-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Anklowitz, Jonathan Livezey, Samuel W Hoppe, Christopher W Mangieri, Byron Faler, The intra-abdominal zebra, paraduodenal hernias resulting in small bowel obstructions: a case series, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae534, https://doi.org/10.1093/jscr/rjae534
Close - Share Icon Share
Abstract
Paraduodenal hernias are a rare but important clinical entity, as their presentation can be life-threatening if not properly diagnosed and managed appropriately. Additionally, this entity is defined by a unique and complex congenital anatomical abnormality which dictates a specific treatment algorithm. Here we present the cases of three patients from our clinical experience who all presented with either acute or chronic small bowel obstructions secondary to paraduodenal hernias. Two were left-sided paraduoenal hernias and one was right-sided. All three patients were successfully managed with surgical intervention. An appreciation of paraduodenal hernias, including the defining anatomy and methods of surgical management, is important for the general surgeon.
Introduction
Paraduodenal hernias are a congenital anatomical abnormality of the small bowel mesentery resulting in internal hernia fossae that can cause both acute and chronic small bowel obstructions [1]. The topic of paraduodenal hernias is of importance to the general surgeon for two reasons. First, small bowel obstructions are one of the most common clinical entities encountered in general surgery. Thus, a general surgeon must be equipped to identify this specific type of bowel obstruction. Paraduodenal hernias affect males three times more frequently compared to females, but should be considered in the differential of any patient present with a small bowel obstruction [2]. Second, without knowledge of the anatomical abnormality involving paraduodenal hernias, a surgeon cannot adequately distinguish this unique cause of an obstructive internal hernia nor properly treat it surgically. This is of particular importance as a paraduodenal hernia is the most common congenital cause of an internal hernia and bowel necrosis is reported in up to 20% of cases [1, 3].
The first description of a paraduodenal hernia is credited to Václav Treitz in 1857 in which he describes various paraduodenal peritoneal folds [4]. He described these folds as providing recesses into which small bowel could become entrapped. As understanding of the condition has grown, two fundamental forms of the condition are now described, the right and left paraduodenal hernias. The distinction between these two anatomical entities is based upon the relationship of the peritoneal folds to the mesenteric vessels and the resulting anatomic position of the fossa thus created.
Left-sided paraduodenal hernias are most common, comprising 75% of cases [5]. The hernia defect consists of one peritoneal fold forming around the inferior mesenteric vein (IMV) and the ascending branch of the left colic artery. The resulting internal hernia space, known as Landzert’s fossa (Fig. 1), allows small bowel to herniate and become obstructed in a right-to-left fashion [6]. The congenital abnormality is illustrated in Fig. 1. The left-sided paraduodenal hernia is like the internal hernia created along the mesentery of the jejunojejunostomy during a Roux-en-Y gastric bypass if that mesenteric defect is not properly closed. As opposed to the right-sided paraduodenal hernia the left-sided internal hernia space is a smaller space behind the transverse mesocolon. Due to smaller space of left paraduodenal hernias, the incarcerated bowel is more susceptible to strangulation. The small bowel involved is typically the fourth portion of the duodenum and proximal jejunum however sometimes almost the entirety of the small bowel to include most of the ileum can be trapped within Landzert’s fossa [6].
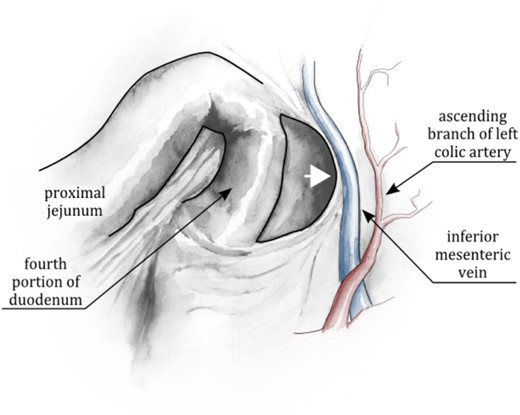
Left Paraduodenal Fossa, aka Landzert’s fossa. The fossa can be conceptualized as the recess formed by the tenting of the posterior peritoneum by the IMV, the ascending branch of the left colic artery, or both (as the positions of these vessels relative to one another are variable). This tenting creates a fold, or lip, behind which abdominal contents can herniate in a right-to-left fashion (arrow).
