-
PDF
- Split View
-
Views
-
Cite
Cite
Mohamed Amine Selmene, Mourad Zaraa, Hedi Annabi, Sabri Mahjoub, Surgical management of concomitant and delayed complex pelvic and acetabular fractures, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf760, https://doi.org/10.1093/jscr/rjaf760
Close - Share Icon Share
Abstract
Managing pelvic ring and acetabular fractures at a late stage of malunion or nonunion is a therapeutic challenge due to the complexity of both the surgical technique and strategy. We report the case of a 42-year-old male patient with pelvic and left hip trauma diagnosed 40 days postinjury, after a prolonged intensive care stay for severe chest trauma. Imaging revealed a Tile-AO B1-2 pelvic fracture with associated transverse–posterior wall acetabular fracture and femoral head dislocation. A two-stage surgery using multiple approaches was performed to remove callus and achieve reduction and fixation. The initial outcome was favorable. At 10 months, the patient developed left hip osteoarthritis and underwent primary total hip arthroplasty. At 36-month follow-up, he had a Harris Hip Score of 85, a Majeed score of 86, and had resumed near-normal daily activities. These complex cases require careful planning, with early surgical reduction being essential in displaced recent fractures.
Introduction
Fractures of the pelvic ring and acetabulum pose a therapeutic challenge in terms of surgical strategy, approaches, and fixation tools [1]. The anatomical complexity of this region and the vascular and nerve risks involved make their management more difficult. When these fractures are treated late, at the stage of malunion or nonunion, their management becomes more complex and difficult [2, 3].
We report the case of a patient who underwent open reduction and internal fixation (ORIF) of concomitant and delayed pelvic and acetabular fractures following a step-by-step surgical strategy.
Case report
This was a 42-year-old male patient with no previous medical history who was admitted to the intensive care unit for treatment of polytrauma: severe chest trauma and pelvic trauma. During his stay in intensive care, the patient developed a pulmonary infection complicated by septicemia, requiring prolonged antibiotic therapy and thereby contraindicating any internal surgical fixation. After hemodynamic and respiratory stabilization, he was transferred to our department 40 days after the trauma with the following injuries: an unstable pelvic ring fracture classified as Tile-AO B1-2 [4]: disjunction of the pubic symphysis, disjunction of the right sacroiliac joint, and an ipsilateral crescent fracture classified as Kumar-Day 2 [5], along with a transverse–posterior wall fracture of the left acetabulum associated with a posterior dislocation of the hip, which was initially reduced but remained unstable. Fixation was performed using a Hoffmann II external fixator applied to the iliac crests with poor reduction (Fig. 1). He presented with complete weakness of the left foot dorsiflexors, with preserved sensation and no urogenital or abdominal complications. ORIF was performed in two stages, 5 days apart. The first stage consisted of performing the first two windows of the ilioinguinal approach: the lateral window to access the sacroiliac joint and the middle window to access the lower part of the sacroiliac joint and remove the osteofibrous callus. A Pfannenstiel approach was used to remove the callus at the pubic symphysis and fix it with a plate. The patient was then placed in the prone position and a posterior approach to the right sacroiliac joint was performed to carry out the same procedures on the posterior part of this joint and to perform fixation using ilioiliac and iliosacral screws. The second stage of the operation involved acetabular surgery. Given the chronic dislocation of the left hip, an anterior approach to the hip was performed to remove the intra-articular fibrosis facilitating the subsequent reduction of the femoral head. A Kocher-Langenbeck approach was then performed to remove the callus, reduce the femoral head and fracture, and fix it with a plate (Fig. 2). Postoperatively, the patient retained neurological deficits. At 6 months, the patient was able to walk without assistance and had a Harris Hip Score (HHS) score of 80 and Majeed score of 75 [6, 7].
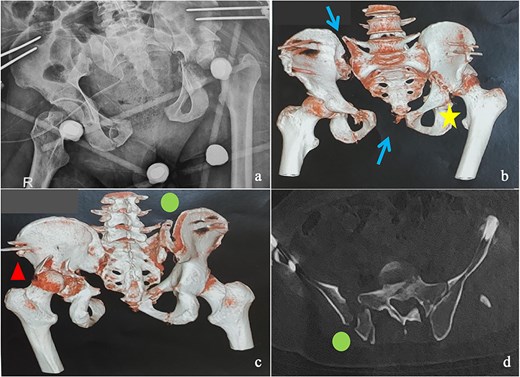
(a) Anteroposterior pelvic X-ray showing delayed pelvic and acetabular fractures. (b) Anterior view of the pelvis on 3D section: pubic symphysis disjunction and right sacroiliac dislocation (arrows), transverse component of the left acetabular fracture (star). (c) Posterior view of the pelvis on 3D section: right crescent fracture associated with right sacroiliac dislocation (circles), fracture of the posterior wall of the left acetabulum associated with posterior dislocation of the femoral head (triangle). (d) Axial section of the pelvic CT-scan: right crescent fracture Kumar-Day 2 (green arrow).
