 38.0 μmol/l, alanine aminotransferase: 89 U/l, aspartate aminotransferase: 111 U/l, alkaline phosphatase: 636 U/l, 5′-nucleotidase: 163 U/l, γ-glutamyl transferase: 859 U/l, and leucine aminopeptidase: 169 U/l. Contrast-enhanced computed tomography (CT) performed at our institution revealed multiple cystic low-density lesions with calcification in the right hepatic lobe and hepatic hilum, along with significant dilation of the intra- and extrahepatic bile ducts. The hilar bile ducts exhibited heterogeneous enhancement. The right hepatic vein and branches of the right portal vein were poorly visualized. Based on the clinical presentation and specialized investigations, a multidisciplinary team consultation favored the diagnosis of mucinous cystadenoma or carcinoma. After thorough discussion with the patient and his family regarding the condition, a decision was made for elective surgical resection. Preoperative assessment indicated insufficient residual liver volume, precluding tolerance for radical resection. Consequently, the primary objective shifted to relieving biliary obstruction. Pharmacological measures for jaundice reduction during hospitalization proved ineffective. Furthermore, existing studies suggest that T-tube placement, biliary stenting, and endoscopic nasobiliary drainage (ENBD) are often ineffective for this condition, as they tend to become obstructed by mucinous material within a short period, leading to recurrent biliary obstruction. After comprehensive consideration, a palliative cholangiojejunostomy was decided upon to resolve the biliary obstruction.
During surgery, extensive abdominal adhesions were observed. Fused lymph nodes were noted in the hepatic hilar region. The gallbladder was deformed due to compression by the dilated common bile duct and the lesion in the right hepatic lobe. The gallbladder was removed and the common bile duct was opened, revealing a large amount of mucoid material and stones spilling out. Intraoperative frozen section pathology confirmed the diagnosis of biliary mucinous adenocarcinoma (Fig. 2). After meticulous adhesiolysis, a left hepatic duct-jejunostomy was performed. Postoperatively, the patient’s bilirubin levels decreased significantly. Follow-up abdominal CT showed marked reduction in biliary duct dilation compared to previous imaging. Survival follow-up is ongoing.
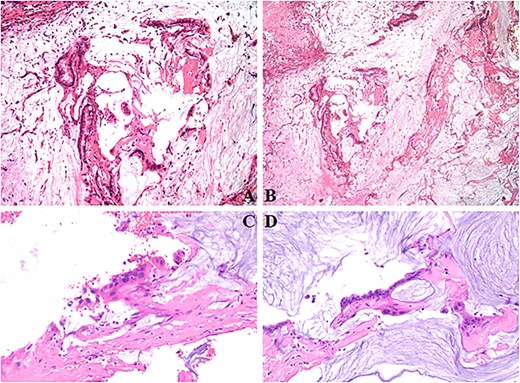
The tumor contains abundant mucin with floating adenocarcinoma cells (A–C). Chronic inflammation of the gallbladder without evidence of carcinoma involvement (D).
Discussion
MC is a rare subtype of cholangiocarcinoma characterized pathologically by tumor cells secreting abundant mucin, forming mucin pools or cystic structures [8, 9]. It frequently coexists with conditions such as biliary stones and chronic cholangitis. The clinical presentation lacks specificity, posing challenges for early diagnosis.
The clinical and imaging features of MC remain incompletely defined, with only limited case reports documented globally. On ultrasonography, lesions may appear as homogeneously echogenic masses resembling cavernous hemangiomas or demonstrate hyperechoic/anechoic patterns. However, due to frequent associations with calculi, inflammation, and biliary fibrosis, ultrasound exhibits limited diagnostic sensitivity and is primarily used for postoperative surveillance. CT imaging typically reveals multiple cystic masses around the lesion with irregularly thickened walls. Dynamic enhancement may show peripheral enhancement or non-enhancement. MRI demonstrates heterogeneous enhancement within the lesion. Conventional cholangiography techniques—such as endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography—provide minimal diagnostic value owing to abundant mucin obstructing contrast diffusion in the biliary system. Consequently, definitive diagnosis of MC predominantly relies on intraoperative frozen section or postoperative histopathological examination.
Surgical intervention remains the primary treatment modality for MC. The surgical approach should be tailored to the lesion location through individualized planning, aiming for maximal tumor resection, and establishment of patent biliary drainage. For patients ineligible for radical resection who experience recurrent cholangitis, ERCP with stenting and percutaneous transhepatic biliary drainage serve as primary palliative interventions for malignant biliary obstruction. However, Lin et al. documented a case where biliary obstruction recurred 16 months after endoscopic stent placement in MC [10]. Mizukami et al. reported a patient with mucinous biliary carcinoma who succumbed to rapidly progressive jaundice merely 3 weeks after ENBD [11]. Historical evidence indicates that stents, drainage tubes, and T-tubes frequently fail prematurely due to mucin-induced occlusion or displacement within dilated bile ducts [12], attributable to continuous mucin hypersecretion by the tumor. Consequently, our team implemented palliative cholangiojejunostomy to alleviate obstruction and enhance quality of life. This approach offers critical advantages. Creation of a wide anastomosis between dilated bile ducts and a Roux-en-Y jejunal limb enables simultaneous drainage of bile and viscous mucin, substantially reducing recurrence risk from mucin accumulation. The expansive jejunal lumen demonstrates superior resistance to mucin obstruction compared to narrow drains/stents, ensuring durable symptom relief. Surgical flexibility permits customized reconstruction adapted to tumor location and anatomical constraints. Postoperatively, bilirubin levels declined significantly, and survival follow-up remains ongoing.
Mucin represents an uncommon cause of malignant biliary obstruction, typically associated with mucin-producing pancreatic or biliary tumors. Most patients present with incidentally detected biliary obstruction that progresses to complications such as jaundice or cholangitis. Although imaging features of MC exhibit low specificity and cannot definitively diagnose mucin-induced obstruction, their presence should raise clinical suspicion for this entity.
Conclusions
Biliary mucinous adenocarcinoma is a rare malignant neoplasm characterized by both secretory properties and high aggressiveness. In this case, multidisciplinary evaluation and an individualized palliative surgical procedure successfully alleviated the biliary obstruction. However, the long-term prognosis remains dependent on postoperative adjuvant therapy and close surveillance. Future research necessitates further elucidation of its molecular mechanisms to advance the development of precision-based diagnostic and therapeutic approaches.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Funding
None declared.
References
Author notes
Hao Chen and Chuanzheng Yin contributed equally to this article and are co-first authors.