The less common right paraduodenal hernia is defined by herniation of abdominal contents into Waldeyer’s fossa (Fig. 2), which is formed by a peritoneal fold around the superior mesenteric artery (SMA) and vein at a location just inferolateral to the third portion of the duodenum (alternatively, the right colic vein and/or ileocolic artery have also been described as inhabiting this fold of peritoneum) [7]. Illustration of the right paraduodenal hernia is presented in Fig. 2. An alternate way to conceptualize this hernia is to imagine the left leaflet of the small bowel mesentery herniating to the right, thereby lifting the right leaflet and posterior parietal peritoneum off the posterior abdominal wall. The resulting internal hernia—which is effectively along the base of the proximal jejunal mesentery—allows herniation of abdominal contents in a left-to-right fashion. This places herniated bowel in a larger hernia sac posterior to the cecum, ascending colon, and even the proximal most portion of the transverse colon and corresponding mesocolon. Due to the larger internal hernia defect, there is a decreased risk of vascular compromise. Right paraduodenal hernias typically contain proximal jejunum and adjacent distal small bowel and contain on average a greater segment of bowel when compared to left paraduodenal hernias [8].
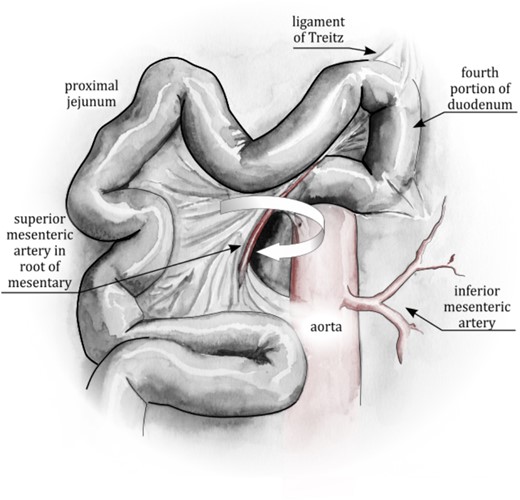
Right Paraduodenal Fossa, aka Waldeyer’s Fossa. The arrow represents the direction of rotation of the small bowel into the fossa. The arrow points into the fossa. The anterior/left edge of the fossa is formed by the tenting of the left mesenteric leaflet around the superior mesenteric vessels. The small bowel rotates around the superior mesenteric vessels to become entrapped behind the transverse mesocolon. This is effectively a partial reversal of mid-gut rotation, or, in some cases, a failure of complete rotation.
Bowel contained in both paraduodenal hernia subtypes is in a position posterior to even retroperitoneal organs (such as the ascending colon in the case of right paraduodenal hernia). Nevertheless, it is important to note that the small bowel is still contained within a hernia sack comprised of invaginated parietal peritoneum as is thus still technically intraperitoneal. Although the size of the hernia sac can be quite variable, especially in the right paraduodenal hernia, the congential mesenteric defect tends to be relatively small with a resultant constricting hernia neck. That constricting hernia neck puts patients at a significant risk for strangulation, thus necessitating prompt surgical reduction and repair [9].
We present here the cases and management of three patients who presented to our institution with paraduodenal hernias. We will conclude with a discussion of the operative technique generally used in the repair of paraduodenal hernias.
Case 1 [LA]
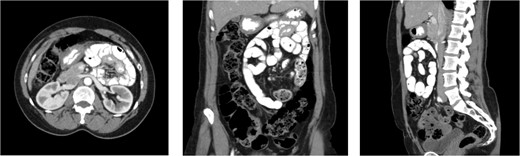
An 80-year-old female presented with symptoms of bowel obstruction. Her medical history was significant for hypertension, diabetes, and a total abdominal hysterectomy through a Pfannenstiel. She presented with ~1 day of colicky abdominal pain, nausea, vomiting, and denied previous episodes of similar symptoms. Physical exam revealed a soft but diffusely tender abdomen without peritoneal signs. Laboratory evaluation was significant for white blood cell count of 15 400 and a lactate of 3.6. A computed tomography (CT) scan of the abdomen was performed, which demonstrated a markedly dilated stomach and proximal small bowel, which was not the duodenum, in a retroperitoneal position. Images of the admission CT scan are depicted below (Fig. 3). Based on the concern for a paraduodenal hernia raised by imaging, as well as elevated white count and lactate, she was taken to the operating room for diagnostic laparoscopy which revealed that a majority of the jejunum was incarcerated within a left paraduodenal hernia. The bowel was reduced by gentle traction and found to be viable. The patient demonstrated evidence of chronic small bowel obstructions with several pulsion-type diverticula present due to recurrent episodes of occult obstruction. The mouth of the hernia defect, identified as Landzert’s fossa based upon its position at the base of the transverse mesocolon and nested between the proximal jejunum and the IMV, was closed with nonabsorbable suture. The operation was completed entirely laparoscopically with the patient experiencing no complications.