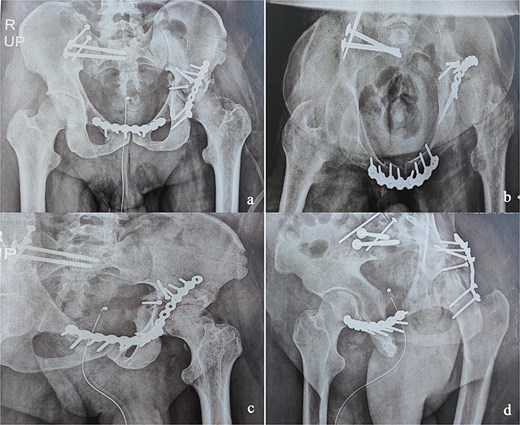
Immediate postoperative X-rays. (a) Anteroposterior pelvic X-ray. (b) Inlet view of the pelvis. (c) Alar oblique view of the pelvis. (d) Obturator oblique view of the pelvis.
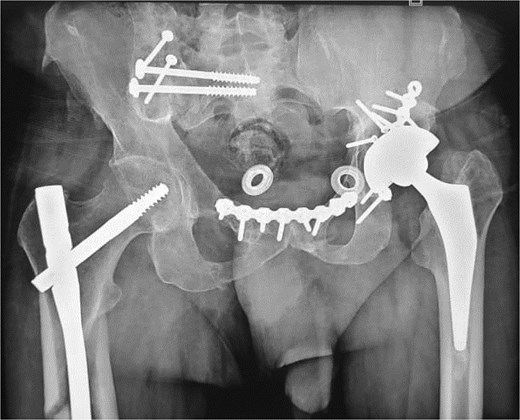
At the 10-month follow-up, the patient showed signs of left hip osteoarthritis with functional deterioration, for which a total ceramic-on-ceramic hip arthroplasty was performed, using a screw-fixed structural graft at the acetabulum (Fig. 3). At the final follow-up, 36 months postoperatively, the patient was walking unaided with the use of an anti-equinus splint on the left foot. The HHS was 85 and Majeed score was 86 [6, 7]. X-rays showed complete bone healing of all fractures and the acetabular graft. It should be noted that, during follow-up, the patient had a right femoral fracture that was successfully treated with a gamma nail (Fig. 4). Written informed consent were obtained from the patient.
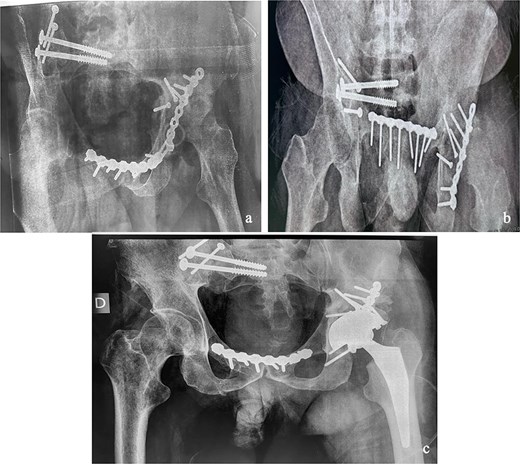
(a and b) Inlet and obturator oblique views showing a left hip osteoarthritis with subluxation of the femoral head. (c) Anteroposterior pelvic X-ray: left total hip arthroplasty, acetabular bone reconstruction with a screwed structural bone graft.
Discussion
Concomitant pelvic and acetabular fractures are rare and result from violent trauma and a complex injury mechanism [1]. The anatomical complexity and close neurovascular relationships in the pelvic and acetabular regions make ORIF surgery difficult and delicate, especially when performed at a late stage [8]. This type of surgery has low to medium patient satisfaction rates postoperatively but can result in significant improvement in terms of pain and function [3, 8].
With regard to the pelvis, the main indications for surgery are pain, walking difficulties, imbalance when standing or sitting, and urinary or sexual dysfunction [3]. The main objective at this level is to restore stability in order to allow continuity between the spine and the lower limbs [9].
These delayed situations are more complex to manage starting with Tile-AO B [4, 10] because they must involve both the anterior and posterior arches simultaneously [10]. This supports the fact that this surgery requires thorough preoperative planning to prepare for a long operation with multiple approaches allowing three-dimensional access to the callus and fracture, as was done in our patient [10, 11].
As for the acetabulum, this is also a rare and challenging situation [2]. The fracture line may have a predominant transverse component present in 58% of cases in a series by Li et al. of fresh concomitant fractures [1] and in our patient, causing added instability to the pelvic ring. Different approaches can be proposed to reduce and fix these delayed fractures. Apart from the classic ones, those associated with iatrogenic dislocation of the femoral head and osteotomy procedures, but also other more extensive ones are proposed in order to remove the callus and reduce the fracture [1, 12]. A combination of an anterior hip approach and a Kocher-Langenbeck approach was proposed for our patient in order to intra-articular fibrosis removal and three-dimensional control of the fracture.
Unlike pelvic fractures, acetabular malunions or delayed fractures that fail to respond to conservative treatment have a definitive solution: total hip arthroplasty. However, this procedure remains challenging due to bone loss, often requiring bone grafting and/or the use of revision implants [13–15]. Nonetheless, the primary objective remains the anatomical reduction and fixation of the fracture to facilitate any future total hip arthroplasty [14].
Conclusion
Surgical treatment of pelvic ring and acetabular fractures at a late stage, particularly in cases of malunion or nonunion, requires precise preoperative planning with a step-by-step surgical strategy in order to optimize results and reduce the complications that are common in this type of pathology.
Conflict of interest statement
We declare that we have no conflicts of interest.
Funding
None declared.