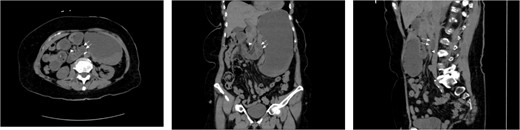
CT cross sectional images of Case 1, axial, coronal, and sagittal, respectively. Note the position of the dilated afferent small bowel (double arrow) posterior to the SMA (single arrowhead), thus confirming the retroperitoneal position of the entrapped bowel. Also note that while left paraduodenal hernias are typically described as existing in the left retroperitoneal position, there is no fixed midline barrier preventing their herniation to the across right of midline. In either case, the peritoneal defect, Landzert’s fossa, is the same with identical surrounding landmarks.
Case 2 [CG]
A 45-year-old morbidly obese male with a history significant for morbid obesity and atrial fibrillation presented with 1 day of abdominal distension, oral intake intolerance, nausea, and vomiting. The patient had no history of abdominal surgery. Physical exam revealed a soft, distended abdomen without peritoneal signs. Laboratory evaluation revealed normal blood cell counts and electrolytes. A CT-scan of the abdomen and pelvis with IV and PO contrast was performed which demonstrated proximal small bowel dilation and a significant amount of small bowel posterior to the SMA. A mesenteric swirl was also observed on CT imaging. The CT scan images are presented below (Fig. 4). Based on the concern for closed-loop obstruction and probable paraduodenal hernia, the patient was taken for diagnostic laparoscopy. During the procedure the patient was noted to have marked small bowel dilation, and most of the small bowel was found incarcerated behind the ascending mesocolon. The laparoscopic approach in this patient was significantly hindered by the excessive intraperitoneal fat present from his morbidly obese state. The procedure was converted to an upper midline laparotomy which facilitated complete reduction of the hernia and evaluation of the incarcerated bowel. Post-reduction, the bowel was deemed well perfused and viable. The internal hernia defect was confirmed as Waldeyer’s fossa based upon its position between the SMA and the ligament of Treitz. The hernia sac was opened laterally by mobilizing the cecum and ascending colon, taking down the white line of Toldt and medializing the ascending colon and cecum. Appendectomy was performed. The operation was completed without complication and the patient recovered well.
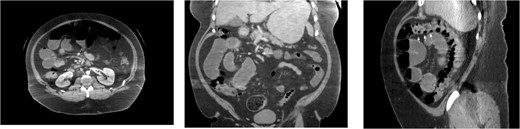
CT images for Case 2, axial, coronal, and sagittal, respectively. Note the mesenteric swirl (arrows in axial and coronal images) around the SMA (single arrowhead in axial and coronal images). This represents the posterior torsion of the small bowel mesentery as it courses into Waldeyer’s fossa toward the right retroperitoneum. The resulting dilated small bowel can be seen in the right upper quadrant. Also note the anterior course of the proximal transverse colon (three arrowheads in the sagittal cross-section) as it has been pushed toward the anterior abdomen due to the significant mass of dilated small bowel which is now posterior to its mesentery.
Case 3 [OS]
A 59-year-old female presented to our clinic with 10 years of vague episodic abdominal pain without prandial association. These episodes varied in severity, were self-limiting, and were not provoked by any identifiable factor. Her history was significant for asthma, GERD, and previous abdominal hysterectomy. The patient’s abdominal exam revealed only a Pfannenstiel scar but no tenderness, hernia, or palpable mass. The patient did not endorse any active symptoms in clinic. The patient underwent a CT scan of the abdomen and pelvis with IV and PO contrast which demonstrated small bowel loops in the right upper quadrant suspicious for herniation into a left paraduodenal space. Outpatient CT scan images can be found below (Fig. 5). The patient was scheduled for a diagnostic laparoscopy to evaluate for a paraduodenal hernia. Dense and extensive adhesive disease necessitated conversion to an upper midline laparotomy. The patient was found to have a left-sided paraduodenal hernia with the entire jejunum contained within Landzert’s fossa but without any signs of active obstruction. Additionally, the patient was found to have malrotation of the large bowel. After successful reduction of the non-obstructed small bowel, the mesenteric defect was then closed with a running silk stitch and the nearby proximal jejunum tacked over the repair. The malrotated large bowel was also placed in its correct anatomical position. The remainder of the procedure was uncomplicated with the patient recovering well.
CT images for Case 3, axial, coronal, and sagittal, respectively. The isolation of the contrast-filled small bowel can be appreciated in the right upper quadrant, representing bowel entrapped within the left paraduodenal hernia.
Discussion
As demonstrated above, the identification of a paraduodenal hernia can be challenging due to the unusual anatomy involved. Nevertheless, once identified, the management of the condition is relatively straightforward.
In the case of a left paraduodenal hernia, reduction of the bowel and assessment of viability is followed by a simple stitch closure of the internal hernia mesenteric defect at the opening of Landzert’s fossa [8]. That repair is akin to the closure of the jejunojejunostomy mesenteric defect closure in a laparoscopic gastric bypass procedure. The greatest challenge involved in the closure of a left paraduodenal hernia is avoiding the mesenteric vessels, particularly the IMV, contained in the peritoneal fold of the hernia. Fortunately, the mesenteric vessels are easily identified and protected during the closure.
In the case of a right paraduodenal hernia, the principle of management is not reduction, but rather release of the hernia space [10]. Although reduction of the herniated bowel is possible, the typically large amount of small bowel entrapped in the hernia makes release of the hernia-space the more straightforward, and thusly preferred, option. Additionally, the proximal SMA is either near the opening of Waldeyer’s fossa or even compromises a portion of the hernia neck rendering it easily injured if closure of the defect is attempted. We propose the more prudent repair approach is simply to convert the incarcerating hernia space into an open space that communicates with the peritoneal cavity. To accomplish this, the cecum and ascending colon are mobilized medially by releasing the white line of Toldt, as one would do in a lateral to medial dissection for a colectomy. In so doing, the hernia sac is entered, and the small bowel is again placed in an appropriate intraperitoneal location, albeit now right of the ascending colon, which is left in a medialized, yet still functional, position. This opens what is usually a very tight hernia space, thereby mitigating the risk of strangulation.
Paraduodenal hernia repairs use relatively straightforward surgical maneuvers that are found in the techniques of many other surgeries. Furthermore, these maneuvers are well described as laparoscopic techniques. We therefore propose that the laparoscopic approach is the technique of choice. That approach utilizes common techniques familiar to most laparoscopic surgeons. Patients benefit from the minimally invasive nature of the procedure. Lastly, laparoscopy affords superior visualization of atypical anatomy involved which is perhaps the most significant challenge involved in this pathology.
While we believe most paraduodenal hernias can be treated laparoscopically, the procedure can be technically demanding. Particularly when concomitant congenital abnormalities are present, such as - malrotation described in case 3. In those cases the operative technique is of course dictated by the unique challenges of the other abnormalities, perspicuity of laparoscopic visualization, and operative skill combined with surgical judgment of the treating surgeon.
In summary, we present three patients with bowel obstruction due to paraduodenal hernias as well as their successful surgical management. We propose laparoscopy as the ideal management approach of this condition and suggest that an open approach be utilized only after an unsuccessful laparoscopic attempt.
Conflict of interest statement
None declared.
The Dwight David Eisenhower Army Medical Center Institutional Review Board deemed this case series exempt from review.
Written informed consent has been obtained from the patients for publication of the case series and accompanying images.
The views expressed are those of the authors and do not reflect the official policy or position of the Army, the Department of Defense, or the US government.
Funding
None declared.



